For the fifth consecutive year, the American Optometric Association (AOA) Contact Lens & Cornea Section (CLCS) presented a two-hour course on the topic of clinical controversies at Optometry’s Meeting, which was most recently held from June 21 to 25, 2017 in Washington, DC. The focus of the 2017 Clinical Controversies course pertained to the applications of presbyopic lens designs for both presbyopic individuals as well as for children who can benefit from some of these designs for potential myopia control. An audience response system was used to poll eyecare practitioners (ECPs) in attendance about their preferences as they pertained to the various corrections. Many of these responses are included in this article.
THE EVOLUTION OF PRESBYOPIA CORRECTION
When analyzing the evolution of contact lenses, it is important to note that in the latter half of the 1980s to the 1990s, nonspherical progressive multifocal and diffraction contact lenses were developed, and a large number of bifocal products were released. Although these new multifocal contact lenses were a leap in optics to free presbyopes from the confines of spectacles, most practitioners were not embracing these designs as their first choice in treating presbyopia. Monovision seemed the preferred method for aging contact lens wearers until studies, like that of Woods1 in 2009, showed that multifocal lens designs (that drive binocularity) were subjectively preferred by emerging presbyopes versus practitioners objectively feeling that patients saw better out of traditional monovision lenses.
It was also found that the vision that practitioners test in the “exam lane” is not reflective of patients’ visual worlds in their everyday tasks. The study results show that we need to take our “clinical blinders” off and prescribe lenses that provide better real-world performance for the visual challenges of today’s presbyopes.
It is estimated that by the year 2020, 36% of the U.S. population will be presbyopic.2 With Baby Boomers (born 1946-1964) all firmly presbyopic, and Generation X (born 1965-1980) joining the ranks as emerging presbyopes, the need has never been greater. Yet, the number of eyecare professionals actively promoting multifocal lenses is only 6%!3
With today’s presbyopic population being active, technology-savvy individuals with the means and desire for visual freedom, the opportunity to enhance our patients’ lives is staggering. Fortunately, the advancements in current multifocal contact lens designs offer better adaptation for successful fits with decreased chair time. Our profession has a golden opportunity to change the way presbyopes see the world; we need to proactively educate patients of multifocal contact lens availability and make fitting these lenses a part of every patient care day.
A NOVEL APPROACH TO EXPLAINING PRESBYOPIA
We all have the knowledge and expertise to help our patients, but understanding the importance of patient communication and how we can use it to elevate our patients’ experiences is the next step. Our patients struggle with understanding presbyopia. They question where they are in the process, how much change is going to occur, why progressives are needed, and why they have to be changed so frequently. They believe that initiating reading assistance is a cause of their further deterioration. We have to face these questions and combat patients’ mistrust in presbyopic options because others around them have failed.
In an attempt to help patients understand presbyopia and answer all of the questions they have, a strategy can be used to explain the accommodative system. The loss of 2.50D of accommodation can be explained as a muscle losing 10 units of energy. Each unit of energy is equivalent to a 0.25D step. The rate at which we lose this energy varies from patient to patient. Using this unit system of 10, it is possible to pinpoint where in the process patients are and have them follow along as their accommodative system changes. They are able to see how many more steps of change lie ahead and hence how many more changes in glasses will be required.
For example, if patients present to the clinic with a +1.50D add, they have more than likely lost six units of their accommodative muscle energy and are running on only 40% of their initial ability. These patients would require six units of add/magnification support to reach their full potential. These six units are added to the distance prescription to give them their best reading vision. When their accommodative system is running at 100%, the rate of change could potentially slow down, and they will ultimately be more comfortable and functional. We can also show them that they have four more steps of change ahead of them.
This system has also made it very easy to explain the difference between a linear progressive design and a circular multifocal contact lens design, how they require different strategies to interpret them, and why patients who have a low add power have an easier time adapting to both progressives and multifocal lenses.
