The bar is perpetually set higher in terms of our ability to provide optimized vision, comfort, and physiological health response for our contact lens wearers. We can provide contact lens alternatives for our patients who have more normal refractive error (myopia, presbyopia, and astigmatism), for those who require vision improvement over spectacles due to corneal irregularity, for those who have compromised ocular surfaces, for those who have ocular disfigurement, and even for those who have progressive myopia, among others. Not only have the specific contact lens design alternatives developed at amazing rates, but the diagnostic technologies that we use to evaluate these eyes, design lenses, and monitor outcomes from our contact lens treatments have advanced greatly.
The development of these diagnostic technologies has significantly impacted not only what we can do with contact lenses, but how effectively the contact lens management strategies perform for our patients. This article will review a number of key diagnostic technologies that have dramatically raised the bar of performance in contact lens care. Specifically, it will review the following areas in which technology has had a dramatic impact on our contact lens practice:
- Evaluating the ocular health status prior to contact lens fitting.
- Managing regular corneas with topography-based fitting software for corneal GP lenses.
- Managing irregular corneas with advanced corneal shape analysis.
- Managing myopia with corneal reshaping assisted by advanced technology.
- Corneo-scleral profile systems for customized scleral lens design.
TEAR FILM AND OCULAR SURFACE ASSESSMENT TECHNOLOGIES
To significantly increase the likelihood of an appropriate physiological response to contact lens wear, it is important to perform a comprehensive assessment of the health status of the cornea, adnexa, and tear film. Advanced diagnostic technologies can provide a deeper and more detailed assessment in addition to the routine performance of biomicroscopy, vital staining, and observational examination of the tear film.
Tear Osmolarity Elevation of tear osmolarity is an integral part of the definition of dry eye disease, according to the International Dry Eye WorkShop (DEWS)study group report.1 Many commonly performed clinical tests for dry eye diagnosis suffer from poor specificity and sensitivity for disease detection. Osmolarity has very high predictive value (87%) for the detection of dry eye disease.1,2
One in-office system to measure osmolarity uses nanoliter-sized samples of tears from each eye to report osmolarity in milliosmoles per liter (mOsm/L). Evaluation of the maximum reading between the two eyes and the asymmetry of readings between the two eyes is used in the diagnosis of dry eye. Values above 308 mOsm/L for the higher of the two eyes, as well as an asymmetry of readings of 10 mOsm/L or more between the two eyes, generally indicate the presence of dry eye disease.
Although osmolarity does not specifically indicate the type or cause of dry eye, it can be used to not only initially assess for the presence of dry eye (versus other potential causes of patient symptomatology), but also can be used to monitor the efficacy of implemented therapies by comparing pretreatment versus post-treatment values.
Matrix Metalloproteinase-9 Detection To my knowledge, there is one commercially available, point-of-care immunoassay test designed to detect elevated levels of matrix metalloproteinase-9 (MMP-9) in the tears. MMP-9 is an inflammatory marker that is known to be elevated in patients who have dry eye disease. It is a cytokine produced by epithelial cells experiencing inflammation, and this measure has been found to have a sensitivity of 85% and specificity of 94%.3
A patient’s tear sample is taken from the inferior palpebral conjunctiva, with no anesthetic required. Once the tears are collected, the applicator is dipped into a solution for 15 to 20 seconds. This solution is able to detect MMP-9 within the tears. A red line appears on the applicator if the tears are positive for MMP-9 (> 40 ng/ml). The intensity of the red line increases with higher levels of MMP-9. A blue line will appear for negative results, and no lines will appear if the test is invalid. The test can be administered in-office and takes about 10 minutes from start to finish for results. Positive results allow practitioners to begin anti-inflammatory therapy in an effort to improve patients’ eye comfort and health while reducing dry eye symptoms. Again, follow-up testing can be used to confirm control of inflammation with therapy.
Lipid Layer Thickness, Meibography, and Blink Pattern Evaluation One diagnostic system for evaluating ocular surface health is an accurate instrument that was initially developed to precisely measure tear lipid layer thickness. It also enables practitioners to evaluate blink characteristics such as blink rate and the presence of incomplete blinks. The most recent version of this system has added a high-resolution infrared meibography component. Although most often used in combination with a partner therapeutic system, it is now available as a stand-alone diagnostic instrument.
The system utilizes interferometry to measure lipid layer thickness down to the submicron level of accuracy. It further incorporates what the manufacturer terms dynamic meibomian imaging (DMI) to produce detailed images of the meibomian glands to demonstrate ductal gland dilation plus gland atrophy and dropout, which are common to meibomian gland dysfunction (MGD).
Tear Film Analysis and Ocular Surface Diagnostic Software Another instrument that is helpful in evaluating ocular surface health is primarily designed as an advanced Placido-based topography system; however, additional illumination, imaging, and software systems dramatically expand the diagnostic applications of the instrument. Diagnostics geared toward dry eye and the ocular surface make this instrument a multifunctional powerhouse.
Tear film stability has traditionally been evaluated by performing invasive tear breakup time measurements by observing dry spot formation on the cornea following instillation of sodium fluorescein. This topography system has software that non-invasively quantifies tear breakup time at multiple areas throughout the corneal surface. The video imaging system detects distortions of the Placido rings reflected on the ocular surface and can indicate breakup of the tear film down to 0.1-second increments (Figure 1). Normative data for first breakup time and average breakup time is determined and can be used to categorize tear film stability. In addition, observation of the corneal area of tear breakup and the slope of the tear breakup graph provides a clear indication of the stability of the pre-corneal tear film.

