RED EYE DIAGNOSIS
Practical Red Eye Problem-Solving
A look at potential causes of red eye in contact lens wearers and non-wearers.
By Thomas G. Quinn, OD, MS, FAAO
A red eye is a red flag—a classic sign of inflammation that alerts us that something is wrong and requires our attention. Many patients presenting with red eye are squeezed into an already packed schedule. The challenge to quickly make the proper diagnosis can be compounded if a patient is a contact lens wearer. What processes can we employ to identify the problem efficiently and treat it effectively?
Is There a Question?
Ocular redness can be due to a host of possible causes, some contact lens-related, some not (Table 1). One of the best tools to help get us to the source is a good history. One study in a hospital emergency department explored what tools were most instrumental in making the proper diagnosis (Paley et al, 2011). For both senior residents (four years in practice) and experienced clinicians (greater than 20 years), a good case history was found to be among the most valuable tools, superseded only by a combined case history and physical examination (Table 2). While imaging studies can obviously provide valuable information, it is interesting to note that, at least in this study, they ranked fairly low in diagnostic value compared to simply asking the right questions and being a good listener.
|
* Contact lens wear * Non-contact lens-related conjunctivitis ○ Bacterial ○ Viral ○ Allergic * Dryness * Environmental irritants ○ Smoke ○ Dust ○ Pool chlorine |
| Residents | Experienced Clinicians | |
|---|---|---|
| History (Hx) alone | 19.8 | 19.3 |
| Physical examination alone | 0.8 | 0.5 |
| Basic tests alone | 1.1 | 1.3 |
| Hx + Physical examination | 39.5 | 38.6 |
| Hx + Basic tests | 14.7 | 14.7 |
| Hx + Physical exam + Basic tests | 16.9 | 18.5 |
| Imaging studies | 6.5 | 6.1 |
How do you conduct a good case history? Although often viewed by clinicians as a headache and yet another demand placed upon them by the “big brother” healthcare system, the history of present illness (HPI) is a wonderful tool to employ (Table 3). Let’s walk through some of the key parts of an HPI and discuss how it helps us quickly arrive at the proper diagnosis of a red eye.
| Element | Explanation |
|---|---|
| Location | Where is the problem? |
| Duration | How long has the problem been there? |
| Severity | Is the pain minor, moderate, or severe? |
| Quality | Is it itchy, gritty, burning, etc.? |
| Context | How did the symptoms begin? (New patient) |
| Are your symptoms better or worse than at the last visit? (Returning patient) | |
| Modifying factors | What makes it better? |
| Associated signs and symptoms | Is there any mattering, swelling, etc.? |
| Timing | When do your symptoms occur? |
Location, Location, Location
When patients report with red eye complaints, they are usually noticing injection of the bulbar conjunctiva. Are both eyes red, or just one? Bilateral injection suggests a systemic or environmental cause, such as dry eyes, seasonal allergies, or contact lens solution sensitivity. Unilateral redness suggests exposure of only one eye to an irritant or a unilateral mechanical or inflammatory issue.
Before pulling up the slit lamp biomicroscope, sit back and look at the patient carefully. Note whether injection is generalized or focused in a particular area. Paralimbal injection may suggest anterior chamber inflammation. Redness in the aperture only may suggest dry eyes (Figures 1 and 2). A sectoral area of injection can help direct you to what area of the ocular surface to scrutinize closely.
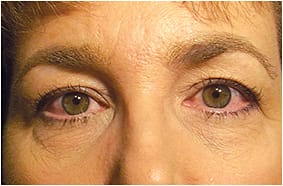
Figure 1. Injection in aperture from dry eyes.

Figure 2. Relative lack of injection superiorly in a dry eye patient.
Redness in areas other than the bulbar region can elicit a “red eye” complaint. Common areas include the surface of the eyelid, the eyelid margins (Figure 3), or even the palpebral conjunctiva. Allow redness of the eyelid margin to prompt you to study the lashes as well as the meibomian gland openings (Figure 4) and their expression. Meibomian gland dysfunction (MGD) will often also have associated generalized bulbar injection. Take care to not let the bulbar injection distract you from examining the eyelids closely.

Figure 3. Red eyelid margin with meibomian gland dysfunction.

