For the fourth consecutive year, the American Optometric Association (AOA) Contact Lens and Cornea Section (CLCS) presented a two-hour course on the topic of clinical controversies at Optometry’s Meeting, which most recently took place from June 29 to July 2, 2016 in Boston. Among other activities, the CLCS is dedicated to protecting contact lens wearers from the consequences of illegal contact lens sales and to promoting contact lens safety in general (see sidebar on next page).
The 2016 Clinical Controversies course featured a debate format that addressed a number of interesting and controversial contact lens topics, all of which have at least two different approaches in terms of management. The questions posed during the program included:
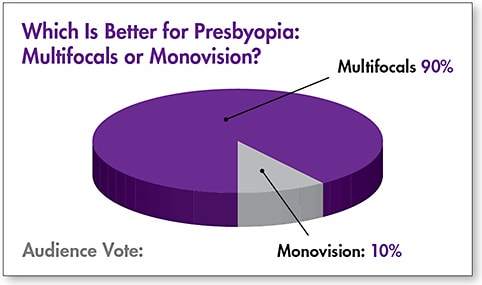
1) Which is better for presbyopia: multifocals or monovision?
2) Does playing outside slow progression of myopia?
3) Which is better for pediatric aphakes: intraocular lenses (IOLs) or contact lenses?
4) Is ultraviolet (UV) treatment in a contact lens important?
5) Which is better for myopia control: soft multifocals or corneal reshaping?
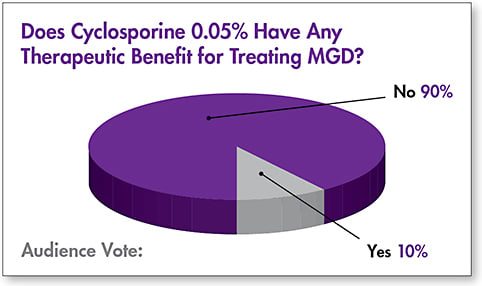
6) Does cyclosporine 0.05% have any therapeutic benefit for treating meibomian gland dysfunction (MGD)?
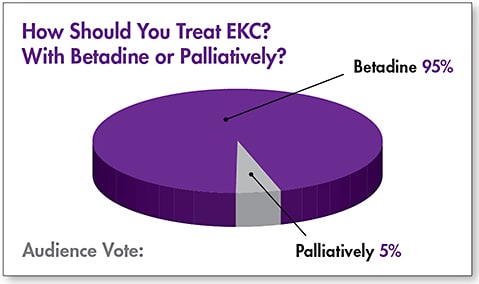
7) How should you treat epidemic keratoconjunctivitis (EKC): with betadine or palliatively?
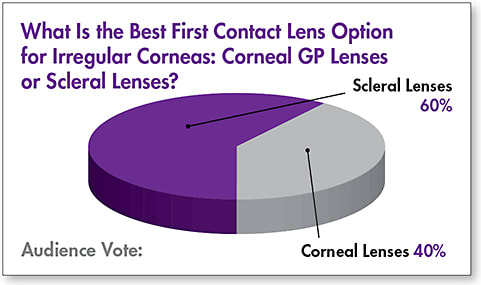
8) What is the best first contact lens option for irregular corneas: corneal GP lenses or scleral lenses?
The debate included CLCS council members who, in many cases, were assigned the topic to debate. Prior to the discussion on each topic, the audience voted in terms of their preference for that topic (Figures 1 to 8).
WHICH IS BETTER FOR PRESBYOPIA: MULTIFOCALS OR MONOVISION?
Multifocals: Dr. Edward S. Bennett There are many viable contact lens options for correcting presbyopia, and both soft and GP multifocals and monovision should certainly be in our presbyopia toolbox. That said, many compromises are inherent with monovision that should be considered when making the decision as to which modality would be preferable for a given patient.
Monovision causes a reduction in contrast sensitivity function compared to multifocal lenses (Richdale et al, 2006; Rajagopalan et al, 2006), which is proportional to the amount of add power (Bennett and Jurkus, 2005). Monovision also significantly reduces stereoacuity (Johannsdottir and Stelmach, 2001). Monocular suppression of blur occurs, which increases with increased add power (Collins et al, 1993); in fact, changes in refractive anisometropia ≥ 0.50D have occurred in 29% of monovision wearers (Wick and Westin, 1999).
Of concern is the fact that 80% of monovision wearers have experienced problems with night driving (Johannsdottir and Stelmach, 2001) and have difficulty suppressing headlights (Wood et al, 1998). Therefore, when prescribing monovision, it is very important to prescribe over-glasses for use in all critical distance tasks.
Fortunately, today we have a large and increasing number of multifocal lens options for presbyopes. These include high-add-power aspheric corneal GP multifocals to complement available segmented translating designs, hybrid multifocals, and scleral multifocal designs.
