Today’s contact lens practice is defined by fitting patients into different categories of lenses, whether they be soft, GP corneal, hybrid, or scleral lenses. The overall contact lens marketplace is dominated by soft contact lenses, and the majority of those lenses are molded in a mass-production fashion in an attempt to satisfy the majority of the patient population while limiting the existing parameter availability within the constraints of manufacturing capabilities and storage capacities.
Eyecare practitioners are not able to satisfy all contact lens patients with the standard molded soft contact lenses that dominate the marketplace. What can be difficult as an eyecare practitioner is recognizing when patients may be better served by a soft contact lens that has parameter(s) (base curve, power, overall diameter, etc.) that are outside of/beyond the molded soft contact lens parameter range.
What can be an even greater challenge is determining how to arrive at an appropriate custom soft lens prescription to satisfy patients’ needs; as soon as a custom soft lens is decided upon, the parameters are essentially limitless in variability for power, base curve, diameter, thickness, material, and optic zone size, among other things. What will be explored in this article are the indications for custom soft contact lenses and a stepwise process for determining the features needed in a custom soft contact lens.
INDICATIONS
Determining whether a custom soft lens design is indicated begins with an evaluation of patients’ astigmatism and identifying whether they have regular or irregular astigmatism. Patients who have regular astigmatism with a cylinder correction need beyond –2.25D at the plane of the cornea are often those who are most commonly fitted into custom soft lenses, as patients who have a cylinder error of –2.25D or below at the corneal plane have numerous molded soft lens options.
However, patients who have regular astigmatism less than –2.25D at the corneal plane may also be candidates for custom soft lenses based on the size and shape of their eye, namely, how large (visible iris diameter [VID]) or how flat or steep (central corneal curvature, keratometry value) their cornea is. VID and corneal curvature are the anatomical features that contribute to the overall sagittal height of the eye and are primarily responsible for the physical fit characteristics of a soft lens on the eye. One study illustrates this nicely by considering the anatomical features under the typical diameter of a soft contact lens and evaluating their overall contribution to the sagittal height of the eye (Figure 1).1 In this study, the anatomical feature that matters the most in terms of the overall sagittal height of the eye is the corneal diameter. Next to corneal diameter, the rate at which the cornea flattens from center to periphery (i.e., corneal eccentricity) is the anatomical feature that has the second greatest impact. Outside of these these two, surprisingly, the corneal feature that matters least is the one that we measure the most: namely, central corneal curvature.

With this information in mind, it is really those extremes—patients who have excessively large or small corneas or excessively flat or steep corneas—that would have a sagittal depth profile that would be outside of the depth profile of those common standard soft molded lenses. It is really this fit mismatch that warrants a custom soft lens for optimal results.
It is also worth mentioning that associated with patients’ regular astigmatism at the corneal plane and the sagittal height of their eye, they may have a need for a high amount of minus or plus power correction, and this may warrant a custom soft lens. It is important to emphasize that patients who have a high amount of myopia with or without astigmatism will need less minus and cylinder at the plane of the cornea, while those patients who have a high amount of hyperopia with or without astigmatism will need greater sphere and cylinder at the plane of the cornea. There are numerous software-based calculators and tables that can assist with vertexing both meridians to the plane of the cornea, and these should be consulted prior to selecting a lens.
The other category of patients for whom a custom soft lens may be indicated are those who have irregular astigmatism. The compensation or correction of irregular astigmatism is not possible in the standard mass-produced lenses because they have central thickness profiles of approximately 0.08mm for a –3.00D lens and will drape over the cornea; therefore, all corneal astigmatism will manifest through the lens. It is not until a soft lens is thickened (Figure 2) that it begins to approach the non-flexing nature of a GP contact lens and masks some of the irregular astigmatism, converting it to more regular astigmatism that can be corrected by making the lens toric.