Tear volume can be evaluated by measuring the height of the inferior tear meniscus. Typically, a qualitative evaluation of the tear meniscus height is determined by slit lamp observation of the tear meniscus. This instrument has software that can image the inferior tear meniscus and allow for quantitative measurement via the use of computer-generated calipers. Accuracy of measurements can be made down to 0.1mm increments. Population studies have shown that a normal inferior tear meniscus is typically above 0.20mm.
The health of the meibomian glands is currently thought to be one of the most critical elements in assessing the status of the ocular surface. MGD is associated with reduced production of lipid for the tear film and is considered the primary cause of dry eye disease. This topography system has the capability to capture infrared images of the meibomian glands of the upper and lower lid (Figure 2). Enhancement software makes gland detection more obvious. These images can show dropout of meibomian glands associated with MGD.

Endothelial Cell Assessment via Specular Microscopy The corneal endothelium is a single layer of cells that function to maintain the thickness and clarity of the cornea. By continually “pumping” water out of the stroma into the anterior chamber, the endothelium offsets the natural tendency of the cornea to imbibe water. Without proper functioning of the endothelium, the cornea thickens significantly and eventually loses its transparency. Such is the case in significant endothelial disease such as Fuchs’ dystrophy.
A key, yet often overlooked, form of endothelial disease is associated with long-term contact lens wear, especially if associated with subsequent chronic hypoxia. Contact lens-induced endotheliopathy is a potentially serious condition that needs to be identified and addressed in its early phases to avoid long-term clinical implications (Figure 3). In recent years, clinically applicable forms of specular microscopy have allowed clinicians to identify corneal endotheliopathy associated with corneal diseases, contact lens wear, trauma, inflammatory eye diseases, and other conditions. Specular microscopy will provide data on endothelial cell density, cell size variation, and cell shape variation as well as central corneal thickness measures. Abnormalities in corneal cell size variability are referred to as polymegethism. A low percentage of normal, hexagonal cell shape is referred to as pleomorphism. Finally, cell density can be reduced beyond normal age-related decreases in the presence of conditions that result in endotheliopathy.