Recent soft multifocal designs feature many improvements that have resulted in a higher success rate and improved vision as compared with previous designs. This was evident in a recent study (Sivardeen et al, 2016), which found that four popular soft multifocal designs all outperformed monovision from a visual standpoint. The introduction of frequent replacement—and even daily disposable—multifocal modalities is a great benefit for a drier-eyed population.
When multifocal contact lenses and monovision have been directly compared in crossover studies, 68% to 76% have preferred multifocals (Johnson et al, 2000; Benjamin, 2007; Richdale et al, 2006; Kirschen et al, 1999; Situ et al, 2003). In addition, multifocal contact lenses result in improved stereopsis (Kirschen et al, 1999; Richdale et al, 2006) as well as improved low- and high-contrast acuity and contrast sensitivity (Rajagopalan et al, 2006). Multifocal lenses are also preferred by patients in real-world situations (Woods et al, 2009).
Therefore, when providing options to presbyopic patients, it is important to position multifocal lenses first. A recent survey showed that 71% of eyecare practitioners (ECPs) do in fact prefer multifocals as compared to monovision (19%) and single-vision lenses with over-spectacles (10%) (Nichols, 2016). So, it is evident that ECPs are recognizing the benefits and increased quality of our current generation of multifocal contact lenses.
THE CLCS: AN ADVOCATE FOR CONTACT LENS SAFETY
The CLCS is the voice of contact lenses for the profession and advocates for the safety of the public by working to help protect lens wearers from the harms of illegal contact lens sales. To that extent, a large and growing number of both websites and businesses have received cease and desist orders from the AOA legal department for illegally selling contact lenses. In addition, an email has been established (stopillegalCLs@aoa.org) through which you can report suspected illegal contact lens sales as well as any adverse events resulting from illegal contact lens sales. The CLCS—in conjunction with the American Academy of Optometry’s Cornea, Contact Lenses & Refractive Technologies Section—also developed a website (www.contactlenssafety.org ) to inform and educate consumers about contact lens safety.
Monovision: Dr. Pamela Lowe Contact lens options for presbyopes have certainly evolved over the past 30 years. With the advent of innovative multifocal contact lens designs, the traditional, tried-and-true monovision concept has received a negative reputation and is perceived as “old school.” Having learned how to fit contact lenses in a time when monovision was the only presbyopic option, I still believe that monovision is an effective tool to meet the needs of today’s presbyopes.
To defend monovision’s value, it is important to dispel the misnomer that monovision negatively impacts binocularity. True, we are correcting each eye for a specific working distance—one eye for predominately distance demands, and the fellow eye predominantly for near—but two eyes are required for success with monovision, so in effect, it is a binocular procedure. The two eyes are still working as a team to maximize the clearest vision at distances important for visual clarity and comfort.
The notion that multifocal contact lenses don’t disrupt binocularity is not entirely true; most multifocal lens designs have distance and near optics simultaneously covering the pupil, which inherently induces aberrations into the visual system. Binocularity will be impacted to some degree any time that we are disrupting the clarity of focus; but, fortunately, this doesn’t translate into any impactful loss of visual performance (Wood et al, 1998). With this in mind, here are the three primary advantages of monovision:
1) Ease of Fit Monovision is all about addressing patients’ visual needs by determining which working distance is most important for them to have optimized visual performance (distance or near); that power lens is utilized on the dominant eye, and the fellow eye is then corrected with the power for the working distance that is not as critical to visual comfort. Fitting monovision gives you more control for customizing working distances to enhance patients’ lifestyle needs.
2) Wider Parameters Available Monovision offers much more flexibility in fitting higher refractive errors and astigmatic patients. Multifocal lenses—notably soft designs—fall short in the range of parameters available, especially for higher hyperopes and those who have greater corneal toricity. Most soft multifocal lens designs do not extend beyond +6.00D, and availability along with functional vision is much more difficult to obtain in astigmatic multifocal lens designs.
3) Excellent Practice Management Tool Monovision is an effective tool for fitting presbyopic laser-assisted in situ keratomileusis (LASIK) patients pre-operatively to determine whether monovision surgery would be successful. It is also an excellent way to satisfy specific visual needs by prescribing part-time spectacles over monovision to enhance specific visual tasks. For example, it is very common for monovision patients to have a pair of spectacles to wear over their contact lenses to optimize distance acuity for driving. What a great way to enhance vision and increase optical sales.
DOES PLAYING OUTSIDE SLOW THE PROGRESSION OF MYOPIA?

Yes: Dr. Jeffrey J. Walline The literature on outdoor time and myopia progression is relatively new. Jones and colleagues first reported that outdoor time is associated with increased myopic refractive error in 2007. Since then, several other investigations have also reported an association between time spent outdoors and myopic refractive error (Dirani et al, 2009; Guo et al, 2013; Rose et al, 2008).
