A recent meta-analysis of refractive error distribution across the world reported astigmatism to be the most common refractive error in both children and adults.1 There are now many contact lens options for these patients who have astigmatism, from soft toric daily disposable to scleral GP contact lenses. However, patients who have high ametropia and significant amounts of astigmatism have fewer contact lens options. Yet, these patients may benefit the most from contact lenses because of poor cosmesis and induced visual aberrations through spectacle correction. Determining the contact lens that provides the best vision for these patients often requires unique fitting considerations. This article discusses the challenges and strategies in fitting contact lenses for patients who have high ametropia and astigmatism.
The first step in evaluating a patient who has astigmatism is to confirm that the patient has a regular cornea by ruling out any irregularity. This can be determined by interpreting a corneal topography map and screening for localized areas of corneal steepening. If a corneal topographer is not available, measure corneal curvatures with a manual keratometer and note any distortions in the mire pattern.
Regular astigmatism occurs when the two primary meridians are 90º apart (Figure 1). Irregular astigmatism will have the two primary meridians oblique to one another (not 90º apart) (Figure 2). Patients who have an irregular cornea will typically exhibit high refractive astigmatism and will have a distorted or warped ocular surface, creating symptoms of blurred vision with spectacles and soft contact lenses.


If a patient has regular corneal astigmatism, determine whether the astigmatism is corneal or lenticular. If the astigmatism is mostly located on the corneal surface where the amount of corneal toricity is similar to the amount of refractive astigmatism, both soft and rigid contact lenses would be good options. If the corneal surface is nearly spherical and the patient has a significant amount of refractive astigmatism, the patient’s astigmatism is primarily lenticular; in this case, the best option would be a soft toric contact lens (Table 1).
| TYPE OF ASTIGMATISM | IDEAL CL OPTION |
| Corneal |
|
| Lenticular |
|
SOFT TORIC CONTACT LENSES
Silicone hydrogel materials have reduced the number of complications from corneal hypoxia that resulted from wearing low-Dk thick contact lenses. However, mass-produced, frequent replacement soft toric contact lenses (daily, two-week, and monthly replacement) are still limited in power parameters, typically available up to –2.25D of cylinder, with a few available up to –2.75D of cylinder. These ready-made frequent replacement contact lenses also come in limited spherical powers, typically ±10.00D. Therefore, if a patient’s refractive error consists of a high spherical and astigmatism component, a custom soft toric contact lens is necessary, in which case the replacement interval is either monthly, quarterly, or annually.
Stability Soft toric contact lenses are comfortable, convenient, and relatively easy to fit. Most ready-made contact lens manufacturers offer diagnostic fitting sets or allow practitioners to order trial lenses during the evaluation period. In addition to ensuring good patient comfort, the success of soft toric contact lens fitting requires that practitioners properly assess both the on-eye rotation and the rotational stability of the lens.
It is important for soft toric contact lenses to be stable. This is particularly important in patients who have higher amounts of astigmatism in their prescription. Unstable soft toric contact lenses will either cause intermittent blur as the lens rotates into and out of position or constant blurred vision if the contact lens consistently rotates out of its normal position. If a soft toric contact lens is unstable, the fit of the lens is likely too loose; therefore, consider steepening the base curve or increasing the overall diameter if the lens is customizable.
Rotation: LARS If the soft toric contact lens is rotated, the misalignment of the correcting cylinder will cause the patient to complain about poor vision. The misalignment in optics can be adjusted for if the rotation is stable.
There are several methods to compensate for the rotation. Practitioners may employ the “Left Add, Right Subtract” (LARS) principle. This rule suggests that if a soft toric contact lens marking is misaligned or rotated to the practitioner’s left, adding the misaligned degrees of rotation to the refractive axis will compensate for the rotated optics. If the soft toric contact lens marking is misaligned or rotated to the practitioner’s right, subtract the misaligned degrees of rotation from the refractive axis to compensate for the rotated optics. To estimate the degree of rotation, most biomicroscopes will have a protractor located on the light housing. Aligning the slit beam with the lens marking will help gauge the degree of rotation (Figure 3).