Baseline specular microscopic imaging/analysis is a useful technique for all contact lens wearers. Periodic repeat imaging is dependent on the risk factors for the development of corneal hypoxia. These risks include the use of continuous or overnight wear of contact lenses, thick lens designs, and/or lenses fabricated from lower-oxygen-transmissible materials as well as corneas at risk for hypoxic sequelae and other causes of endotheliopathy.
Confocal Microscopy This imaging technology has developed as a highly useful technique for the detailed study of corneal cellular structure. The basic principle of a confocal microscope involves a single point source of illumination on a single point of tissue that is simultaneously imaged by a camera in the same plane, hence the term “confocal.” Confocal microscopy is a powerful diagnostic technique that allows non-invasive microscopic examination of the cornea. However, until recently, use in clinical practice has been limited to research centers. New developments in technology have made confocal microscopy available to clinical practitioners.
The applications of confocal microscopy in ophthalmic practice are numerous and expanding as the value of these high-resolution images is realized. For example, confocal microscopy can be used to identify the causative organism in patients who have infective keratitis such as Acanthamoeba keratitis and other causes of contact lens-related keratitis. Confocal microscopy also seems to have relevance in the deeper understanding of keratoconus, glaucoma, and dry eye/ocular surface disease. It is highly applicable to the detection of corneal anomalies induced by contact lens wear. Confocal microscopy continues to develop, and researchers are discovering more about a variety of diseases and conditions through the use of this technology.
MANAGING REGULAR CORNEAS WITH TOPOGRAPHY-BASED FITTING SOFTWARE FOR CORNEAL GP LENSES
Using corneal topography for the “virtual” design of corneal rigid contact lenses is one of many software suites provided by topography manufacturers. Most contact lens fitting and simulation software programs have a number of common properties. Contact lens fitting software programs will typically have a library of proprietary lens designs available and can either suggest a specific lens design for an individual topography map, or practitioners can select a lens design from the available choices and apply it to the topography map. The software will suggest the most appropriate parameters of that lens design for that cornea; however, practitioners can change and manipulate multiple lens parameters to achieve the desired fitting relationship. Alternatively, practitioners can “custom” design a lens by determining all of the key lens parameters.
Typically, the software will provide a simulated fluorescein pattern that will change as lens parameters are modified in the program (Figures 4 and 5). The software will also calculate posterior to anterior lens-to-cornea fitting relationships in terms of microns of clearance between the two surfaces. These measures can be calculated along any meridian of the cornea. Analysis of such data allows practitioners to see central, peripheral, and edge clearance for 360º.

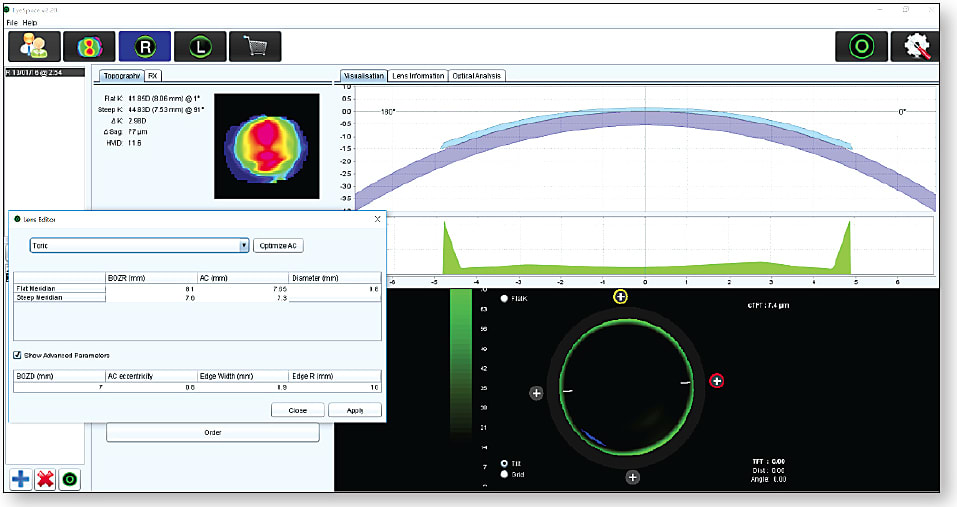
In addition to the physical fitting characteristics of the virtually fit lens, the software can assist in determining the optical power properties based upon entered refractive data and vertex distance. Changes in base curve can immediately be calculated in terms of the effect on the required optical power parameters.
MANAGING IRREGULAR CORNEAS WITH ADVANCED CORNEAL SHAPE ANALYSIS
An appropriate understanding of the complex nature of corneal shape in cases of diseases and conditions associated with irregular corneas not only results in superior fitting of contact lenses, it also allows for a far more comprehensive understanding of the disease or condition entity. Various advanced technologies provide us with an amazingly detailed depiction of these corneas.
Placido Corneal Topography This is a reflection-based and curvature-based method to portray the anterior surface of the cornea. The instrument will project concentric light rings onto the anterior surface of the cornea (more specifically onto the anterior surface of the pre-corneal tear film). The image of the reflected rings is captured, and the computer analyzes the spacing between the rings. Closer rings suggest steeper curvature, and more separated rings suggest flatter curvature. This curvature-derived data can be displayed in many ways and can be interpolated to suggest elevation data.
However, Placido topographers can never provide true elevation data, nor do they provide any information about the posterior corneal surface or the overall/global corneal thickness. Many corneal diseases and conditions must be analyzed for these measures to fully understand how those corneas are shaped.
Elevation-Based Scheimpflug Tomography Tomography is a two- dimensional slice through a three-dimensional object. Anterior segment tomographers utilize a widely known and time proven photographic method termed Scheimpflug imaging that expands the depth of focus. It provides a 360º image of the anterior segment via a rotating Scheimpflug camera. This provides true elevation data of both the anterior and posterior corneal surfaces and also is able to measure the entire corneal surface thickness, thus providing a global optical pachymetry map. Curvature data can be derived quite accurately from elevation data as well (Figure 6).