Similarly, Fulk and Cyert first reported a seasonal effect on myopia progression in 1996, namely that myopia tends to progress more slowly during the summer months than it does during the winter months. This effect has subsequently been reported by several other studies as well (Donovan et al, 2012; Fulk et al 2002; Goss and Rainey, 1998; Gwiazda et al, 2014). Children spend more time outdoors during the summer months (Deng et al, 2010), so it is assumed that they progress less because they spend more time outdoors.
Schools in Guangzhou, China participated in a randomized clinical trial in which some schools were randomly assigned to an additional 40-minute outdoor activity during each school day throughout the school year. These children were compared to those from other schools who did not receive the additional 40 minutes of outdoor activity (He et al, 2015). In the schools that had compulsory outdoor times, the children were also encouraged to spend more time outdoors in their spare time. The encouragement did not result in more time spent outdoors outside of school (Dirani et al, 2009; Guo et al, 2013; Rose et al, 2008). However, the extra time spent outdoors during the compulsory 40-minute period was associated with slowing the progression of refractive error over three years from –1.59D to –1.42D, which was statistically significant (He et al, 2015).
A study in Taiwan randomly assigned one school to encourage almost seven hours per week of additional outdoor time compared to a school that gave no encouragement of outdoor time (Wu et al, 2013). They found that the progression of refractive error was faster for the school that did not encourage outdoor time when considering all students. When they compared only the myopic students who were not using atropine, they found that the progression was almost half for those who were encouraged to increase outdoor time, although the results were not statistically significant.
Outdoor time almost certainly affects the onset of myopia, and evidence indicates that it may also affect the progression of myopia. The onset and progression of myopia are closely linked, and encouragement of more outdoor time includes benefits beyond refractive error. Therefore, further investigation of the effect of outdoor time on myopia progression is possibly warranted despite a current lack of understanding of the mechanism by which outdoor time may slow myopia progression.
No: Dr. Jeffrey Sonsino In the 1970s, there was a mounting body of evidence that yellowing fingers were associated with lung cancer (Gauch, 2009). Some postulated that based on the data, it appeared that the yellowing fingers caused lung cancer (Gauch, 2009). In fact, yellow fingers were the byproduct of cigarette smoking, which we all now know is a causative agent in lung cancer. The point is that in evaluating any clinical study, readers must answer the question of whether the results make intuitive sense or whether they may be skewed by testing bias and poor experimental design. In other words, don’t turn off your brain when you are reading studies.
There are a litany of reasons why a clinical study may be weak, but common reasons include too narrow a patient population, failure to use appropriate controls, failure to demonstrate comparability of subjects in treatment and control group, confounding variables, and systematic errors and differences in measurement (Joy et al, 2005).
By no means am I suggesting that the science was weak in the studies indicating that outdoor time slowed myopia progression, but it is ultimately up to the readers of those papers to decide.
Although there are a few studies indicating that time spent outdoors is related to myopia progression, there are many more indicating that near work and near defocus is related (Jacobsen et al, 2008; French et at, 2013; Ip et al, 2008; Mutti et al, 2002). At this point, based on the literature, we are unable to determine the cause of myopia. But, as we continue the search for more answers, please remember to read clinical studies with a critical eye.
WHICH IS BETTER FOR PEDIATRIC APHAKES: INTRAOCULAR LENSES OR CONTACT LENSES?

Intraocular Lenses: Dr. Lowe Pediatric patients who undergo cataract extraction present a special challenge in clinical decision-making regarding the best way to manage their refractive error postoperatively. Of course, the younger the patient, the more aggressive you must be in combating any amblyogenic factors that could rob the patient of functional vision. IOL placement has compelling advantages over contact lens correction:
1) Guaranteed Correction The primary advantage of IOL placement in a pediatric patient is the guarantee that vision is being corrected 24/7. Pediatric patients, especially infant to toddler age, are obviously not capable of managing the rigors of contact lens application and removal, let alone the maintenance of contact lens care. Parents managing aphakic contact lenses have a heavy burden of constant compliance to avoid vision loss in their child; this is a heavy burden to put on even the most caring of parents. IOLs alleviate the cost of poor contact lens compliance or the risk of infection that corneal lenses pose.
Unlike contact lens powers that can be changed, IOL calculations have one shot at being as accurate as possible. Knowing the amount of normal myopic shift as pediatric eyes grow is key in IOL lens power selection and is vital in managing patients’ visual development with the target goal of aiming for emmetropia. Formulas for IOL power calculation have come a long way in predicting the proper IOL selection depending on patient age (Tromans et al, 2001; VanderVeen et al, 2012).