Figure 4. Oil cap at lid margin.
Some patients present reporting redness of the inside of the lower eyelids. In such cases, be on the lookout for patient-induced mechanical irritation from repeated wiping of this area and “fishing” out mucus. Everting the lids will assist you in understanding whether both the upper and lower palpebral conjunctival tissue is involved. Consider everting the superior tarsal plate on all patients complaining of redness and ocular discomfort. This is particularly important for patients who have both a history of allergy and who are wearing reusable contact lenses, particularly if the lenses are worn on an extended wear basis.
The Quality Question
Redness is often accompanied by other symptoms. Ask patients to describe the quality of their symptoms. Patients reporting “itching” are often suffering from allergies, whereas those complaining of “burning” often suffer from dry eyes—but not always. How can you be sure?
Feeling the Itch Itching of both eyes, particularly if it is most intense nasally, is likely due to allergy. The focus in the nasal area is due to the allergens in the tear film accumulating in this area as they are washed from the ocular surface with the blink and pushed toward the nasal puncta for drainage.
I have come to appreciate that many patients complaining of itchy eyes are really reporting itchy eyelids. I have found that asking, “Is it your eye or your eyelid that itches?” early in the conversation has been immensely helpful in taking me in the right diagnostic direction.
When the source of the itch is the eyelid margin, simple eyelid hygiene (lid scrubs) often provides relief. Also available now are eyelid treatments incorporating ingredients that actively combat infection and inflammation. Examples include 4-terpineol, the active ingredient in tea tree oil, and hypochlorous acid, a non-antibiotic anti-infective that works by attacking essential proteins on bacterial membranes.
Itchy eyelid margins should prompt you to examine this area and express the meibomian glands (Figure 5). MGD is “a chronic, diffuse abnormality of the meibomian glands, commonly characterized by terminal duct obstruction and/or qualitative/quantitative changes in the glandular secretion” (Nichols et al, 2011). If the secretion is cloudy or thick (i.e., toothpaste), consider hot compresses, followed by milking of the glands. Other treatment strategies include lubricating eye drops, topical azithromycin or anti-inflammatory drops such as cyclosporine or loteprednol, omega-3 supplements, and tetracycline-derivative oral medication.

Figure 5. Matter in expression from meibomian glands.
When? Ask patients who have itchy eyes when symptoms occur. Seasonal complaints obviously point to seasonal allergies, but year-round itching does not rule out an allergic etiology. The patient may be sensitive to offending agents that are ever present, such as dust mites.
Patients reporting itch after working on the computer may be suffering from ocular surface dryness. If rubbing helps, this is a further indication of dryness because rubbing expresses oils and spreads tears across the ocular surface. If rubbing makes the itching worse, allergy is likely the culprit because rubbing breaks open mast cells and releases the irritants that cause an allergic reaction.
Burn Notice As stated earlier, complaints of burning eyes are likely due to ocular surface dryness, particularly if both eyes are involved and it is exacerbated by reading or computer use. Again, rubbing the eyes will often relieve burning if dryness is the culprit. Bulbar conjunctival staining with lissamine green can confirm a diagnosis of dry eye (Figure 6).

Figure 6. Lissamine green staining of the bulbar conjunctiva in a dry eye patient.
If burning occurs shortly after contact lens application, patients may have sensitivity to the contact lens storage solution, or they may have transferred lotion or perfume from their fingers to the lens surface. If you suspect that the culprit may be a foreign substance, but the patient denies it, ask about hand soap. Many commercially available hand soaps contain common irritants.
Associated Clinical Signs and Symptoms
Ask red eye patients about mattering (mucus), watering, and light sensitivity. If mattering is reported, ask about the quality of the matter. A white, stringy discharge suggests an allergic etiology, whereas a greenish, globular character suggests infection. Infection is also likely to be the cause if the discharge is sufficient such that the eyes have to be pried open upon waking in the morning.
A watery red eye may be viral in origin, particularly if the patient has a history of a recent head or chest cold. If the watering is exacerbated by cold air, computer work, or reading, it may be another sign of dry eyes.
Photophobia suggests anterior chamber involvement, which could be secondary to corneal irritation; therefore, always look for corneal compromise in these cases (Figure 7).