Case One A 49-year-old female presented to the office with a desire for better vision. She found herself struggling to be productive with her current correction. She was wearing soft toric lenses with +1.25D readers over top for near work. Her job involves much computer work, which is causing the majority of her eyestrain. She was a previous GP lens wearer before being refit into soft toric lenses. Her current prescription and keratometry readings are as follows (Ks; refraction):
39.75 / 43.75 x 012; +4.25 –4.25 x 013
40.00 / 44.25 x 167; +3.75 –4.00 x 165, +2.00D add
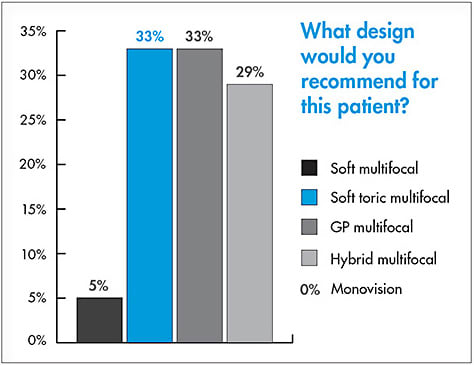
She was open to all contact lens options to help reduce strain. Given this information, the audience was polled and given five contact lens options to choose from to best fit her (Figure 1).

Although the audience preference was for soft toric multifocal lenses, the patient had prior experience with GP lenses and was open to revisiting this type of lens. There are several GP multifocal designs that are available to us. We have aspheric multifocal designs (Figure 2a) and segmented translating bifocal and trifocal designs (Figure 2b). With aspheric multifocal designs, the asphericity of a lens can be placed on the back surface of the lens, the front of the lens, or on both surfaces.

It was decided that we would fit this patient in an aspheric GP multifocal. She was a perfect candidate for these lenses because she has a medium add power requirement that we were able to comfortably correct with this design. She has a high intermediate demand, which is more challenging with a translating design. In addition, her corneal astigmatism matches her refractive astigmatism, which means that there is no residual astigmatism. Therefore, the front surface for an aspheric multifocal design can be used to incorporate the add power, and the back surface can be spherical to mask the corneal astigmatism and provide the distance power. A soft toric multifocal was not chosen, as she has a high amount of astigmatism and she desired better vision than she had with her previous soft lenses. Many patients can benefit from aspheric GP multifocal lenses including:
- Current single-vision GP lens wearers entering presbyopia
- Astigmatic presbyopes new to contact lens wear
- Soft toric contact lens patients entering presbyopia
- Soft toric multifocal lens patients who are not visually satisfied
- Post-refractive surgery presbyopes
WHAT ABOUT MONOVISION?
Monovision—in which the dominant eye is corrected for distance and the nondominant eye is corrected for near—was the first modality for the contact lens correction of presbyopia and the preferred one for most of the 50-plus years it has been in use. However, that has changed in recent years with the development and introduction of ever-improving multifocal designs. Nichols4 reported that, for presbyopes wearing contact lenses, 75% of ECPs preferred to use multifocals as their first choice, with 17% preferring monovision and 8% preferring single-vision lenses and over-spectacles. Nevertheless, monovision, on average, has been found to result in an approximate 70% success rate while providing uninterrupted vision out of each eye individually and also being easy to fit and relatively inexpensive.5 However, there can be compromised vision at each distance and negative impacts on stereopsis and night driving.5
However, monovision remains a popular option for contact lens correction of presbyopia. It is important to select individuals who are motivated for this option, educate them about the compromises inherent with this modality, and recommend an over-correction for critical distance tasks such as night driving.
Determining the dominant eye is also important. The audience was polled as to which one of six different methods they used to determine a patient’s dominant eye (Figure 3). Which eye patients use to view through an opening in their hand was clearly the preferred option. Although, the so-called “swinging flashlight” test—in which (typically) a +2.00D trial lens is viewed by each eye individually, with the most blurred eye at distance being the dominant eye—was also popular.

Case Two A 40-year-old early presbyope was resistant to wearing spectacles. She spends some time on the computer, but not an excessive amount. She has a history of cosmetic contact lens wear in the past and is interested in these lenses. She is pleased with the distance vision of her lenses without correction. Her refractive information is as follows:
Refraction: OD plano, 20/20; OS –0.25D sph
Reading Rx: +1.00D add
Keratometry: OD 42.25 / 42.75 @ 84; OS 43.00DS
Sighting Technique: Right eye dominant
Monovision was the modality selected for this patient, and the audience was polled as to why monovision would be considered in this case (Figure 4). Ease of fitting, the patient’s desire for distance vision clarity, and the patient’s visual demands were all popular choices.