2) Reduces Amblyogenic Factors As previously stated, IOL placement is a guaranteed form of correction that can be easily enhanced by corrective spectacles if needed. This becomes even more important in the proper visual development of unilateral aphakes. In such cases, if contact lenses are not being properly placed during most of the child’s waking hours, this would seriously contribute to permanent vision loss due to suppression from deprivation and anisometropia.
3) Long-Term Cost Pediatric aphakes have a lifetime of visual correction needs. Hands down, the initial investment of an IOL is more cost effective compared to years upon years of contact lens replacements. Premium pricing for specialty aphakic lenses and the need for multiple lenses over a lifetime not only has a financial impact, but a physical impact on patients’ corneal health. The normal oxygen deprivation of a hyperopic lens in combination with the physical mechanics of a silicone polymer riding on the cornea certainly takes its toll. Pediatric IOL placement has its risks, including increasing risk of glaucoma (especially the younger the patient); but, the cost-to-risk ratio definitely favors IOL placement.
In a matter of a few short decades, cataract surgery, which was already safe and effective, increased in safety and efficacy, coupled with it becoming a refractive procedure due to the advent of laser-guided, wavefront technology available in the operating room. There has never been a better time for enhanced outcomes in the hands of a skilled surgeon.
Contact Lenses: Dr. Jason Compton While there are advantages to using an IOL, we also need to recognize the challenges. At this stage, the eye is growing so rapidly that it can be difficult to judge the correct focusing power. IOL surgeries (typically safe in adults) tend to be more prone to postoperative problems in a pediatric population (Plager et al, 2011). There are additional concerns such as inflammation, postoperative corneal astigmatism, and whether the posterior capsule is even able to support the IOL.
The Infant Aphakia Treatment Study (IATS) (Lambert et al, 2014) did an excellent job of addressing the question of IOLs versus contact lenses. This study began in 2004 (114 infants). One-half of the participants (babies four weeks to seven months) received IOLs, and the other half received contact lenses. No significant difference in visual acuity was found between the two groups at age 1 or at 4.5 years, but more complications occurred in the IOL group, which led to more corrective surgeries (Lambert et al, 2014).
When it comes to contact lenses in this population, a larger focus has to be on the parents (or guardians). Can the parents deal with the responsibility of contact lenses? Congenital cataracts are hereditary; do the parents have visual problems that would make it difficult to remove and apply lenses? There is also a financial responsibility as well; IOLs are covered by insurance, whereas contact lenses are not. While there are means available to get lenses for those who are financially challenged, this may be a concern.
GP lenses are easier to apply and remove, are available in unlimited parameters, and provide better quality of vision at higher powers. Soft lenses for aphakia are immediately comfortable and easy to prescribe. With the available options and limited risk, contact lenses continue to be a better option for pediatric aphakes.
IS UV TREATMENT IN A CONTACT LENS IMPORTANT?

Yes: Dr. Shalu Pal I believe that UV blocking in contact lenses is an important feature and that we should discuss it with our patients to maximize their protection from the sun’s harmful rays. We are all aware of the damage that UV light can do to the eye, including the formation of pingueculae and pterygia, eyelid and conjunctival cancer, solar keratopathy, retinal damage, and the advancement of cataracts and macular degeneration (Ham et al, 1982; Ham et al, 1978).
UV protection is something that we think about on a regular basis through the use of products including sunscreens, face creams, and lotions; lip balms; hats; sunglasses; and UV coatings on windshields. When it comes to ophthalmic lenses, all have a built-in UV protection that we do not have to think about; it is automatically there, protecting our patients. Why do we not automatically think of it for our contact lens products of choice?
When it comes to protecting the eyes, sunglasses are not enough. Studies show that up to 45% of UV light is still reaching the eye from the top, bottom, and sides of sunglasses, which can increase the risk of the peripheral light focusing effect (PLF). PLF refers to UV light damage due to oblique UV light being refracted from the peripheral cornea to concentrated sites inside the anterior segment (Kwok et al, 2003). The use of UV-blocking contact lenses reduces the PLF effect by 69% for UVA and 96% for UVB (Kwok et al, 2003; Walsh et al, 2001).
UV damage is accumulative over the course of our life, with 50% of that damage occurring before the age of 20 (Green et al, 2011). Children have larger pupils and clearer crystalline lenses, thus allowing more light into the eye. By the age of 15, 80% of children have signs of UV damage (Ooi et al, 2006). Maximum protection is achieved with UV-blocking contact lenses, UV-blocking sunglasses, and wearing a wide-brimmed hat (Young and Sands, 1998). Only 3% of our children are wearing sunglasses when outdoors, and we as practitioners need to be doing a better job of educating parents about the importance of this (Young and Sands, 1998).