An alternative is to consider the hours in an analog clock. Each clock hour is 30º; therefore, if the marking has rotated approximately one clock hour, from 6 o’clock to 7 o’clock, the lens has rotated to the practitioner’s left by 30º. A rotation to 6:30 would indicate a 15º rotation (Figure 4).

Rotation: Sphero-Cylindrical Over-Refraction (SCOR) When prescribing soft toric contact lenses with high amounts of astigmatism, even small amounts of rotation can have a large impact on the vision. Therefore, employing LARS in these circumstances may be difficult because of the precision required to measure the rotation. When empirically ordering trial contact lenses, consider ordering a contact lens with the axis at the patient’s refractive axis and then two other lenses ±10º in case the lens rotates. If multiple contact lenses have been ordered in an attempt to compensate for the rotation with little success, consider utilizing the SCOR as an alternate method to compensate for rotation.
When a SCOR exhibits an axis that is located at an oblique position to the diagnostic soft toric lens axis, the contact lens power and the SCOR act as obliquely crossed cylinders. Although you may be using an online cross-cylinder calculator, there are aspects of the SCOR to help select the appropriate lens.
First, the spherical equivalent (EDS) of the SCOR indicates whether the patient is over- or under-corrected. For example, if the SCOR is +1.00 –1.00 x 65, the patient is over-minused by +0.50D. If the EDS of the SCOR is plano, then no additional effective power is needed in the trial lens.2,3
Secondly, if the soft toric contact lens is misaligned, the SCOR reveals the degrees of rotation. Examining the amount of cylinder power in the SCOR will provide information as to the degrees of rotation of the soft toric contact lens. Assuming that the soft toric contact lens power and axis match the manifest refraction, the more that a lens is misaligned or rotated, the greater the induced cylinder power in the SCOR.4 For this reason, patients who have large amounts of astigmatism may not tolerate even small amounts of soft toric lens misalignment or rotation because this may induce blur. The amount of rotation follows the trend in Table 2.5,6
| Degrees of Rotation | Approximate Cylinder Power in SCOR |
| 10º | one-third of the cylinder power |
| 15º | one-half of the cylinder power |
| 30º | Full cylinder power |
Every 10º of contact lens misalignment will result in one-third of the correcting cylinder power present in the SCOR. For example, a soft toric contact lens with –2.25D of cylinder power that rotates 10º off axis will induce –0.75D of unwanted residual cylinder power. Similarly, if the SCOR results in –0.75D of astigmatism for a –2.25D cylinder power soft toric lens, then the new contact lens requires a 10º axis adjustment.
Lastly, the axis of the SCOR provides information on the direction to adjust the new cylinder axis. The new cylinder axis will usually be located between the trial contact lens and the SCOR axes.
CONSIDER THIS EXAMPLE:
Trial soft toric contact lens power: plano –2.00 x 090
SCOR: +0.50 –1.00 x 145
In the example above, half of the contact lens astigmatism is presented in the SCOR; therefore, a 15º power compensation is needed (Table 2). The SCOR axis indicates that the ideal axis should be between 90º and 145º; therefore, a 15º change toward 145º would properly compensate for the rotated optics. The ideal contact lens power is plano –2.00 x 105.
Other Types of SCOR It is possible that a SCOR has an axis that is not oblique, but instead 90º away from the trial contact lens axis. This is an indication that the trial contact lens is over-correcting the cylinder power, in which case decreasing the amount of cylinder power would optimize the patient’s vision.
CONSIDER THIS EXAMPLE (FIGURE 5):
Trial soft toric contact lens power: –1.00 –1.25 x 060
SCOR: plano –0.50 x 150
Ideal soft toric contact lens power: –1.50 –0.75 x 060