Certainly, our patient’s interest in cosmetic lenses and her interest in maintaining good distance vision factored in this choice. In addition, as she is essentially emmetropic, there would not be the effects of simultaneous vision present in soft multifocal lenses. She was fit successfully into silicone hydrogel cosmetic-tinted lenses with a plano power for the lens OD and +0.75D for the lens OS.
SOFT MULTIFOCAL LENSES
As mentioned previously, multifocal designs have increased in popularity in recent years, in part as a result of the introduction of improved designs and also the convenience of a daily disposable option. Fitting of these lenses is relatively straightforward via the use of an inventory. Typically, a lens is selected that is as close to the patient’s refractive error and add power as possible; 0.25D refinements in power are often significant. The audience was polled as to what would be their preferred change if patients reported blur at near through their soft multifocals (Figure 5). Adjusting the reading prescription was the preferred option of the respondents. However, this was actually a trick question because the best option would be to use the manufacturer’s fitting guide, as every design is different.

Case Three A 47-year-old presbyope was looking for additional options. He is a businessman with a moderate amount of near work. He is athletic and often plays basketball. He currently wears a daily disposable soft lens for distance vision only. He is receptive to trying something new. His findings are as follows:
Refraction: OD –2.25 –0.50 x 175, 20/20; OS –2.50 –0.25 x 015
Reading Rx: +1.50D add
Keratometry: OD 42.25 / 43.25 @ 86; OS 42.75 / 43.50 @ 103
Sighting Technique: Right eye dominant
The question posed to the audience was why they would consider soft multifocal lenses for this patient (Figure 6). The primary reasons offered for why soft multifocal lenses should be considered are the patient’s visual demands followed by his willingness to try something new. His previous contact lens history was essentially a non-issue as far as the audience was concerned.

The patient was successfully fit into a daily disposable soft multifocal lens with a low add on the right (dominant) eye and a low add on the left (nondominant) eye.
MULTIFOCALS FOR MYOPIA CONTROL
Based on animal models6,7 and evidence presented in human clinical trials,8-12 myopic defocus is thought to be the putative cue to slow eye growth and, therefore, myopia progression. In theory, myopic defocus presented anywhere in the retina will lead to slowed eye growth. However, only myopia control using center-distance multifocal contact lenses has been reported in the peer-reviewed literature.8-14
Because available information consistently says that center-distance design multifocal contact lenses provide effective myopia control, and there is an extreme paucity of information regarding myopia control with center-near multifocal contact lenses, eyecare practitioners ought to prescribe only center-distance multifocal contact lenses for myopia control. In the United States, there are only a few center-distance multifocal contact lenses available. One of these lenses ought to be considered for myopia control.
Although no direct evidence exists to indicate that a stronger add power will provide better myopia control, indirect evidence indicates that this may be true. Eyes fit with orthokeratology contact lenses that have higher baseline myopia experience slower eye growth,15,16 and this may be because those eyes exhibit greater myopic blur in the periphery. Furthermore, there is a significant correlation between the peripheral myopic defocus and progression of refractive error at some peripheral retinal locations.8 Because higher add powers result in greater myopic blur,17 higher add powers are therefore thought to provide better myopia control. Based on what is currently known about soft multifocal contact lens myopia control, center-distance multifocal contact lenses with a high add power are thought to maximally slow eye growth and optimize myopia control.
Case Four A 7-year-old female had progressed 1.00D in myopia over the past year. The desire was to slow the progression of her nearsightedness. Her corrected visual acuities were 20/50 OD and OS, 20/40 OU at distance, and 20/20 OU at near. Other findings included the following:
Spectacle Rx: –3.75 DS OD and OS
Refraction: –5.25 DS OD and OS
Cover Test with Refraction: Ortho at distance, 12Δ XP at near
Accommodative Amplitude: 8.00D OD and OS
Near Point of Accommodation: 10.00D
Pupillary Distance (PD): 50mm
What about the convergence insufficiency? Did we make it worse by fitting a multifocal? If you calculate the AC/A ratio (the accommodative convergence AC [in prism diopters] to the stimulus to accommodation A [in diopters]), you find that it is low. (Note: H is phoria at near [N] and distance [D].)