No: Dr. Walline If you ask parents whether we should protect their children from the potentially harmful effects of the sun, of course the answer is “yes.” If you ask parents how that should be accomplished, they would likely say that we should use sunscreen, wear clothes that protect, stay out of direct sunlight, and wear sunglasses. Few parents would say that their child should wear contact lenses to protect them from the sun.
We frequently prescribe contact lenses for people who wish to wear plano sunglasses, either for fashion or light sensitivity. The sunglasses provide adequate protection from the sun, although peripheral light rays may still affect ocular health. There is no direct evidence of the effect of peripheral light rays on the risk of ocular complications, and it is unlikely that they affect the crystalline lens or the retina. Hats can also help to protect the eyes from the harmful effects of UV light.
Although contact lenses that block UV light provide a benefit beyond vision correction without any associated harmful effects, selecting a contact lens based on UV protection doesn’t make much sense. Vision, comfort, and ocular health are all far more important factors when choosing a contact lens. If the contact lens that provides the best vision and comfort also happens to contain protection from UV radiation, then the benefits far outweigh the risks. However, if any compromise of vision or comfort is necessary to maximize UV protection, then the risk-to-benefit ratio is skewed and may indicate that there is not a strong need for UV protection.
When considering contact lenses for our patients, if everything else is equal, perhaps we could consider a contact lens that provides UV protection. Otherwise, it is not something that we need to recommend to patients until further evidence shows long-term ocular health benefits provided by UV-blocking contact lenses.
WHICH IS BETTER FOR MYOPIA CONTROL: SOFT MULTIFOCALS OR CORNEAL RESHAPING?

Soft Multifocals: Dr. Lowe Regarding myopia control, the good news is that both multifocal contact lenses and corneal reshaping are viable options; it’s great to have two effective tools in our clinical bag to lessen the impact of myopia progression in our pediatric population. Clinically, I prefer soft multifocal lenses as my modality of choice for the following reasons:
1) Decreased Risk Factors/Increased Compliance Distance-center multifocal contact lenses with high adds have proven efficacy in myopia control (Walline et al, 2013; Aller et al, 2016). There are currently four of these designs available, all in a disposable modality. Daily wear of these frequently replaced lenses poses less risk of complications compared to the required sleeping in GP lenses to reshape the cornea. Ease of adaptation to soft lenses also increases compliance; therefore, patients wear their lenses comfortably all day, which increases efficacy of treatment.
2) Consistent Vision to Day’s End Corneal reshaping is most effective in low-to-moderate myopia. As myopia approaches the 4.00D range, visual clarity with corneal reshaping can decrease as the day progresses. Optimally, multifocal lenses offer patients clear, consistent vision all day without the possibility of blur induced from corneal shape rebound.
3) Lower Dropout Rates Discomfort and inconvenience are known factors contributing to contact lens dropout (Rumpakis, 2010). Soft, frequently replaced contact lenses are easy to care for and offer healthy pediatric patients comfortable wear from the onset of treatment. Corneal reshaping lenses have the potential for lens awareness, especially during initial adaptation to the rigid lens flattening properties, which can more readily contribute to young patients becoming less motivated to persevere with therapy.
Whether patients are fit with overnight corneal reshaping or daily wear soft multifocal distance-center designs to alter ocular axial length, it’s important to educate parents of young near-sighted patients that effective treatments are now available to take control of progressive myopia. When it comes to myopia control, eye-care practitioners need to be proactive in offering these viable clinical treatments that enhance the quality of pediatric patients’ lives and offer lifelong vision benefits.
Corneal Reshaping: Dr. Bennett
The Benefits Corneal reshaping offers numerous benefits compared to soft multifocals for myopia reduction, including:
1) Myopia is reduced via corneal shaping overnight, resulting in the absence of a need for vision correction during the day and greater visual freedom for eligible patients.
2) Corneal reshaping is a good option for individuals who are very active, notably young athletes.
3) Corneal reshaping results in unaided vision similar to aided vision with soft lenses (Ritchey et al, 2005). In addition, when corneal reshaping lenses and two-week replacement lenses were directly compared in a forced-choice scenario, 67.7% preferred corneal reshaping (Lipson et al, 2005).
4) There is excellent long-term evidence supporting myopia control with corneal reshaping. It has been stated that a reduction in myopia progression of 50% is clinically meaningful to patients (Walline, 2012; Holden, 2015). For example, a 1.00D myope at age 8 would, on average, progress to 5.00D of myopia by age 16. A 50% reduction in myopia progression would result in the same patient having myopia of only 3.00D at age 16. Several studies have demonstrated the efficacy of corneal reshaping for myopia control. Many have either approximated the 50% goal or exceeded it (Cho et al, 2005; Walline et al, 2009; Charm and Cho, 2013).