The axis of the SCOR is 90º away from the soft toric contact lens power. The EDS of the SCOR in the above example is –0.25DS. Therefore, the SCOR indicates that a decrease in the amount of astigmatism is warranted, as is a net power change of –0.25D.
Typically, the contact lens power should correlate with the vertexed spectacle refraction; however, when working with patients who have high refractive errors, the vertex distance will have a significant impact on the prescription. The SCOR is not as prone to vertex changes because the majority of the prescription is already incorporated in the lens.
If an exact trial lens is not available in the office, consider using the closest contact lens power in the desired brand on the patient’s eye during the initial evaluation. The use of a trial lens allows practitioners to fine-tune the contact lens power without needing to account for the vertex distance. Choose a trial lens that has the same axis as the refraction to minimize the effects of crossed cylinders during an over-refraction.
Furthermore, if a decision needs to be made between the sphere and cylinder power, consider matching the larger of the two components. A high-plus toric contact lens will interact with the eyelids differently compared to a high-minus toric contact lens. The trial lens will also allow practitioners to evaluate for potential lens rotation and thus save chair time.
CORNEAL GP LENSES
Corneal GP contact lenses provide another option for patients who have high ametropia and high refractive astigmatism. Corneal GP lens parameters are customizable and can be specified for a patient’s high prescription. This is ideal, as the patient’s prescription may not be available in soft toric contact lenses. Corneal GP lenses are also beneficial because of the inherent sharp vision that this modality provides. However, this contact lens option may not be well-suited for patients whose vocation or avocation is in dusty or windy environments or for those who plan to be part-time contact lens wearers.
When the majority of a patient’s astigmatism is due to corneal toricity, the tear lens formed by the GP contact lens and the cornea will provide the necessary correcting astigmatism power. When a patient’s astigmatism is primarily from the crystalline lens and the corneal curvatures are relatively spherical, residual astigmatism will occur with a spherical GP contact lens. In this second situation, a front-surface toric corneal GP lens is needed to correct the residual astigmatism. Front-surface toric corneal GP lenses are prism-ballasted. In high-ametropia patients, for whom the lens thickness profiles are inherently thick, the prism may further decenter the lens inferiorly.
The amount of corneal toricity determines the corneal GP contact lens design. Patients who have low amounts of corneal toricity can be fit into a spherical contact lens, and patients who have a highly toric cornea (> 2.00D) generally require a toric-back-surface or bitoric contact lens design. One benefit to a toric-back-surface corneal GP lens is that it will best contour a highly toric cornea and will optimize lens centration.
Although a spherical GP lens will mask the majority of the corneal toricity and provide optimal vision for patients, the mismatch in the spherical back surface of the lens and the toric cornea will reduce the comfort for patients and cause lens decentration. The poor centration is further complicated if patients have a high prescription, as the thicker lens profiles will have a tendency to cause the lens to position inferiorly.
If there is uncertainty as to whether a patient would benefit from a toric-back-surface design, evaluate a spherical corneal GP lens on the patient’s eye. If the fluorescein pattern is toric with peripheral edge lift, the patient may benefit from a toric-back-surface corneal GP contact lens (Figure 6).