In addition, these systems can image out onto the sclera and deeper into the anterior chamber and the crystalline lens. The result is that with the extensive analysis software available with these systems, a comprehensive evaluation of the anterior segment can be obtained (Figure 7). The applications are amazingly diverse. Most specific to cornea and contact lenses, these systems provide detailed data for disease diagnosis, monitoring of disease progression, and evaluation of shape in the designing of corneal and scleral contact lenses.

Anterior Segment Optical Coherence Tomography (AS-OCT) AS-OCT provides exquisite images of the cornea and other structures of the anterior segment of the eye. Not only can we obtain these images for viewing, but we can use various tools provided within the systems to measure various elements of anterior segment structures, such as corneal diameter, corneal sagittal height, corneo-scleral sagittal height, anterior chamber angles, anterior chamber depth, and many more (Figure 8). Developing software programs are now allowing us to measure not only global corneal thickness, but also epithelial and stromal thickness. Normative database analysis will soon enable us to identify patients who are, for example, suspects for early keratoconus.
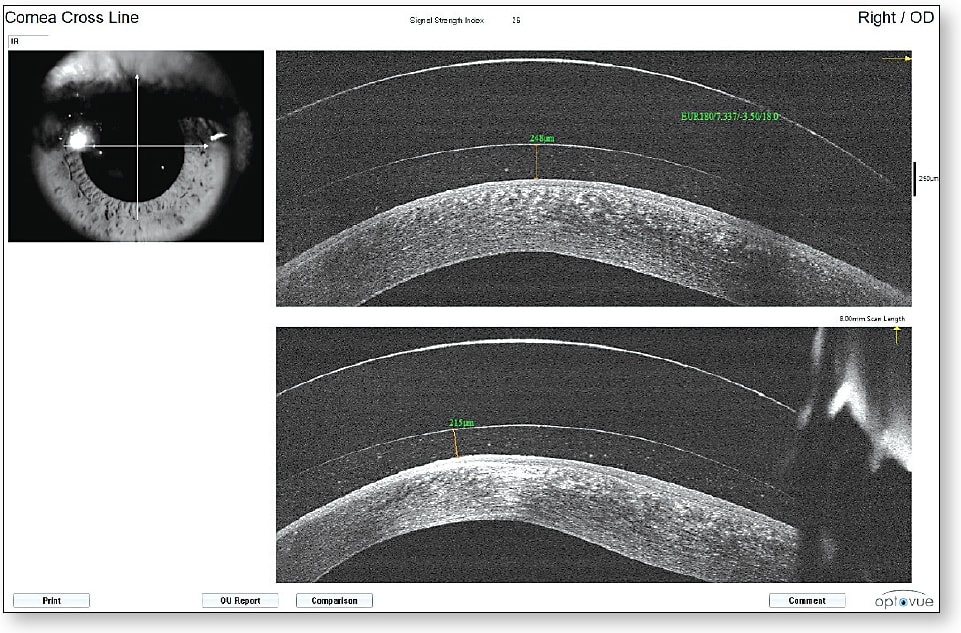
There has been a dramatic expansion in the use of AS-OCT to evaluate the fitting characteristics of vaulting contact lenses such as scleral lenses and vaulting hybrid lenses. Precise measurements of the retro-lens tear layer and the landing areas of these lenses allow practitioners to far more precisely establish optimal fitting relationships (Figure 9). We have come to further understand that the vaulting and landing appearance at initial dispensing of these contact lenses can significantly change following hours of settling on the eye. AS-OCT allows us to quantify this settling phenomenon. In fact, new software programs for AS-OCT are allowing the systems to automate the vaulting measurements without having to manually measure various areas of lens vault (Figure 10). In essence, AS-OCT is revolutionizing the assessment of vaulting contact lenses, and the technology is being developed that will allow for virtual fitting of such lenses from AS-OCT measurements.