Dispelling the Concerns: Many concerns that ECPs may have about corneal reshaping are actually quite easy to resolve or dispel:
1) Adaptation Corneal reshaping wear results in much quicker adaptation compared to corneal GP lenses because the lenses have larger diameters that move less with the blink, and they are worn only at night.
2) Certification Certification can be completed online and is quite simple and straightforward. Thousands of ECPs have been certified.
3) Handling Studies have found that the great majority of young people successfully adapt to—and can handle—corneal reshaping lenses (Walline et al, 2009; Cho et al, 2005; Walline et al, 2004).
4) Microbial Keratitis The great majority of reports of microbial keratitis with corneal reshaping have been from southeast Asia (Swarbrick, 2009). The risk of a corneal ulcer with overnight corneal reshaping is similar to with any other overnight contact lens modality (Bullimore et al, 2013).
5) Complicated Fitting Process Corneal reshaping lenses are most often fit empirically with very good first-fit success. In fact, one large multicenter study reported that 80.5% of children fit into corneal reshaping lenses experienced success with the first lenses fit (Eiden et al, 2009).
Soft Multifocal Challenges Soft multifocals/peripheral plus designs are still in their infancy, and there are several challenges and unanswered concerns with this modality, including (Swarbrick, 2016):
1) The studies to date have greatly varied in treatment protocol.
2) The lenses used have also varied greatly in parameters and design.
3) At times, a large difference has resulted between the change in the refractive error versus the change in axial length.
4) To date, the treatment periods have been relatively short, often one to two years.
5) Typically, there has been non-randomization of subjects, a high dropout rate, and use of historical or contralateral eye as control.
6) The impact of a multifocal lens on vision.
The Bottom Line Corneal reshaping allows long-term effective myopia control as confirmed by a number of clinical studies. The U.S. Food and Drug Administration (FDA) is gathering evidence on corneal reshaping as a modality for myopia control. The quality of unaided vision rivals that of aided visual acuity with daily wear soft contact lenses and is not compromised via having a multifocal correction in front of the eye. It also represents a viable option for most astigmatic patients. The visual freedom of not needing to wear a correction during the day makes it a very good modality for active individuals—including young people—involved in sports.
DOES CYCLOSPORINE 0.05% HAVE ANY THERAPEUTIC BENEFIT FOR TREATING MGD?
Yes: Dr. Sonsino Cyclosporine 0.05% is not indicated for the treatment of MGD. However, in its 14-year history on the market, many practitioners have used this product off-label as an adjunct to the MGD regimen. Of course, the regimen may include hot compresses, lid hygiene, lipid emulsion artificial tears, supplementation with omega-3 fatty acids, and gland expression. Dr. Donald Korb recommends 15 minutes of intense heat in each hot compress session (personal communication). We all know from clinical experience that although this regimen typically improves the quality of the tears, it is not a cure, and MGD must be managed chronically.
In fact, three studies published in well-respected journals have shown improvement in clinical signs, improvements in symptoms, or both when treating MGD with topical cyclosporine 0.05% (Perry et al, 2006; Prabhasawat et al, 2012; Rubin and Rao, 2006). Although the mechanism of action has not quite been determined with this treatment, it is likely the interruption of the inflammatory cascade associated with dry eye.
Interrupting the inflammatory cascade can be accomplished with topical steroids, which are generally regarded to be safe only for short-term use, and/or an immunomodulator such as cyclosporine 0.05% or lifitegrast 5%. Whether you believe that the mechanism of action is increased tear production or interruption of the inflammatory cascade, both compounds are safer long-term compared to using topical steroids. Whenever we are determining a treatment regimen for patients, we must weigh the risk/benefit ratio. According to the package inserts, the major risks for lifitegrast are burning and stinging upon instillation, altered taste, and blurred vision; the most common for cyclosporine is ocular burning. These are relatively minor risks; if there is any benefit at all, the risk/benefit ratio would still be favorable.
No: Dr. Pal MGD is a blockage of the meibomian glands, resulting in poor secretion of oils from the eyelids onto the ocular surface. The oils within the glands become stagnant and thickened, which leads to poor quality tears and, ultimately, ocular surface dryness.
The FDA approved topical cyclosporine in 2003 for increasing tear production in patients who have inflammatory dry eye disease (Donnenfeld and Pflugfelder, 2009). Cyclosporine is an immunomodulator that inhibits t-cell activation, inhibits apoptosis of epithelial cells, and increases the density of goblet cells. It also repairs the ocular surface (Kymionis et al, 2009).