Figure 7. Corneal staining in a dry eye patient.
Are Contact Lenses the Cause?
One of the best ways to determine whether a red eye is related to contact lens wear is to explore the impact of modifying factors. Simply ask, “Do your symptoms get worse when you wear your contact lenses?” and “Do your symptoms get better when you remove your contact lenses?” If the answer to either of these questions is affirmative, contact lenses are probably contributory.
Another potentially insightful question is to ask about eye redness on waking. If redness tends to be worse on waking for patients who do not sleep in their contact lenses, the lenses are unlikely to be the primary cause of irritation. Conversely, contact lenses are high on the suspect list if redness is worse on waking for those sleeping in their lenses.
Contact Lens Causes of Red Eye
Hypoxia Hypoxia has been shown to lead to limbal hyperemia (Papas et al, 1997). Suspect a hypoxic etiology, particularly for red eye patients wearing low-oxygen-transmitting lenses for long hours, especially if they have a higher prescription resulting in a thicker lens. An added factor may be patients’ individual corneal oxygen requirement, which has been shown to vary in the population (Mueller et al, 2001; Quinn and Schoessler, 1984; Larke et al, 1981). Other clinical signs that lead to a likely hypoxic etiology for red eye include corneal neovascularization (Dumbleton et al, 2001) (Figure 8), corneal microcysts (Keay et al, 2000), and a steady increase in myopia over time, referred to as myopic creep (Dumbleton et al, 1999).