MANAGING THE MYOPIC EYE WITH CORNEAL RESHAPING ASSISTED BY ADVANCED TECHNOLOGY
As evidence continues to mount supporting the efficacy of corneal reshaping in the control of myopia progression, more and more practitioners are embracing this highly effective treatment modality. Freedom from daytime wearing of ocular appliances, along with the potential for myopia progression control, makes corneal reshaping a very attractive option for our patients.
Advanced technologies come into play in a variety of ways with corneal reshaping. Of course, all of the technologies mentioned previously in regard to establishing ocular health status prior to contact lens fitting apply. The use of corneal topography or Scheimpflug tomography becomes critical in corneal reshaping, in part to establish a baseline for anterior corneal shape and to some degree for determining whether a patient is a good candidate (by evaluating corneal curvature, asphericity, and diameter in relation to the desired refractive correction). Its greatest value is in comparing pre-treatment to post-treatment maps, which will clearly show the influence of these contact lenses on the corneal shape (Figure 11). Evaluating the treatment centration, size, and shape provides critical direction for any required modifications to optimize outcomes.

Finally, there are programs within these instruments that can automate the fitting process in a way similar to how other programs can be used to fit traditional corneal rigid lenses on normal corneas (Figure 12). Additional advanced technologies that are applicable to corneal reshaping, and specifically to myopia progression management, include measurements of axial length. Both ultrasound and optical systems are now available and are being more commonly incorporated into the myopia management armamentarium.

CORNEO-SCLERAL PROFILE SYSTEMS FOR CUSTOMIZED SCLERAL LENS DESIGN
Just as technologies have been developed that successfully allow us to virtually fit corneal GP contact lenses, we now are expanding into the measurement of corneo-scleral profiles and shapes that allow us to design larger contact lenses that are intended to vault the cornea and land on the bulbar conjunctiva overlying the sclera. We have come to know that both the corneal and scleral surfaces are asymmetrically toric in most cases. Because vaulting large-diameter lenses land on the scleral surface, understanding the scleral profile becomes quite important, even if the entire cornea is vaulted by the contact lens.
Two stand-alone corneo-scleral profile systems are currently available. More recently, systems are being developed as adjuncts to existing diagnostic instruments that also are measuring the corneo-scleral profile (Figure 13). Finally, direct measurement of the anterior ocular surface is possible through taking an impression, which can be used to design a totally customized scleral prosthetic lens. These technologies have the potential to revolutionize contact lens fitting. Time will tell.

OPTIMIZE YOUR CONTACT LENS FITTING
Although advanced technologies are not mandatory for contact lens fitting, they surely advance our ability to provide the best contact lens options for our patients in terms of optimizing their vision and comfort while maintaining excellence in physiological response. We all need to embrace these technologies and continue to move our field forward. CLS
REFERENCES
- Report of the International Dry Eye WorkShop. Ocul Surf. 2007 Apr;5:65-204.
- Tomlinson A, Khanal S, Ramaesh K, Diaper C, McFadyen A. Tear film osmolarity: determination of a referent for dry eye diagnosis. Invest Ophthalmol Vis Sci. 2006 Oct;47:4309-4315.
- www.quidel.com/immunoassays/inflammadry .