PDcm + (HN – HD / AN – AD)
5 + (–12 – 0 / 3.00 – 0)
5 + (–4)
1Δ/D
The phoria changes by 12, and accommodation changes by 3; 12 divided by 3 is 4. Because the patient became more exophoric, subtract this from the PD, and the patient has an AC/A ratio of 1. Therefore, providing a +2.50D add will only increase exophoria by 2.5 prism diopters. You will aid the accommodative insufficiency with the add, so the patient is unlikely to now have complaints secondary to convergence insufficiency if she didn’t already.
Therefore, in this case study, a higher add power may provide better myopia control. A high add power has little effect because of the low AC/A ratio, but be sure to tell such children to return if they notice double vision, headaches, or eyestrain. In addition, most myopic children can independently care for their contact lenses.
DRY EYE
Nearly 40% of people experience dry eye symptoms on a regular basis, and dry eye is one of the most common reasons for patients to visit their eyecare practitioner.18 According to multiple studies, dry eye disease may have a considerable impact on quality of life (QOL).19,20 One study evaluated utility assessment scores to quantify the QOL of dry eye disease (DED) patients.21 Moderate dry eye had a utility score of 0.78, which is in the same range reported for moderate angina (0.75); perfect health has a utility score of 1.0, whereas death has a utility score of zero.21 The distinguishing factors of dry eye and contact lens dropout may blend. In clinical practice, it is observed that patients who have signs and symptoms of dry eye disease are more likely to experience contact lens discomfort.22 In addition, with advancing age, dry eye becomes increasingly prevalent, which may exacerbate contact lens discomfort.
In Sjögren’s syndrome, the lacrimal and salivary glands are targeted by circulation antibodies in an autoimmune process directed against muscarinic receptors within the glands.23 Sjögren’s syndrome is classified by the European-American consensus group.24 Primary Sjögren’s syndrome consists of aqueous-deficient dry eye, dry mouth in combination with autoantibodies, reduced salivary secretion, and a positive focus score on minor salivary gland biopsy. Secondary Sjögren’s syndrome consists of all of the classifications of Primary Sjögren’s syndrome combined with autoimmune connective tissue diseases, most commonly rheumatoid arthritis. Nine out of 10 patients diagnosed with Sjögren’s syndrome are women.
Aqueous deficient dry eye and dry mouth are hallmarks of Sjögren’s syndrome. Ocular surface disease in Sjögren’s syndrome is a product of lacrimal functional unit (LFU) dysfunction.25 The LFU is composed of ocular surface tissues (cornea, conjunctiva, conjunctival blood vessels, and the eyes), the main and accessory lacrimal glands, meibomian glands, conjunctival goblet and epithelial cells, and their neural connections. This network connects the sensory tissues and secretory glands that provide homeostasis of the ocular surface.
Ocular symptoms in patients who have Sjögren’s syndrome include eye irritation (foreign body sensation) that is constant and can affect their QOL as well as photophobia due to tear dysfunction and ocular surface disease.26 Other ocular symptoms include dryness, pain, stinging, burning, itching, epiphora, and blurring or interrupted vision. It has now been demonstrated that clinically significant ocular surface disease in Sjögren’s syndrome patients may be present with normal tear production and tear volume.
In addition to topical therapy (including artificial tears, lubricant ointment, autologous serum, topical cyclosporine, topical lifitegrast, or eyelid hygiene treatments), adjunctive therapies may be utilized. These include nighttime moisture eyewear, daytime dry eye relief, humidifiers, scleral lenses, and/or oral supplementation.
Case Five A 50-year-old Caucasian female was interested in contact lenses for full-time wear. She had been diagnosed more than three years prior with Sjögren’s syndrome. She had symptoms of dry mouth, ocular foreign body sensation, and intermittent red eyes. She currently wears spectacles full-time and has a history of weekly replacement contact lens wear, but ultimately discontinued due to dryness. She is a budget analyst who works at a computer and reads eight to 10 hours per day.
She was currently taking hydroxychloroquine sulfate 200mg b.i.d. (for the past 2.5 years). She uses cyclosporine 0.05% b.i.d. in both eyes, preservative-free artificial tears PRN (three times in past week), and an ocular decongestant PRN (two times in past week). A positive family history of rheumatoid arthritis was present in her mother.
