Evaporative Dry Eye Post-Eyelid Surgery
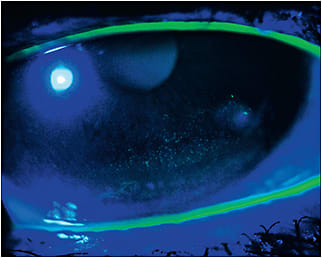
This image shows a case of evaporative dry eye with mild exposure keratitis and erosion.
Case History
This was a result of plastic surgery of the eyelid in a 56-year-old patient. She underwent the procedure two years ago and also had Botox injected twice since the surgery. The condition was further aggravated by only partial eye closure while the patient slept and because of intensive computer and air conditioner use in the summer.
She went to her ophthalmologist complaining of intense photophobia and ocular pain. The first doctor prescribed carboxymethylcellulose q.i.d., which initially offered some relief; however, in a few months, the symptoms returned and got worse. The patient then went to another doctor to get a second opinion; he tried different concentrations of preservative-free artificial tears, but none seemed to heal the corneal epithelium.
The patient was referred to our clinic for alternative treatment of the condition. The referring doctor suggested overnight scleral lens wear as therapeutic treatment. After careful examination, we found that the condition was more severe OD and not as significant OS. The patient also complained of photophobia and pain in both eyes, but worse OD, which supported our initial findings.
Case Management
We decided against the suggestion of overnight scleral lens wear and prescribed therapeutic daily scleral lens wear of 14 to 16 hours (Figures 2 and 3). We instructed the patient to only remove the lens before sleep. It is important to mention that we fit a specialty scleral lens design with radial ventilating channels that allowed the preservative-free tear drops applied to enter the fluid. Also, the lens has significantly less thickness and mass without inducing lens flexure.


We instructed the patient to apply preservative-free ointment and also to apply small strips of 3M Micropore surgical tape before sleep to help keep the upper eyelids as closed as possible. The patient is scheduled to come in for the initial training in the first week of April, and we will instruct her to return in 10 to 15 days to reevaluate the fitting and especially the corneal epithelium to ultimately decide whether we will make any changes in the treatment.
Discussion
This case is of mild-to-moderate dry eye, as the damage to the epithelium was limited to the lower, paracentral cornea. However, we cannot underestimate the patient’s complaints. So, our points of focus are the complete healing of the corneal epithelium and making the symptoms disappear.
We estimate that it will take two to four months to achieve the desired result. If it persists, we may rethink the possibility of overnight scleral lens wear using a modified preservation-free saline solution with a different concentration. Another precaution we do in some cases is to check the endothelial cell counts (via specular microscopy) during the follow-up visits over the first few months and thereafter once every year or two.
In this case, the patient’s uncorrected visual acuity was 20/25 OU; with scleral lens wear, the visual acuity improved to 20/15 OU. As the patient is a mature presbyope, we prescribed full distance correction in the dominant eye and added +2.25D to the nondominant eye. She felt good with the overall visual acuity and tolerated the monovision. We considered the vision improvement a bonus because the principal focus and original complaints were ocular pain and photophobia. In the future, we may consider a multifocal scleral lens, although we have a considerable number of presbyopic patients who are still successful with monovision in corneal GP and scleral lenses.
Conclusion
It is always important to focus on the problem, investigate, examine, and talk to your patients to help them better understand the cause and establish the best treatment options. Then, you can also offer some additional benefits such as fitting therapeutic, monovision scleral lenses that will improve the corneal physiological health.
Luciano Bastos is the director and clinical instructor of specialty contact lenses at the Instituto de Olhos Dr. Saul Bastos (IOSB) and is the director and specialty lens consultant of Ultralentes, a small laboratory specializing in GP and scleral lens designs in Porto Alegre, RS, Brazil.



