November 2016 Online Photo Diagnosis
By William Townsend, OD
Superior Limbic Keratoconjunctivitis
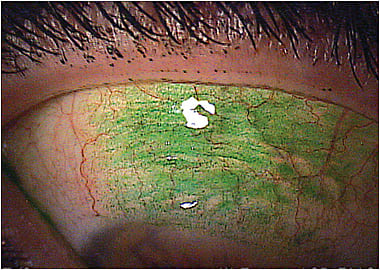
This 39-year-old female presented with foreign body sensation and irritation in her right eye, a recurring event in her 15-year history as our patient. On evaluation, we noted injection of the superior conjunctiva extending down to the limbus. There was minimal fluorescein staining of the affected area, but subsequent instillation of lissamine green resulted in the more intense staining pictured.
This patient suffers from chronic, recurring superior limbic keratoconjunctivitis (SLK), an inflammatory condition of the superior palpebral and bulbar conjunctiva. Theodore first described SPK in 1963; he reported a triad of signs including:
1. Papillary reaction of the superior palpebral conjunctiva
2. Superior bulbar conjunctival hyperemia
3. Superior superficial punctate keratoconjunctivitis1
SLK may also present with punctate keratopathy, filamentary keratitis, keratinization of the superior limbus, and discharge. Commonly reported symptoms include burning, redness, foreign body sensation, and photophobia.2
The precise pathophysiology of SPK has not been established, and it may actually be multifactorial.2 Cher proposed that SLK is caused by microtrauma resulting from repetitive abnormal rubbing of the tarsal and bulbar surfaces as well as rubbing between conjunctival stroma and sclera.3 He supported this concept with light and electron microscopy evaluation of these tissues. Histological findings included squamous metaplasia and edema of epithelium as well as stromal infiltrates with edema.
In addition to mechanical trauma, dry eye, localized inflammation, and Graves’ disease have been linked to SLK. A number of diverse therapies for SLK have been proposed and evaluated, including thermocautery, chemocautery, cryotherapy, conjunctival resection, punctal occlusion, autologous serum, topical cyclosporine A, vitamin A drops, topical nonsteroidal agents, bandage contact lenses, topical botulinum toxin, and topical steroids.4
In the case of our patient, we prescribed loteprednol etabonate ophthalmic gel 0.5% b.i.d. for one week and then tapered her dosing over the following week. Her signs and symptoms resolved. But, as is the case in many patients who have SLK, there is a strong likelihood that the condition will recur in the future.
References
1. Theodore FH. Superior limbic keratoconjunctivitis. Eye Ear Nose Throat Mon. 1963 Jan;42:25-28.
2. Nelson JD. Superior limbic keratoconjunctivitis (SLK). Eye. 1989;3(Pt 2):180-189.
3. Cher I. Superior limbic keratoconjunctivitis: multifactorial mechanical pathogenesis. Clin Exp Ophthalmol. 2000 Jun;28:181-184.
4. Fraunfelder FW. Liquid nitrogen cryotherapy of superior limbic keratoconjunctivitis. Am J Ophthalmol. 2009 Feb;147:234-238.