With slit lamp biomicroscopy, she exhibited 2+ meibomian gland dysfunction (MGD) in both eyes. With lissamine green stain, she exhibited 2+ conjunctival staining OD and 3+ OS. Trace inferior corneal staining was present OD and 3+ inferior staining OS.
She was advised to continue cyclosporine 0.05% b.i.d. in both eyes. In addition, she was advised to use non-preserved lubricating artificial tears or a nonpreserved lubricating eye gel q.i.d. in both eyes PRN. We also recommended an overnight lubricant ointment q.h.s. in both eyes PRN. In addition, she was advised to increase her water intake, and omega-3 fatty acids were recommended. Additionally, an eyelid and eyelash cleaner was prescribed b.i.d. OD and OS for two weeks, then daily OD and OS for two weeks as well as warm compresses.
The audience was polled as to what lens design they would fit for this patient (Figure 7). Almost 80% recommended a scleral multifocal. That was what was prescribed, and it was ultimately successful with her.

Fortunately, scleral lenses are a comfortable lens option that provide excellent optics. Scleral lenses correct refractive error including myopia, hyperopia, and astigmatism, and multiple multifocal options are available. Even in the past few years, numerous multifocal designs have been introduced for patients who have corneal irregularity, ocular surface disease, and normal, healthy eyes. A supplemental benefit is that the post-lens fluid reservoir of scleral lenses bathes the ocular surface and helps soothe ocular surface disease and dry eye.
Multifocal scleral lenses are an option for all appropriate candidates. These may include patients who have corneal irregularities (e.g., keratoconus), those who have severe dry eye (e.g., Sjögren’s disease), or those who experience discomfort with other lens modalities and are interested in continuing contact lens wear.
Pupil size and best-corrected vision in each eye help guide scleral multifocal lens selection. If vision is reduced in one eye, a modified multifocal fit may be beneficial. A multifocal can be used in the eye that has better vision, and a single-vision near lens may be used in the eye with reduced vision. Visual requirements are another factor when selecting a lens design.
Once a scleral lens is fit and an over-refraction is performed, discuss the preferred lens design with the laboratory consultant. Most multifocal scleral lenses are ordered empirically, without a diagnostic lens fitting set.
It is important to set and manage realistic patient expectations when fitting multifocal scleral lenses. It is best to underpromise and overdeliver. The lenses may correct most, but not all, of the visual needs. Some specific activities may require reading glasses.
Prior to prescribing lenses, it is important to discuss the fitting process. With multifocal scleral lenses, some manufacturers recommend fitting single-vision distance lenses first to obtain the ideal fit and vision before ordering multifocal scleral lenses. Discuss the number of visits expected to obtain a successful fit and vision. The number of visits may vary; however, it may require more than two to three visits to obtain success.
THE CLCS: WORKING TO PROTECT AGAINST ILLEGAL CONTACT LENS SALES
The American Optometric Association (AOA) Contact Lens & Cornea Section (CLCS) serves optometry primarily in the capacity of being an advocate for the profession by working to help in the protection from the harms of illegal contact lens sales. This has represented a very important issue in recent years as entities attempt to not recognize contact lenses as medical devices, and the CLCS works closely with the AOA and its legal department to help enforce this.
To that end, a large and growing number of both websites and actual businesses have received cease and desist orders from the AOA legal department for the illegal selling of contact lenses. In addition, an email has been set up (stopillegalCLs@aoa.org) so that practitioners can report suspected illegal contact lens sales as well as any adverse events resulting from illegal contact lens sales.
In addition, the CLCS—in combination with the American Academy of Optometry’s Cornea, Contact Lenses and Refractive Technologies Section—has developed a website (www.contactlenssafety.org ) to inform and educate consumers about contact lens safety. The “FAQs about Contact Lens Prescriptions” is a resource that practitioners can provide to patients to help in their understanding of why contact lenses are prescription medical devices. In addition, the CLCS has educational resources to improve basic and specialty contact lens fitting skills as well as numerous student programs and benefits.
The majority of current soft multifocal contact lenses have a center-near design. The advantage of this design is improved near acuity. Center-near designs are valuable for people who require close distance work, especially digital device users for whom most of their work is up close. Different add powers may be used in each eye. Typically, a lower add power is used in the dominant eye, and a higher add power is used in the nondominant eye.