The typical custom soft lens intended for the management of irregular astigmatism has a central thickness of approximately 0.40mm. The irregular astigmatism-correcting ability of the lens can be verified by performing keratometry (manual keratometry or corneal topography/videokeratography) over the contact lens on the eye and evaluating the regularity of the reflected mires. Figure 3 shows a keratoconus patient who has irregular astigmatism as verified by the distorted mires with videokeratoscopy; some masking of the irregularity is evident with videokeratoscopy over a thickened custom soft lens for keratoconus. At this point, perform a sphero-cylindrical over-refraction and incorporate that power into the ordered lens.

DESIGNS
Like their mass-produced soft lens counterparts, custom soft contact lens designs are generally categorized by their optical profile. Also like their standard soft lens counterparts, spherical and toric custom soft lenses are designed by vertexing the manifest refraction to the plane of the cornea. What is unique about custom soft spherical and toric lenses is that the power can be ordered in steps as specific as 0.1D and in 1º axis increments versus the traditional 0.25D and 10º steps, respectively, of mass-produced lenses.
Multifocal and multifocal toric contact lenses that are custom in nature are unique in that not only is the add power customizable, but the placement of the distance and near optics is also customizable. Some designers and patients prefer a center-near multifocal lens, and some prefer a center-distance multifocal lens. What remains constant between the two is that both distance and near optics are presented to the eye at the same time; however, with custom contact lenses, eyecare practitioners have control over both the power of the central and the surrounding zones and, uniquely, over the sizes of the central and surrounding zones.
For example, when designing a center-near aspheric multifocal contact lens, the add power is first incorporated into the center, then the center-near zone size and the peripheral zone size (the point at which distance power/correction is reached) are specified. The zone sizes are selected based on each patient’s unique pupil size (Figure 4).

An optical design modification that is not often considered in custom soft contact lenses is varying the optical zone size in a single-vision lens. A reason to do this would be patient visual symptoms related to flare/glare/halos/starbursts around lights, particularly in low-light environments. This occurs because the optical zone within the contact lens is too small in relation to the patient’s pupil size. As the pupil gets larger in relation to the optic zone, the likelihood for glare and halos increases.
First perform a sphero-cylindrical over-refraction to ensure that there is no uncorrected sphere or cylinder contributing to patients’ visual symptoms. If after performing a sphero-cylindrical over-refraction the patients’ symptoms remain, it may be assumed that the optic zone is too small and will need to be increased. Assess this clinically by partially occluding the eye that is not experiencing the visual disturbance and shine a penlight or transilluminator into the partially occluded eye. This shrinks the pupil size in both eyes due to the yoked effect. If patients report an improvement in visual symptoms, then ask the custom soft lens manufacturer to increase the optic zone diameter in an attempt to eliminate the flare and halos (Figure 5).

FITTING
As discussed earlier, in the study on anatomical contributions to sagittal height,1 the goal of evaluating the anatomical features of the eye is to gain an understanding of how they relate with one another and control the sagittal depth of the eye. The final frontier in custom soft lens design and prescribing is the understanding and precise measurement of the depth of the eye, as this would truly be the way to arrive at a custom fit.
Topography software is available that provides sagittal height data over specified chord lengths, and computer algorithms can extrapolate out to a chord of the diameter of a typical soft contact lens. There is also optical coherence tomography (OCT) technology available to calculate the sagittal height of the eye. However, until these technologies mature and are widely available in clinical practice—and until soft contact lens manufacturers provide the sagittal depths of their lenses in addition to the base curve and overall lens diameter—eyecare practitioners will need to calculate the necessary base curve and diameter to achieve an optimal lens-to-eye fit via other means.
If trialing a standard soft lens fails secondary to the physical fit on the eye, and/or the size and shape of the eye are identified as being beyond the normal range, it is appropriate to utilize a custom lens. To better accomplish this, perform a quick evaluation of the amount of limbal coverage provided by a standard soft lens of a known diameter. After placing the lens on the eye and allowing it to settle, measure the amount of coverage/extension beyond the limbus (Figure 6). The lens should extend a minimum of 1mm beyond the limbus if it is manufactured in toric powers.
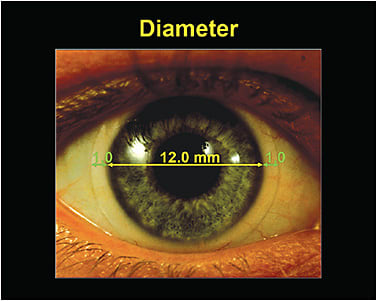
Next, evaluate the relationship between VID and corneal curvature. As the cornea steepens, it deepens, and the cornea deepens as it gets larger. It is therefore those patients who have large, steep corneas who will need large, steep, and deep custom soft lenses, and this should be communicated to the laboratory. The converse is also true—those patients who have small and relatively flat corneas have an overall shallow sagittal height and should be prescribed smaller and shallower lenses (Figure 7).

