Contact Lens Case Reports
A New Look at Scleral Shape
BY PATRICK J. CAROLINE, FAAO, & MARK P. ANDRÉ, FAAO

Today, we know that the human sclera is both asymmetrical and often surprisingly toric. The influence that this has had on scleral lens design for individual patients cannot be overstated. Three anterior segment imaging technologies have emerged capable of measuring the sclera in all eight principle meridians: anterior segment optical coherence tomography, profilometry techniques, and Scheimpflug imaging.
While many patients wearing scleral lenses enjoy excellent physical comfort, there is a subset who are unable to achieve adequate wearing time with (what appear to be) well-fitted scleral lenses. This problem can be either unilateral or bilateral.
Today, we believe the factors responsible for this intolerance include: 1) A neurologic hypersensitivity of the cornea, limbus, conjunctiva, and/or sclera; 2) Subtle design elements related to the array of junctions on the anterior and posterior lens surface; and 3) Subclinical anatomical anomalies in the unique scleral shape of the patient.
Mapping the Sclera
This month’s case involves a 32-year-old male who underwent bilateral LASIK in 2012 with significant postoperative symptoms of dry eyes. We refitted him into rotationally symmetric (spherical haptic) scleral lenses, and he was able to comfortably wear his left lens all day. However, he was never able to achieve adequate comfort with his right lens.
We performed scleral mapping of the two eyes with the sMap3D (Visionary Optics, manufactured by Precision Ocular Metrology, LLC) and discovered a subclinical scleral toricity of the right eye only. The sMap3D uses sodium fluorescein and projected pattern sequences to map the corneal and scleral surface out to a chord of 22mm (Figure 1). This is accomplished by measuring the ocular surface in three fields of gaze (Figure 2), after which the images are stitched together to form a single composite map. The cornea is displayed as a uniform red color when in the “scleral elevation” display.
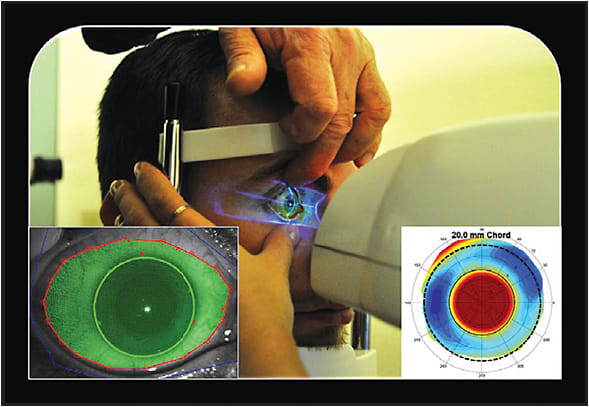
Figure 1. An sMap3D performed in primary gaze resulting in a 360º elevation display map of the sclera out to a chord of 22mm.
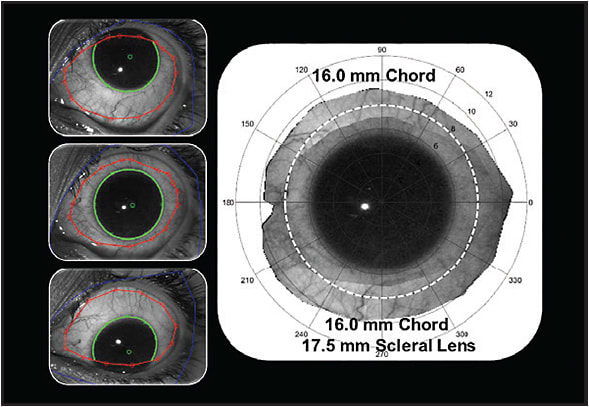
Figure 2. The subject looks in three fields of gaze (primary, up, and down), which are then stitched together to form a single composite of the anterior segment.
Figure 3 shows the elevation display of the patient’s right and left eyes. The red areas indicate where the sclera is “highest,” and the blue areas indicate where it is the “lowest.” Note the near-sphericity of the sclera on the left eye.
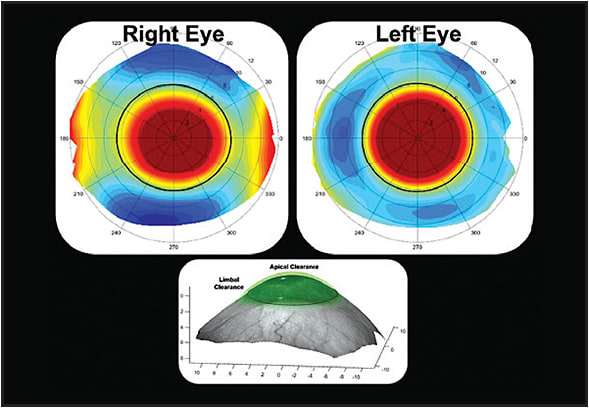
Figure 3. Scleral elevation display maps of our patient’s right and left eyes. Note the elevation differences in the toric right eye versus the near-spherical left eye.
The patient was subsequently fitted with a toric haptic scleral lens on his right eye, and his wearing time immediately improved from an uncomfortable six hours per day to comfortable all-day lens wear.
This case illustrates how new instrumentation can be used to recognize each patient’s unique asymmetrical and astigmatic scleral shape. CLS
Patrick Caroline is an associate professor of optometry at Pacific University. He is also a consultant to Contamac. Mark André is an associate professor of optometry at Pacific University. He is also a consultant for CooperVision.