There is a huge global potential for multifocal lenses, including scleral lenses. In fact, a very small percentage of presbyopes are fit with multifocal lenses in the United States.27 Scleral lenses provide superb vision and comfort and may be an option for presbyopic patients. Fitting these lenses is a great opportunity for patients and practitioners alike and is a tremendous opportunity to develop a scleral lens practice.
SOFT TORIC MULTIFOCALS
An option of increasing interest and use in recent years is soft toric multifocals. The introduction of a lathe-cut silicone hydrogel material has allowed several laboratories to make a high-oxygen-permeable soft toric multifocal in almost any possible spherical and cylinder power as well as in any axis. This complements several lathe-cut hydrogel multifocal toric contact lens designs that have been successful.
Case Six A 49-year-old Caucasian male presented for a contact lens examination. He complained that it is difficult to walk around in visually demanding places such as a bookstore. He now needs bifocals, but would like to continue wearing contact lenses. He currently wears contact lenses only for distance and has done so for 25 years. His current lenses are monthly replacement, but he replaces them every three months. He is unable to read well out of these lenses. He also indicated that he rubs his eyes frequently due to allergies. He is a graduate student who is at a computer every day for eight to 10 hours. He is definitely interested in continuing contact lens wear with a correction for near. His current lenses are silicone hydrogel toric lenses with the following powers and visual acuities:
OD –0.50 –1.75 x 160, distance visual acuity (DVA) 20/70, near VA (NVA) J5, pinhole (PH) 20/25
OS –0.25 –1.75 x 010, DVA 20/70, NVA J1+, PH 20/25
With slit lamp biomicroscopy, both lenses exhibited a good lens-to-cornea fitting relationship. There was 10˚ of temporal rotation in both eyes. His refractive criteria was as follows:
Keratometry: OD 42.50 / 44.75 @ 082; OS 44.50 / 44.75 @ 090
Manifest refraction: OD –2.75 +1.75 x 079, 20/20; OS –3.00 +1.75 x 096, 20/20
Add: OD +1.75DS, 20/20 J1+; OS +1.75DS, 20/20 J1+
The audience was polled as to whether this patient should be fit into a soft multifocal, a soft toric multifocal, a GP multifocal, or a hybrid multifocal. The responses were almost equal between the latter three options, all astigmatism-correcting (Figure 8).
The patient was successfully fit into a daily wear hydrogel soft toric multifocal. The benefit of this design versus the other rigid options is the amount of predicted residual astigmatism (i.e., –1.50D) in the left eye. These lenses resulted in good visual acuity at distance and near. The parameters and resulting visual acuities were as follows: OD –1.25 –1.75 x 170, 20/20-2 J1; OS –1.25 –1.75 x 006, 20/15-2 J1+.
SUMMARY
It is evident that the presbyopia-correcting contact lens toolbox is becoming bigger with increasing quality and quantity of options. Stay tuned for the 2018 Clinical Controversies course at Optometry’s Meeting in which we will discuss myopia control and the current challenges presented by alternative methods of contact lens delivery. CLS
The authors would like to acknowledge current AOA Contact Lens & Cornea Section Liaison Taylor Dahms and Immediate Past AOA Contact Lens & Cornea Section Liaison Annie Lee, OD, for their assistance with this article.
REFERENCES
- Woods J, Woods CA, Fonn D. Early symptomatic presbyopes—what correction modality works best? Eye Contact Lens. 2009 Sep;35:221-226.
- Market Scope LLC. 2012 Global Presbyopia Report.
- Multi-Sponsor Surveys, Inc. The 2013 Gallup Study of the US Multifocal Contact Lens Market. MS 13039. 2014 Jan.
- Nichols JJ. Contact Lenses 2016. Contact Lens Spectrum. 2017 Jan;32:22-25, 27, 29, 55.
- Johannsdottir KR, Stelmach LB. Monovision: A review of the scientific literature. Optom Vis Sci. 2001 Sep;78:646-651.
- Smith EL 3rd, Hung LF, Huang J, Arumugam B. Effects of Local Myopic Defocus on Refractive Development in Monkeys. Optom Vis Sci. 2013 Nov;90:1176-1186.
- Smith EL 3rd, Kee CS, Ramamirtham R, Qiao-Grider Y, Hung LF. Peripheral Vision Can Influence Eye Growth and Refractive Development in Infant Monkeys. Invest Ophthalmol Vis Sci. 2005 Nov;46:3965-3972.