MATERIALS
When custom soft contact lenses are manufactured, the anhydrous button is cut on a lathe similar to how GP corneal and scleral lenses are; however, there is an extra step after lathing that hydrates the lens, resulting in diameter expansion and ultimately the final base curvature and power. Standard soft lenses are manufactured in a very different method in which they are generally molded in mass quantities. It is this manufacturing process in which the varying material characteristics between custom lathe-cut soft lenses and the molded standard soft lenses become apparent.
Historically, we have used traditional hydrogel HEMA-based materials in custom soft lenses. The hydrogel-based plastics can be easily lathe-cut, and they hold onto water well after the process of hydration. But the benefits associated with the increased oxygen transmission profile of molded silicone hydrogel lens materials prompted custom soft material manufacturers to accomplish the task of creating silicone hydrogel materials that could be successfully lathe-cut, would hydrate and expand at a predictable and stable state, and would remain optically clear and wettable during wear.
Several latheable silicone hydrogel materials are now available in the marketplace and can be considered when the increased oxygen profile inherent with silicone hydrogels is desired. It should be noted that no custom soft lens material or design (hydrogel or silicone hydrogel) has U.S. Food and Drug Administration clearance for use overnight in the closed eye.
OVER-REFRACTION
In an effort to optimize the vision of a custom soft toric lens, the first step is to verify the lens fit and stability. After ensuring that the fit and stability of the lens are appropriate, record the direction and amount of rotation of the orientation markers on the lens.
Next, perform a sphero-cylindrical over-refraction. Once the desired endpoint acuity is achieved, input that information into a cross-cylinder calculator. Several cross-cylinder calculators are available. They each vary slightly with regard to the information necessary to make the calculation. However, generally, the information needed is manifest refraction, the power of the contact lens that is on the eye at the time of the sphero-cylindrical over-refraction, the sphero-cylindrical over-refraction value, and the direction and amount of rotation. Once the calculation is made, order the contact lens to retrial on the patient.
REPLACEMENT SCHEDULES AND CARE SOLUTIONS
The typical replacement schedule suggested for custom soft contact lenses varies by manufacturer, design, and material; however, it is generally monthly, quarterly or semi-annually. This is in stark contrast to the standard soft contact lens market, which has seen a shift away from longer replacement schedules toward daily disposable contact lenses.
The recommended replacement schedule in custom soft lenses becomes important during patient education and targeted care solution recommendations. In the care and handling of custom soft lenses, it is advocated to rub and rinse lenses to maintain their surface characteristics; this is also critically important to increase the longevity of custom soft contact lenses. Also, possibly using more traditional enzymatic cleaners or even isopropyl alcohol cleaners approved for soft lenses can dramatically lessen deposition. However, if you prescribe such cleaners to custom soft lens wearers, communicate to these patients to vigorously rinse their lenses prior to storage and/or application to the eye.
FINAL THOUGHTS
Custom soft contact lenses can be incredibly rewarding for both patients and practitioners. It is those unique challenges that present the greatest reward in clinical practice when success is reached. CLS
REFERENCES
- Young G. Ocular sagittal height and soft contact lens fit. Cont Lens Anterior Eye. 1992;15(1):45-49.




