There’s an old riddle: “If April showers bring May flowers, what do May flowers bring?” If you ask an eyecare practitioner for the answer, the response is likely to be itchy, red eyes.
During the spring, increasing mold and pollen counts bring potential misery to allergy sufferers. According to the Centers for Disease Control and Prevention (CDC), allergies are the sixth leading cause of chronic illness in the United States, affecting more than 50 million people each year (CDC, 2011). In addition to allergic rhinitis, commonly referred to as hay fever, studies indicate up to 40% of the population is affected by ocular allergies (Singh et al, 2010).
It has been well documented that discomfort is the leading cause for contact lens dropout (Rumpakis, 2010; Pritchard et al, 1999). Although the spectrum of allergic eye disease is broad, even mild presentations can negatively impact contact lens comfort, leading to reduced wear time and eventual intolerance. Fortunately, this scenario is avoidable with proper identification and management of ocular allergies.
IDENTIFYING OCULAR ALLERGIES
Despite its frequency, ocular allergy can easily be overlooked. For many individuals, allergies are a burdensome seasonal annoyance. Too often, patients ignore their symptoms or eyecare practitioners fail to ask about them, especially if the examination does not occur during allergy season. In response to the question of “Do your eyes ever itch or get red?” patients tend to downplay their answer.
However, follow-up questioning about the use of topical or oral allergy medications throughout the year may reveal symptomatic allergies. Patients also inadequately self-treat with over-the-counter (OTC) medications, potentially exacerbating comorbidities such as dry eye disease. Therefore, a thorough case history and careful examination comprise the best method for diagnosing allergic eye disease. In addition, using a standardized ocular surface symptom survey can also elicit symptoms and help differentiate between allergy and other causes of ocular surface disease.
Allergic Conjunctivitis The most common ocular allergy that eyecare practitioners will encounter is allergic conjunctivitis, which is further classified into seasonal (SAC) or perennial (PAC). SAC typically occurs during the spring and fall when pollens and molds are more abundant and ragweed is in bloom, while year-round exposure to dust mites and animal dander are the usual culprits for PAC (Bielory, 2000). In some regions of the United States, allergy seasons don’t necessarily occur in the spring and fall, such as in Texas with pine allergies. Both conditions are typically bilateral and affect patients of all ages.
The hallmark symptom of allergic conjunctivitis is itching, most notably near the nasal canthus where histamine and other inflammatory mediators pool in the tear film before draining through the nasolacrimal duct system. Other symptoms include burning, foreign body sensation, and a watery discharge (Ackerman et al, 2016). These symptoms often overlap with ocular surface disease, so clinical presentation cannot be ignored.
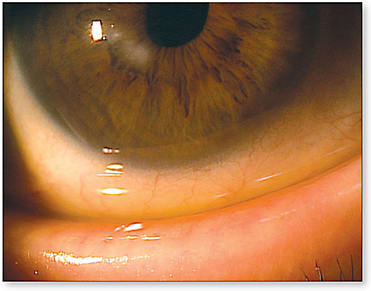
Clinical presentation of both SAC and PAC are similar; however, the signs and symptoms of PAC tend to be milder (McGill et al, 1998). Examination of the bulbar conjunctiva will reveal hyperemia and chemosis. While a fine papillary reaction of the palpebral conjunctiva is common, the presence of follicles may indicate a chronic condition (Figure 1). In moderate-to-severe cases, the eyelid becomes edematous, potentially causing periocular venous congestion and the appearance of dark rings around the eyes (Bielory, 2000; Adamczyk, 2008).

Giant Papillary Conjunctivitis (GPC) Commonly referred to as contact lens-induced papillary conjunctivitis (CLPC), GPC is a growing problem in contact lens wearers. In addition to causing mechanical microtrauma, reusable soft contact lenses introduce lens-bound antigens to the superior palpebral conjunctiva (Katelaris, 1999). This repeated interaction results in an immune response characteristic of both an inflammatory and a hypersensitivity reaction (McGill et al, 1998).
Patients who have GPC will present complaining of increasing contact lens intolerance, itching, blurry vision, and a stringy, mucous-like discharge. In early stages, symptoms can occur before clinical signs are present (Donshik, 1994). Despite varying levels of discomfort, the bulbar conjunctiva can be white and quiet. Diagnosis is confirmed by everting the upper eyelid to reveal conjunctival hyperemia and large papillae, typically 1.0mm in size or greater (Katelaris, 1998; Donshik, 1994) (Figure 2). Instillation of sodium fluorescein (NaFl) can aid in detection, as the NaFl will pool between papillae (Doughty et al, 1995). Evaluation of a contact lens on eye may demonstrate excessive movement, as the lens can be pulled upward by the papillary reaction (Donshik, 1994).