It is a great product and very effective in reducing the clinical signs and symptoms of dry eye disease (Rao and Rao, 2006). Cyclosporine does not decrease the blockage of the glands, nor does it improve oil secretion or quality. It is very effective at reducing inflammation of the cornea, and it does improve the ocular surface. When we used cyclosporine with a patient who had MGD in our clinic, we were ultimately treating the side effects of MGD. However, I believe that it does not treat MGD directly. There are no current studies showing that cyclosporine effectively improves MGD with any clinical significance (Prabhasawat et al, 2012).
HOW SHOULD YOU TREAT EKC: WITH BETADINE OR PALLIATIVELY?
With Betadine: Dr. Pal Each of us will eventually see a patient who has the perfect storm known as EKC: an acute onset of watery eyes, swollen lymph nodes, conjunctival petechial hemorrhages, pseudomembranes, pain, and discomfort (Melton and Thomas, 2008)
Currently, there are no FDA-approved medications to treat adenoviral conjunctivitis. EKC will self-resolve slowly over several weeks. Some ECPs prescribe cool compresses and artificial tears for palliative support during this time. I think that we can do better for patients.
When surveyed, 30% of ECPs have used a 5% betadine wash to help reduce their patients’ suffering (Than et al, 2014). Betadine reduces the viral load and the presence of corneal subepithelial infiltrates, which dramatically slows down the progression of EKC. Both the infectious period and the period of suffering are reduced with this wash (Melton and Thomas, 2008).
Based on our experiences in our clinic, this procedure is safe, inexpensive, takes only two minutes to perform, and, most importantly, it works. There is no scientific evidence behind the use of betadine to treat EKC, but anecdotally, it is a miracle cure that has helped many patients. Our job is to help our patients by all means within our scope, while doing no harm. Trust in yourself and in those who have done this hundreds of times before you.
Palliatively: Dr. Walline EKC is a self-limiting disease that resolves spontaneously within one to three weeks without significant complications. Symptoms are often described as itch and irritation, but rarely pain. EKC is caused by an adenovirus, and there are no antiviral treatments currently available to treat EKC.
Treatment is mostly aimed at alleviating symptoms with cold compresses and artificial tears. While steroids may reduce symptoms, they also increase the time course of the disease, thereby providing little benefit.
Today, innovative treatments attempt to rid the eye of the virus. One such treatment uses an in-office application of iodine to the eye to reduce the viral load and shorten the course of the disease. A protocol recommended by ECPs uses proparacaine to reduce the pain associated with iodine administration, topical non-steroidal anti-inflammatory drugs (NSAIDs) to reduce short-term pain sequelae, and loteprednol etabonate 0.5% q.i.d. for four to five days to improve comfort (Melton and Thomas, 2008).
It appears that the majority of this protocol is designed to alleviate the discomfort associated with the administration of iodine. Why not simply treat the symptoms of EKC, a self-limiting disease, with the same agents meant to improve ocular comfort following administration of iodine? Perhaps the most severe cases of EKC would benefit from administration of a painful treatment; but many cases of EKC are not so abrasive, so why subject patients to further discomfort when the disease is self-limiting?
WHAT IS THE BEST FIRST CONTACT LENS OPTION FOR IRREGULAR CORNEAS: CORNEAL GP LENSES OR SCLERAL LENSES?
Corneal GP Lenses: Dr. Sonsino Are you a scleral lens fitter or are you a problem solver? I am a problem solver who has sclerals in my armamentarium of contact lenses used to treat irregular corneas. In any disease, there is a continuum of care based on the severity of the disease state. An example of this is in the medical treatment of dry eye. One of the heavy guns that we use in severe dry eye therapy (ocular graft-versus-host disease, Sjögren’s syndrome, Stevens-Johnson syndrome) is autologous serum. But, when a patient presents with a mild lens-related dry eye, most of us are not pulling out the autologous serum. The reasons are cost, risks of dealing with blood-borne pathogens, the hassle of compounding, the hassle of storage, and the list goes on. We treat dry eye in a step-wise fashion according to the disease state.
Why would contact lenses be any different? Arguably, scleral lenses are more expensive, more time-intensive, a greater hassle to apply and remove, and have unknown long-term complications compared to corneal lenses. So, jumping to the most complex contact lens strategy in mild disease states does not make sense. In fact, at least one payer dictates two tiers of coverage for mild disease state and severe disease state. Let’s use our clinical judgment in making the best decisions that are in our patients’ interests each and every time.
Scleral Lenses: Dr. Compton There are some really great reasons to reach for a scleral lens first. Many can be defined by one underlying theme: enhanced patient experience. We might feel a great sense of accomplishment for achieving great acuity with an amazing alignment fit. But are we really successful if patients feel miserable and rarely even wear their lenses? My ultimate goal is to provide clear, comfortable vision as quickly as possible. Scleral lenses allow me to do that.
