Contact Lens Case Reports
Bulging Graft? Consider a Scleral Lens
BY PATRICK J. CAROLINE, FAAO, & MARK P. ANDRÉ, FAAO

The majority of patients who have undergone corneal transplant surgery require some form of optical correction to optimize their visual acuity and to reestablish binocular function. This may include correction with glasses, refractive corneal surgery, or contact lenses.
Today, a wide variety of rigid, soft, and combination contact lens designs and materials are available for post-keratoplasty eyes. The choice of lens design is often influenced by the topography of the post-surgical cornea.
A Case of a Bulging Graft
Our patient is a 57-year-old male with a longstanding history of keratoconus. He underwent penetrating keratoplasty to his left eye at age 25; since that time, he has been unable to be fit successfully with a contact lens. The patient has functioned unilaterally using a corneal contact lens on his unoperated keratoconic right eye to achieve a visual acuity of 20/40.
Slit lamp examination of the patient’s left eye showed the graft to be clear and free of any vascularization. It was obvious that the graft had bulged significantly after surgery (Figure 1). The exact mechanisms responsible for a bulging corneal transplant remain unclear today. Some suggested theories include excessive postoperative intraocular pressure (IOP), inadequate tightening of the corneal sutures, and a lack of tissue rigidity in the donor cornea, often present in younger tissue. Our patient’s IOP was within normal limits in both eyes.

Figure 1. The patent’s left eye as viewed in profile.
Managing the Lens Fit
Figure 2 shows optical coherence tomography (OCT) images of the sagittal depth of the patient’s left eye (5,780 microns) as compared to a normal eye (3,735 microns). Because of the bulging graft, it was determined that a scleral lens would best serve the patient.
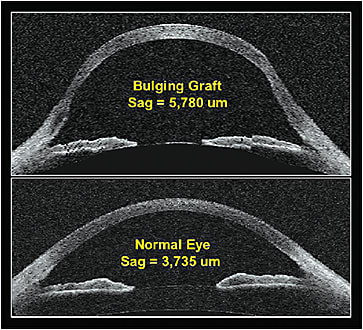
Figure 2. (A) An OCT image of the patient’s left eye with a sagittal depth of 5,780 microns, and (B) a normal eye with a sagittal depth of 3,735 microns.
The patient was diagnostically fitted in a lens with the following parameters: sagittal height 5,600µm, base curve radius 56.00D (6.03mm), power –17.25D, diameter 16.5mm, peripheral corneal clearance zone +1, limbal clearance zone +10, and a scleral landing zone of –2.
Figure 3 shows the final lens on the patient’s eye. He was able to wear the lens all day with excellent comfort and a visual acuity of 20/30. CLS
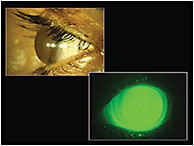
Figure 3. A white light and cobalt blue image of the patient’s scleral lens on-eye.
Patrick Caroline is an associate professor of optometry at Pacific University. He is also a consultant to Contamac. Mark André is an associate professor of optometry at Pacific University. He is also a consultant to CooperVision.