Vernal Keratoconjunctivitis (VKC) A less common, but more severe form of allergic eye disease is VKC. VKC is a seasonal condition with the highest occurrence during the spring in geographically warmer climates. Typically affecting males more than females, onset occurs during childhood and adolescence in individuals predisposed to atopy (Kumar, 2009).
The hallmark symptom of VKC is intense itching, but it may also present with foreign body sensation, photophobia, and a mucous discharge (Kumar, 2009; Leonardi, 2013). Similar to GPC, everting the upper eyelid will reveal giant cobblestone papillae; however, these occur in the absence of contact lens wear or other mechanical trauma. Unlike GPC and SAC, VKC can also affect the cornea.
With VKC, papillae can also form at the corneal limbus. Known as Horner-Trantas dots, these grey-white gelatinous nodules are a collection of eosinophils (Adamczyk, 2008). Corneal involvement may also include pannus or superficial punctate epitheliopathy. In severe cases of VKC, a coalescence of the punctate keratopathy, in conjunction with mechanical trauma from the cobblestone papillae, can cause the formation of a sterile shield ulcer (Kumar, 2009; Adamczyk, 2008).
Atopic Keratoconjunctivitis (AKC) Although its clinical presentation can be similar to VKC, AKC is another serious form of allergic eye disease. AKC affects adults, with a peak incidence between ages 30 to 50 (Bielory, 2010). Patients who have AKC also commonly suffer from other atopic diseases including eczema, asthma, and allergic rhinitis (Guglielmetti, 2010). Additionally, there is an association with anterior polar cataracts and keratoconus (Tuft, 1991). Eye rubbing is considered to be associated with keratoconus, which may explain its association to AKC (McMonnies and Boneham, 2003).
With AKC, itching is a common complaint; however, burning can be described as the more severe symptom (Bielory and Bielory, 2010; Karpecki, 2012). In addition to conjunctival chemosis, hyperemia, and giant papillae, evaluation of the eyelids may reveal staphylococcal blepharitis, meibomian gland dysfunction, ectropion, or periorbital dermatitis (Adamczyk, 2008). In severe cases, corneal involvement becomes devastating. Beginning as a superficial punctate keratopathy, there is a high risk of corneal ulceration and scarring (Figure 3). Filamentary keratitis, herpes simplex keratitis, and limbal stem cell deficiency may also develop (Batta, 2013).
PATHOPHYSIOLOGY OF THE ALLERGIC CASCADE
An allergic reaction, or hypersensitivity, is an abnormal immune response to an antigen, or foreign substance to the body. There are four classifications of hypersensitivity; however, ocular allergies are predominantly localized type I or type IV hypersensitivities.
When the body is first exposed to an antigen, such as pollen, ragweed, or animal dander, it is taken to a lymph node by antigen-presenting cells. There, the antigen binds to CD4+ T cells, which later become T helper (Th2) cells. Th2 cells release the cytokine interleukin-4, signaling B-lymphocytes to produce antigen-specific immunoglobulin E antibodies (IgE). IgE then binds to circulating mast cells, sensitizing them for subsequent exposure to the allergen. Meanwhile, other cytokines are activating basophils and eosinophils to assist with the allergic response (Bielory et al, 2016).
Following secondary exposure to an allergen, IgE bound to mast cells are cross-linked, initiating an allergic cascade characterized by two phases. First, mast cells degranulate, releasing histamine, preformed inflammatory mediators, and cytokines into the tear film and surrounding tissue. In this early phase, histamine binds to H1 receptors in both vascular tissue and sensory neurons of the conjunctiva, resulting in increased vascular permeability, vasodilation, and sensory nerve stimulation (Leonardi, 2000). This produces the hyperemia, edema, itching, and reflex tearing that is characteristic of ocular allergies.
Several hours after mast cell degranulation, inflammatory mediators, including leukotrienes and prostaglandins, are still being released along with various cytokines. These cytokines attract more neutrophils, eosinophils, and macrophages to the area, potentiating a chronic inflammatory response. Effects of this late phase can last months after the allergen exposure (Bielory et al, 2016).
The late phase of a type I hypersensitivity should not be confused with the delayed reaction of a type IV hypersensitivity. A type IV hypersensitivity is a T cell-mediated response occurring 12 to 72 hours after exposure (Adamczyk and Jaanus, 2008). Certain antigens cause CD4+ T cells to release IL-2 and interferon gamma, activating cytotoxic CD8+ T cells. Although acute contact dermatitis is the primary type IV hypersensitivity affecting periorbital tissue, T cells contribute to inflammation in chronic allergic conditions (McGill, 1998).
THERAPEUTIC MANAGEMENT
When faced with symptoms of ocular allergies, many patients self-treat first, often selecting ocular decongestants containing naphazoline, tetrahydrozoline, or oxymetazoline. They are not only the most commonly found OTC topical agents, but also the least expensive. Advertised to “get the red out” and provide eye allergy relief, they unfortunately provide only a palliative benefit.