Figure 8. Corneal neovascularization from extended wear of a low-Dk soft contact lens.
Mechanical/Allergic Mechanical causes of contact lens red eye usually present unilaterally or asymmetrically. Lens damage is a common culprit. An infrequent cause is a superior epithelial arcuate lesion (SEAL). Found on the superior cornea, SEALs are thought to result from chafing of the peripheral cornea by the posterior contact lens surface. Tight overlying eyelid pressure and a high-modulus contact lens material are thought to predispose a patient to this condition (Holden, 2001). SEALs are often asymptomatic, so be sure to lift the upper lid and examine the superior cornea in all contact lens wearers reporting a red eye.
Contact Lens-Induced Papillary Conjunctivitis Contact lens-induced papillary conjunctivitis (CLPC), sometimes interchangeably referred to as giant papillary conjunctivitis (GPC), is an inflammation of the palpebral conjunctiva. It is thought to be a result of mechanical irritation from a poor lens edge design or deposits on the lens surface. These surface deposits are also thought to trigger an allergic/hypersensitivity response.
CLPC is more likely to occur with wear of silicone hydrogel lens materials and with extended lens wear. It is less likely to be a problem with daily disposable lenses (Sankaridurg et al, 2001), so switching patients to this wearing modality can be used as a treatment strategy. Topical steroids or antihistamine/mast cell stabilizers can also be quite helpful in quieting this condition.
Non-Infectious Corneal Inflammatory Events Corneal inflammatory, or infiltrative, events (CIEs) have been classified in the following way (Sweeney et al, 2003):
• Serious and symptomatic (e.g., microbial keratitis [MK])
• Clinically significant and symptomatic (e.g., contact lens-induced peripheral ulcer, contact lens-induced acute red eye, infiltrative keratitis)
• Clinically non-significant and asymptomatic (e.g., asymptomatic infiltrative keratitis and asymptomatic infiltrates)
With a reported incidence of 26.7% (Szczotka-Flynn and Diaz, 2007), non-infectious CIEs are commonly encountered in clinical practice. Non-infectious CIEs tend to occur in the peripheral cornea, and the eyes are generally quieter compared to those that have infectious lesions. Although the vast majority of CIEs are non-infectious, some overlap in clinical signs and symptoms can occur, so approach all with suspicion.
Wagner and colleagues (2011) have found a greater risk for CIEs in contact lens wearers in late adolescence and early adulthood. They also found a higher incidence in patients wearing silicone hydrogel lenses. Other studies have found that wearing silicone hydrogel lenses leads to a two-times increase in the incidence of CIEs compared to those wearing hydrogel lenses (Szczotka-Flynn and Diaz, 2007; Radford et al, 2009). There is evidence suggesting that this may be associated with higher binding levels of bacteria to silicone hydrogel lens surfaces (Subbaraman et al, 2011).
If surface cleanliness is important, you would expect that wear of a daily disposable contact lens would significantly reduce the likelihood of CIEs. This has, in fact, been found to be the case. One study found that the risk of CIEs decreased by 12.5 times when lenses are changed on a daily basis (Chalmers et al, 2012). This beneficial effect has been shown to occur for both hydrogel and silicone hydrogel daily disposable lens wearers (Chalmers et al, 2015).
Corneal Infection/Inflammation The incidence of MK has remained relatively unchanged over the past few decades, even with the introduction of silicone hydrogel lenses. The risk of MK is approximately five times greater for those wearing lenses on an extended wear basis and is estimated to be between 18 and 25.4 per every 10,000 wearers (Poggio et al, 1989; Schein et al, 2005; Stapleton et al, 2008).
There is also evidence suggesting that poor storage case hygiene can put patients at almost as much risk for MK as extended lens wear can (Szczotka-Flynn, 2009). It is now recommended that cases be cared for in the following way: discard old solution, rub case with clean fingers for at least five seconds, rinse with disinfecting solution, wipe dry with a clean cloth, and store (with lids off) upside down in a clean area (Wu et al, 2010). There is evidence to suggest that cases may develop significant contamination after two weeks of use (Lakkis et al, 2009). So, at minimum, monthly case replacement would be advisable. Of course, another option is to simply fit patients with daily disposable lenses, in which a storage case is not needed and therefore removed as a potential source of contamination.
A corneal lesion is most likely to be infectious (versus sterile) if it is more centrally located, is 2mm or greater in size, and, in general, causes a very “hot eye.” Approximately 90% of all MK is due to bacterial infection (Musa et al, 2010), in which case you would expect associated mucus production. However, some viral, parasitic, and immune-related stromal necrosis will not have this associated sign (Srinivasan et al, 2008), so absence of mucus does not rule out infection.
MK is an ocular emergency requiring aggressive therapy. In cases of bacterial ulcers, there is evidence that adding a topical steroid two to three days after starting antibiotic treatment reduces scarring, leading to improved visual outcomes (Ray et al, 2014). Consider co-managing MK patients with a corneal specialist, particularly if the lesion is central and may lead to permanent vision loss.
Contact Lens-Induced Peripheral Ulcer In 1998, Grant and associates coined the term “contact lens-induced peripheral ulcer (CLPU)” to describe small, round, peripheral infiltrates with an overlying absence of epithelium. CLPUs present unilaterally. They can be asymptomatic, but it is not unusual for them to be accompanied by mild discomfort. CLPUs result from colonization of gram-positive bacteria, particularly Staphylococcus species, on the contact lens surface; they are often associated with a recent history of overnight contact lens wear. Treatment includes temporary discontinuation of contact lens wear and close monitoring for the next 24 to 48 hours to ensure that the lesion is not, in fact, infectious. This concern leads many eyecare providers to often prescribe, as a precautionary measure, a broad-spectrum antibiotic until the epithelial lesion is healed.
Contact Lens Acute Red Eye Any patient who is sleeping in contact lenses and awakes with a unilateral, acute red eye with no, or minimal, corneal staining is likely suffering from contact lens acute red eye (CLARE). CLARE is an inflammatory response to the accumulation of gram-negative bacteria. Temporarily ceasing lens wear should result in significant resolution of ocular redness within a day or two. Again, when in doubt, prescribe a broad-spectrum antibiotic.
Infiltrative Keratitis (IK) Corneal infiltrates, which can be observed in both symptomatic and asymptomatic patients, are an accumulation of white blood cells in the epithelium or anterior stroma. They are a response to an inflammatory stimulus, which can include a wide array of possibilities. Figure 9 is the left eye of a patient who presented with complaints of a unilateral red eye with mild discomfort. Further examination found mild infiltrates in the right eye as well. Switching the patient from a multipurpose contact lens care system to a hydrogen peroxide-based system resolved the infiltrates (Figure 10).

Figure 9. Infiltrative keratitis associated with contact lens solution sensitivity.

Figure 10. Same eye as Figure 9 one week later with infiltrative keratitis resolved.
Listen, Then Look
Any time a patient presents with a red eye, even when squeezed into an already busy schedule, take a detailed history. It will be time well invested because it will streamline your physical examination, allowing you to more accurately diagnose and more effectively treat the patient. With keen listening and thoughtful observation, everybody wins. CLS
For references, please visit www.clspectrum.com/references and click on document #237.

| Dr. Quinn is in group practice in Athens, Ohio. He is an advisor to the GP Lens Institute and an area manager for Vision Source. He is an advisor or consultant to Alcon and B+L, has received research funding from Alcon, AMO, Allergan, and B+L, and has received lecture or authorship honoraria from Alcon, B+L, CooperVision, GPLI, SynergEyes, and STAPLE program. You can reach him at tgquinn5@gmail.com. |