Comfort Without question, scleral lenses are more comfortable compared to standard corneal GPs. When fit correctly, they can feel as comfortable as soft lenses. Think how our fitting philosophy changed with the advent of soft lenses. Twenty-five years ago, we were fitting primarily corneal GPs; as materials evolved, the primary motivating force to switch to soft lenses was comfort. This could be the same motivating factor all over again.
Stability Scleral lenses are tucked under the lid, removing the risk of dislodgement. This is both a financial and a safety issue for active contact lens wearers.
Foreign Particles No foreign bodies become lodged under the lens. What can be a common complaint from corneal GP wearers is virtually a non-issue for scleral lens wearers.
Ocular Dryness The way in which scleral lenses vault over the cornea can have protective and soothing properties. We are literally bathing the eye in solution for the entire wearing time.
Improved Manufacturing Processes Scleral lenses are available with spherical, front toric, and multifocal optics as well as with toric peripheral curves, reverse geometry, quadrant-specific designs, notching, microvaults…whatever patients need.
Yes, there may be handling issues or concerns about tight fits or poor tear exchange, but these concerns can be addressed during the fitting process.
CONCLUSION
We hope that the information presented in these debates is beneficial in the clinical decision-making process whenever these specific topical areas are encountered in practice. The responses—with two notable exceptions—were quite definitive in what the preferred modality should be. However, the jury is still out on the effect of outdoor time on slowing myopia progression. The answer to this should become more evident over the next few years as we learn the results of ongoing research.
Likewise, there is not a definitive solution as to which contact lens—corneal or scleral GP—is preferable for irregular corneas. The trend in recent years is more toward sclerals; therefore, it will be interesting to see the results of this question if asked two or three years from now.
Please join us at our next Clinical Controversies course to be held at Optometry’s Meeting, June 21 to 25, 2017 in Washington, DC. CLS
The views expressed here are those of the presenters and not necessarily those of Contact Lens Spectrum.
For references, please visit www.clspectrum.com/references and click on document #254.
Dr. Bennett is assistant dean for Student Services and Alumni Relations at the University of Missouri-St. Louis College of Optometry and is executive director of the GP Lens Institute. He is also clinical features editor for Contact Lens Spectrum. You can reach him at ebennett@umsl.edu.
Dr. Walline is the Associate Dean for Research at The Ohio State University College of Optometry. He receives research materials from Bausch + Lomb. You can reach him at walline.1@osu.edu.
Dr. Sonsino is a partner in a high-end specialty contact lens and anterior segment practice in Nashville, Tennessee. For more than 12 years, he was on the faculty at Vanderbilt University Medical Center’s Eye Institute. Dr. Sonsino is a Diplomate in the Cornea, Contact Lens, and Refractive Technologies Section of the American Academy of Optometry, chairman of the Cornea and Contact Lens Section of the American Optometric Association, a fellow of the Scleral Lens Education Society, board certified by the American Board of Optometry, and the 2017 GP Practitioner of the Year awardee by the Gas Permeable Lens Institute (GPLI). He consults for or receives research support from Alcon, Art Optical, Johnson & Johnson, Optovue, Shire, SynergEyes, and Visionary Optics. He also has proprietary interest in LVR Technology and has received travel funding from Contamac.
Dr. Pal is currently the owner of a group practice in Toronto, specializing in specialty contact lens fitting and dry eye assessment and management. She is the vice chair of the AOA Contact Lens and Cornea Section Council, member of the Canadian Association of Optometrists, and sits on the Continuing Education Committee of the Ontario Association of Optometrists. Dr. Pal is a member of the Women’s Advisory Board for Alcon USA and speaker for Allergan’s Dry Eye Faculty in Canada, a consultant for several companies, and a facilitator of the STAPLE program.
Dr. Lowe is currently director/president of Professional Eye Care Center, Inc., a full-scope primary care practice she founded in Chicago, and she serves as an adjunct clinical professor for Illinois College of Optometry. Dr. Lowe is a past president of the Illinois Optometric Association and a member of the AOA, currently serving on the AOA External Communications Committee and as secretary of the AOA Contact Lens and Cornea Section. She is a Fellow of the American Academy of Optometry and a Diplomate of the American Board of Optometry. Dr. Lowe is also a consultant or advisor to Alcon, Visionx, Bausch + Lomb, and Johnson & Johnson Vision Care and has received lecture or authorship honoraria from Zeavision, Maculogix, and Eye Eco.
Dr. Compton owns a private practice “Compton Eye Associates” in the New York CIty area. He serves as assistant adjunct faculty for the SUNY College of Optometry. Dr. Compton is a fellow in the American Academy of Optometry. He is the president/founder of TheRightContact.com, a contact lens resource used by eyecare professionals worldwide. Dr. Compton is also a speaker for Johnson & Johnson Vision Care.