- Sankaridurg P, Holden B, Smith E 3rd, et al. Decrease in Rate of Myopia Progression with a Contact Lens Designed to Reduce Relative Peripheral Hyperopia: One-Year Results. Invest Ophthalmol Vis Sci. 2011 Dec;52:9362-9367.
- Walline JJ, Greiner KL, McVey ME, Jones-Jordan LA. Multifocal Contact Lens Myopia Control. Optom Vis Sci. 2013 Nov;90:1207-1214.
- Aller TA, Liu M, Wildsoet CF. Myopia Control with Bifocal Contact Lenses: A Randomized Clinical Trial. Optom Vis Sci. 2016 Apr;93:344-352.
- Anstice NS, Phillips JR. Effect of Dual-Focus Soft Contact Lens Wear on Axial Myopia Progression in Children. Ophthalmology. 2011 Jun;118:1152-1161.
- Lam CS, Tang WC, Tse DY, Tang YY, To CH. Defocus Incorporated Soft Contact (DISC) Lens Slows Myopia Progression in Hong Kong Chinese Schoolchildren: A 2-Year Randomised Clinical Trial. Br J Ophthalmol. 2014 Jan;98:40-45.
- Paune J, Morales H, Armengol J, Quevedo L, Faria-Ribeiro M, González-Méijome JM. Myopia Control with a Novel Peripheral Gradient Soft Lens and Orthokeratology: A 2-Year Clinical Trial. Biomed Res Int. 2015;2015:507572.
- Cheng X, Xu J, Chehab K, Exford J, Brennan N. Soft Contact Lenses with Positive Spherical Aberration for Myopia Control. Optom Vis Sci. 2016 Apr;93:353-366.
- Cho P, Cheung SW, Edwards M. The Longitudinal Orthokeratology Research in Children (LORIC) in Hong Kong: A Pilot Study on Refractive Changes and Myopic Control. Curr Eye Res. 2005 Jan;30:71-80.
- Santodomingo-Rubido J, Villa-Collar C, Gilmartin B, Gutiérrez-Ortega R. Factors Preventing Myopia Progression with Orthokeratology Correction. Optom Vis Sci. 2013 Nov;90:1225-1236.
- Lopes-Ferreira D, Ribeiro C, Maia R, et al. Peripheral Myopization Using a Dominant Design Multifocal Contact Lens. J Optom. 2011 Jan;4:14-21.
- Multi-Sponsor Surveys, Inc. Gallup study of dry eye sufferers. Princeton, NJ. 2005 Aug.
- Miljanović B, Dana R, Sullivan DA, Schaumberg DA. Impact of dry eye syndrome on vision-related quality of life. Am J Ophthalmol. 2007 Mar;14:409-415.
- Pflugfelder SC. Prevalence, burden, and pharmacoeconomics of dry eye disease. Am J Manag Care. 2008 Apr;14:S102-S106.
- Schiffman RM, Walt JG, Jacobsen G, Doyle JJ, Lebovics G, Sumner W. Utility assessment among patients with dry eye disease. Ophthalmology. 2003 Jul;110:1412-1419.
- Begley CG, Chalmers RL, Mitchell GL, et al. Characterization of ocular surface symptoms from optometric practices in North America. Cornea. 2001 Aug;20:610-618.
- Zoukhri D. Effect of Inflammation on Lacrimal Gland Function. Exp Eye Res. 2006 May;82:885-898.
- Vitali C, Bombardieri S, Jonsson R, et al. Classification criteria for Sjögren’s syndrome: a revised version of the European criteria proposed by the American-European consensus group. Ann Rheum Dis. 2002 Jun;61:554-558.
- Pflugfelder SC. What causes dryness in Sjögren’s syndrome patients and how can it be targeted? Expert Rev Clin Immunol. 2014 Apr;10:425-427.
- Uchino M, Schaumberg DA. Dry Eye Disease: Impact on Quality of Life and Vision. Curr Ophthalmol Rep. 2013 Jun;1:51-57.
- Morgan PB, Woods CA, Tranoudis IG, et al. International Contact Lens Prescribing in 2016. Contact Lens Spectrum. 2017 Jan;32:30-35.