Toric corneal GP lenses can be designed from empirical or diagnostic data. If you are prescribing toric corneal GP lenses because a patient has high sphere and cylinder power, consider designing the contact lens empirically. The patient will have a better initial experience when the corneal GP contact lens has a prescription (and base curve) closer to what the patient needs. Designing a lens from empirical data, in which the bulk of the prescription is already incorporated in the lens, also eliminates large over-refractions that are subject to small changes in vertex distance. When ordering a contact lens empirically, keratometry values and a manifest refraction are required.
A toric corneal GP empirical fitting guide that is readily available online is the Mandell-Moore fitting guide (www.gpli.info/mandell-moore ). It can be downloaded as a worksheet and requires practitioners to input a patient’s corneal curvatures and manifest refraction. This guide applies a “fit factor” based on the patient’s corneal toricity.
The “fit factor” results in a mild misalignment between the toric base curve and the toric cornea to enhance movement of the lens and promote tear exchange (i.e., it often simulates a fit of a spherical GP lens on a slightly toric—often 0.50D to 0.75D cylinder—cornea). The final base curve and power of the contact lens can quickly be calculated after incorporating the suggested “fit factor.”
Once a toric GP lens has been designed, evaluating the fit with sodium fluorescein is necessary. When fitted appropriately, a back-surface-toric or bitoric corneal GP lens on a toric cornea will have a similar fluorescein pattern appearance as would a spherical GP lens on a spherical cornea (Figure 7). If the toric GP lens is too flat, the fluorescein pattern will have a round, central area of bearing (Figure 8). If the toric GP lens is too steep, the fluorescein pattern will have a midperipheral circular area of bearing (Figure 9). To adjust for a toric GP lens that is too flat or too steep, simply flatten or steepen both base curves to achieve an optimal alignment fit, then compensate for the change in power.



FOR EXAMPLE:


If the lens is too flat by 0.50D, then the new toric GP lens should be:


If the fluorescein pattern exhibits a toric appearance, this indicates that the toricity in the base curves is insufficient (Figure 10). In this case, increase the difference in the base curves by the necessary amount to create a sphere-like alignment sodium fluorescein pattern.

FOR EXAMPLE:


If the lens exhibits a 1.00D toric appearance, then the new toric GP lens would be:


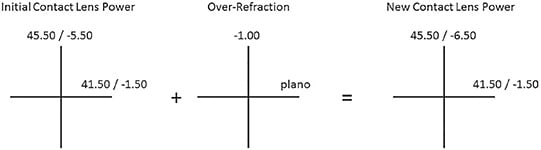
Over-refraction If the over-refraction through a back-surface toric or bitoric corneal GP lens is spherical, simply add the sphere power to each meridian of the lens.
FOR EXAMPLE:


OR: –0.50DS
New GP lens:


If performing a SCOR through a back-surface-toric or bitoric corneal GP lens, then confirm that the axis of the SCOR is the same as the axis of one of the major meridians of the corneal curvatures. If the axis is the same, then utilize an optical cross and add the cylinder power to the contact lens (Figure 11).
FOR EXAMPLE:


SCOR: plano –1.00 x 180
Manual K: 46.50 x 42.00 @ 180
New GP lens:


If the axis of the SCOR is not the same as the axis of the major meridian, then take the EDS of the SCOR and add the resultant power to each meridian of the lens.
SPEcial Consideration A type of bitoric lens design called a spherical power effect (SPE) lens has unique properties in which the contact lens behaves like a spherical corneal GP lens on the eye. It can rotate on the eye and not induce any unwanted oblique astigmatism. An SPE contact lens is a bitoric contact lens in which the difference between the base curves and the difference between the powers are equal.
This is an example of an SPE lens:


SCLERAL GP LENSES
If a patient’s lifestyle is not compatible with corneal GP lenses but he or she still desires precise vision, scleral GP or hybrid contact lenses can be considered. Scleral lenses have become increasingly popular and are not only an option for patients who have irregular corneas, but can be a good option for patients who have normal corneas. Scleral lenses vault the entire cornea and, therefore, in patients for whom the majority of the astigmatism is on the corneal surface, scleral contact lenses can be successfully fit with a simple spherical-back-optical surface. In addition, scleral GP lenses and hybrid contact lenses have larger diameters compared to corneal GP lenses. This large diameter can help center a lens on the eye and enhance initial comfort.
When a SCOR through a scleral lens results in residual astigmatism, the cylinder power needs to be added to the front surface of the scleral lens. All front-surface toric contact lenses require a stabilizing mechanism to properly orient the contact lens. The stabilizing mechanism in a scleral lens is either a prism or, more commonly, a toric peripheral haptic. The haptic refers to the region peripheral to the central curvature of a scleral contact lens. A toric haptic indicates that one meridian of the peripheral curve is flatter compared to the other meridian. A toric haptic is usually prescribed because of the difference in sagittal height between the horizontal and vertical meridians of the sclera.7 It allows the scleral contact lens to align with the toric sclera and “lock” into place.
These toric haptics can be prescribed regardless of whether or not a patient has residual astigmatism in the SCOR. When the patient has both residual astigmatism in the SCOR and a toric sclera, the practitioner can utilize the toric haptic as the stabilizing mechanism and incorporate the astigmatism on the front surface without resorting to prism ballasting. This maintains a thinner center thickness of the scleral contact lens and enhances contact lens centration. Laser markings on the scleral contact lenses will indicate the meridians of the toric sclera, which may not coincide with the axis of the residual astigmatism. Clear communication with the scleral lens laboratory will prevent unnecessary remakes.
THE ROLE OF SPECTACLES
There are some patients who have high ametropia and a low amount of refractive astigmatism. These patients are often prescribed spherical contact lenses, but they may have a low amount of residual astigmatism that improves the quality of their vision. If a patient is wearing a high-powered spherical soft contact lens, correcting a small amount of astigmatism may require the patient to move into a quarterly replacement lens. Instead, if the patient is generally satisfied with the vision or requires sharper vision for only certain activities (such as night driving), prescribing a pair of spectacles to be worn in conjunction with the contact lenses is beneficial.
When prescribing an “overlay” pair of glasses to correct residual astigmatism, optimize the vision in the contact lens power. Doing so may reduce the occasions during which the patient is dependent on the spectacles. To confirm that the contact lens power is optimized, perform a SCOR, and confirm that the spherical equivalent is plano.
CONSIDER THIS EXAMPLE:
Soft Contact Lens Power: –18.00DS
SCOR: plano –1.00 x 090 (EDS = –0.50D)
New Contact Lens Power: –18.50DS (EDS incorporated into the new lens)
Overlay Spectacle Prescription: +0.50 –1.00 x 090 (EDS = plano)
Overlay spectacles can also be beneficial for presbyopes who require a reading prescription. In the above example, if the patient has a +1.50D add, the overlay spectacles for single-vision reading glasses would be +2.00 –1.00 x 090.
CONCLUDING THOUGHTS
Patients who have high ametropia and significant amounts of astigmatism can be successful in contact lens wear despite fewer contact lens options compared to those available for patients who have low refractive errors. The role of practitioners is to carefully interpret the examination data and understand lens design to provide the best contact lens vision and corneal physiology for each patient. CLS
REFERENCES
- Hashemi H, Fotouhi A, Yekta A, Pakzad R, Ostadimoghaddam H, Khabazkhoob M. Global and regional estimates of prevalence of refractive errors: Systematic review and meta-analysis. J Curr Ophthalmol. 2018 Sep 27;30:3-22.
- Long WF. Lens power matrices and the sum of equivalent spheres. Optom Vis Sci. 1991 Oct;68:821-822.
- Lindsay RG, Bruce AS, Brennan NA, Pianta MJ. Determining axis misalignment and power errors of toric soft lenses. ICLC. 1997 May-June;24:101-106.
- Benjamin WJ. The “explicability” of cylinder axis and power in refractions over toric soft lenses. Cont Lens Anterior Eye. 1998 May-Jun;25:89-92.
- Snyder C. A review and discussion of crossed cylinder effects and over-refractions with toric soft contact lenses. ICLC. 1989 Apr;16:113-117.
- Dain SJ. Over-refraction and axis mislocation of toric lenses. ICLC. 1979;6(2):57.
- Ritzmann M, Caroline PJ, Börret R, Korszen E. An analysis of anterior scleral shape and its role in the design and fitting of scleral contact lenses. Cont Lens Anterior Eye. 2018 Apr;41:205-213.





