Today in clincal practice, we often come across peculiar-looking corneal shapes for which we need to determine the etiology of the asymmetric or irregular astigmatism (Figure 1). In the late 1930s, Swiss ophthalmologist Marc Amsler (of Amsler Grid fame) coined the term forme fruste keratoconus to describe a subtle form of asymmetric corneal astigmatism that has topographical features that “mimic” those often seen in early forms of keratoconus, such as superior flattening and inferior steepening. The condition was further described by Duke-Elder in the 1960s.

Unlike a conical cornea (primary keratoconus), forme fruste keratoconus is characterized by the presence of: 1) a stable asymmetrical astigmatism that is non-progressive, 2) a corneal thickness that is normal and stable, and 3) no positive slit lamp signs of keratoconus.
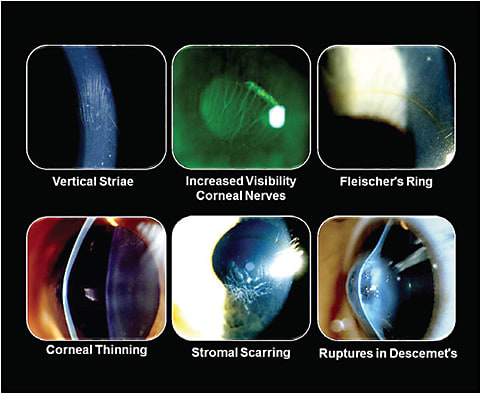
Our patient is a 32-year-old male referred to us from a local refractive surgery center with the diagnosis of possible keratoconus OD and OS. Our examination showed none of the early slit lamp findings of keratoconus, such as vertical or Vogt’s striae, Fleischer’s ring, or anterior stromal scars (Figure 2). However, corneal topography analysis showed an asymmetric corneal astigmatism in both eyes that is somewhat suspicious of early keratoconus (Figure 3). Corneal pachymetry with an optical coherence tomographer showed a normal corneal thickness throughout both corneas.

Don’t Jump to Conclusions
So does this patient have forme fruste keratoconus (as described by Amsler and Duke-Elder), or is this an early form of primary keratoconus? We believe that the answer is simple: we don’t know. Our concern is that, throughout the years, the term forme fruste keratoconus has somehow lost its original definition (that of Amsler and Duke-Elder) and has morphed into a term that is now used to describe any form of early keratoconus.
We truly believe that non-progressive, asymmetric (keratoconus-like) corneal topographies do indeed exist; we have had the pleasure of following such patients’ corneal topographies and corneal thicknesses for many, many years, and we have clearly documented exactly what Amsler and Duke-Elder described—no changes in corneal topography and no changes in corneal thickness.
Today, we believe that the “true” diagnosis of forme fruste keratoconus can be made only through a historical profile of the patient that clearly documents the non-progressive nature of the asymmetric corneal astigmatism and no changes in corneal thickness. Therefore, at the initial presentation of our patient, he might have forme fruste keratoconus or he might have early keratoconus; only time can clarify the diagnosis. CLS
For references, please visit www.clspectrum.com/references and click on document #261.