These adrenergic agonists bind to α-adrenergic receptors in the conjunctival tissue, causing vasoconstriction and the reduction of conjunctival hyperemia and chemosis (Abelson et al, 1980). While the onset of action occurs within minutes, the duration is only three to four hours, requiring dosing up to four times daily (Adamczyk and Jaanus, 2008). The potential long-term side effects of adrenergic agonists include pupil dilation and medicamentosa, making more frequent dosing or chronic use a concern (Adamczyk and Jaanus, 2008). Rebound hyperemia and the resultant patient urge to increase frequency of dosing can prove to be a vicious cycle that is very difficult to break clinically.
Dual Action Topical Agents Historically, antihistamines and mast cell stabilizers were prescribed as monotherapy, each targeting specific points of the allergic cascade. Antihistamines reduce allergy symptoms by inhibiting the physiological action of histamine. First-generation topical antihistamines antazoline phosphate and pheniramine maleate are only available in combination with the decongestant naphazoline. These OTC formulations include the popular brand names Vasocon-A (Novartis Ophthalmics), Naphcon-A (Alcon Laboratories, Inc.), Visine-A (McNeill Consumer Healthcare), and Opcon-A (Bausch + Lomb [B+L]). Again, rebound hyperemia is of primary concern with these agents. Second-generation topical antihistamines including azelastine, ketotifen, and olopatadine have a selective affinity for H1 receptors in addition to a mast cell stabilizing effect (Kumar, 2009; Ackerman, 2016)
Mast cell stabilizers inhibit mast cell degranulation, preventing the release of inflammatory mediators (namely histamine) into the tissue. Because they have no ability to counter the effect of already released mediators, these agents are best used for prophylaxis and for more chronic conditions like VKC (Leonardi, 2013).
There are several topical mast cell stabilizers available by prescription including nedocromil sodium 2% (Alocril, Allergan), lodoxamide tromethamine 0.1% (Alomide, Alcon), and cromolyn sodium 4% (Opticrom, Allergan); however, given the wide availability of dual action agents, there is minimal clinical benefit to using them as monotherapy.
Currently, there are multiple topical second-generation antihistamine-mast cell stabilizing combinations available. These agents provide both rapid relief of itching and a long-term prevention of symptoms. Dosing is typically twice daily, but newer additions to the market have the benefit of once-daily dosage. In addition to prescription combination agents (Table 1), ketotifen fumarate is available OTC with a variety of trade names including Alaway (B+L) and Zaditor (Alcon) (both 0.025%), Claritin Eye (Merck & Co., Inc.), and Refresh Eye Itch Relief (Allergan).
| BRAND NAME | GENERIC NAME | MANUFACTURER | SIZE | DOSING |
|---|---|---|---|---|
| Elestat | epinastine hydrochloride 0.05% | Allergan | 5 mL | BID |
| n/a | olopatadine hydrochloride 0.1% | Apotex | 5 mL | BID |
| Pataday | olopatadine hydrochloride 0.2% | Alcon | 2.5 mL | QD |
| Pazeo | olopatadine hydrochloride 0.7% | Alcon | 2.5 mL | QD |
| Lastacaft | alcaftadine 0.25% | Allergan | 3 mL | QD |
| Bepreve | bepotastine besilate 1.5% | Bausch + Lomb | 5 mL, 10 mL | BID |
Topical Anti-Inflammatories In moderate-to-severe presentations of ocular allergies, the secondary inflammatory response, mediated by prostaglandins and leukotrienes, plays a more significant role. As part of the arachidonic acid pathway, these mediators can be inhibited by topical corticosteroids (Ackerman, 2016). Soft steroids such as loteprednol etabonate 0.2%, loteprednol etabonate 0.5%, or fluoromethalone 0.1% are effective for short-term pulsing. Long-term use is usually not required and includes side effects of increased intraocular pressure and cataract formation. Dosing may vary, but a typical protocol is four times daily for one to two weeks or until the inflammation is resolved, followed by a twice-daily taper for another week. After discontinuation of the steroid, combination agents can be prescribed for long-term control.
No longer commonly used, the topical nonsteroidal anti-inflammatory ketorolac tromethamine 0.4% (Acular LS Rx, Allergan) is approved to treat SAC. Ketorolac can reduce itching by inhibiting cyclooxygenase and the formation of prostaglandins. Chronic use of topical nonsteroidal anti-inflammatory drugs (NSAIDs), however, can cause corneal toxicity and reported cases of corneal melt (Flach, 2001).
Immunomodulators including topical cyclosporine 0.05% and tacrolimus 0.03% can also be used off-label to control chronic allergic conditions such as VKC and AKC. In particular, cyclosporine is effective in the treatment of shield ulcers in VKC (Leonardi, 2013).
Oral Antihistamines For atopic individuals, OTC oral antihistamines are a staple of allergy management. First-generation oral antihistamines are lipid soluble, thus able to cross the blood-brain barrier and affect the central nervous system (Simons and Simons, 2008). The most common first-generation antihistamine diphenhydramine (Benadryl, McNeil) has a strong sedative effect, while second-generation antihistamines including fexofenadine HCl (Allegra, Chattem Inc.), loratadine (Claritin), and cetirizine HCl (Zyrtec, McNeil) lack the sedative effect. The anticholinergic effect, however, decreases the secretion of tears and mucus, leading to dry eye symptoms (Ackerman, 2016).
THE ROLE OF ALLERGY AND OCULAR SURFACE DISEASE
The signs and symptoms of ocular allergies often present similarly to other forms of ocular surface disease. Ocular surface disease has come to encompass any condition altering the normal physiology of the cornea and conjunctiva, with the most notable being dry eye and blepharitis.
Case history can assist in distinguishing between symptoms of ocular surface disease and allergies. In both conditions, the eyes may be irritated and red, with watery discharge. The hallmark of allergy is itching, so the absence of this symptom requires other comorbidities to be evaluated. When itching is present, location can differentiate between blepharitis, Demodex, and allergic conjunctivitis. Itching from allergic conjunctivitis tends to be worse toward the nasal canthus, while diffuse itching around the base of the eyelashes is more likely to be indicative of blepharitis, in particular Demodex infestation (Figure 4).

The tear film plays an important role in both allergies and ocular surface disease, so it’s no surprise that these conditions not only coexist, but also exacerbate one another. Atopic patients who have concomitant dry eye disease lack a sufficient, stable tear film, causing a higher concentration of allergens, histamine, and other inflammatory mediators in the tear film. Many of those same allergy mediators also potentiate inflammation in dry eye disease. Additionally, if patients use oral antihistamines, tear production can be decreased.
If the diagnosis is more ambiguous, tear osmolarity and the inflammatory marker MMP-9 can be measured by collecting tear film samples. For example, a lower tear osmolarity may point toward a diagnosis other than dry eye disease. Conversely, a high osmolarity combined with elevated MMP-9 is typically a result of dry eye disease with an inflammatory component (Schargus et al, 2015).
AVOID CONTACT LENS DROPOUT
With the threat of contact lens dropout looming, one of the goals of allergy management should be the preservation of comfortable contact lens wear. When faced with contact lens discomfort, the first instinct of many eyecare practitioners is to change the contact lens modality or care solutions. While this approach may lessen symptoms, it will not eliminate them entirely.
The most obvious and effective means to combat ocular allergies is the complete avoidance of offending allergens. Because contact lenses serve as a vehicle for introducing allergens to the ocular surface, temporary discontinuation of contact lens wear can reduce the allergen load. Once symptoms are controlled with topical therapeutics, contact lens wear can be resumed.
If a patient is struggling with ocular allergies of any kind, this provides a great opportunity to discuss daily disposable lenses. More frequent replacement of lenses reduces exposure to lens-bound antigens and contact lens care solution preservatives. If the patient is averse to year-round daily disposables, consider seasonal prescribing.
When daily disposables are not an option, compliance with lens care and hygiene is of the utmost importance. Extended wear should be contraindicated, as higher levels of inflammatory mediators may be found in the tear film. If using a multipurpose solution, patients should be instructed to rub and rinse to remove allergens from the lens surface.
Generic solutions should be avoided because of their varying compositions and preservatives. Some patients can develop a preservative toxicity, causing irritation, hyperemia, and chemosis resembling allergic conjunctivitis (Carnt et al, 2007). A preservative toxicity presents with a diffuse punctate epitheliopathy, so NaFl staining can aid in diagnosis. Preservative-free hydrogen peroxide solutions offer superior cleaning and disinfection compared to multipurpose solutions and should be recommended to non-daily disposable patients.
Patients who require topical therapeutics for maintenance therapy are not excluded from contact lens wear. It is recommended that eye drops be instilled 10 to 15 minutes prior to applying contact lenses. Preservative-free artificial tears can also be instilled prior to contact lens application and post removal to help dilute and flush the ocular surface of allergens.
CONCLUSION
SAC and GPC are the most commonly encountered forms of ocular allergy by eyecare practitioners. Luckily, there is an arsenal of topical therapeutics available to manage these conditions. Temporary discontinuation of contact lenses, while aggressively treating with topical corticosteroids and combination agents, typically provide quick relief of symptoms. Once contact lens wear is resumed, strong consideration should be made for the use of daily disposable lenses, if possible. Eyecare practitioners should consider appointing these patients ahead of their peak allergy season to get treatment started prior to the explosion of the inflammatory and allergic cascades. CLS
For references, please visit www.clspectrum.com/references and click on document #258.





