Patients may need to replace a scleral lens for a variety of reasons, including lens deposits, crazing, breakage, and fit or power changes. Duplicating the previous lens order is acceptable in some cases, but other cases require either modifications to the previous order or refitting the scleral lens to ensure continued successful wear.
Lens Replacement
If a patient is successfully wearing a scleral lens with good comfort, vision, and without secondary fit complications to the anterior ocular surface, then duplicating a replacement lens order can be the best strategy. However, if it has been a few years since the original fit, consider taking advantage of technological advances that can help improve lens function. For example, reorder a duplicate lens with a decreased center thickness, or select a higher-Dk material if there are any hypoxia-related complications. If patients have had some mild dryness or if they are a moderate/heavy depositor, then consider ordering the lens with a 90% water polyethylene glycol (PEG) treatment. If patients have recently crossed the threshold of presbyopia, they might be a candidate for multifocal optics or for monovision.
Design Modifications
There are patients who have been “successfully” wearing a scleral lens despite a less-than-ideal fit. For example, the lens may exhibit haptic compression and is difficult to remove. For these cases, reorder a lens with a flatter-haptic back surface or switch designs. As well, the lens may have uneven bearing or areas of edge lift, which can be commonly observed if a spherical-back-surface design was used to fit a toric or asymmetric anterior ocular surface. To improve the fit, reorder with back-surface haptic toricity. Finally, increased ectatic changes can decrease or eliminate central corneal clearance, requiring a steeper base curve.
Refitting
There are cases in which a complete refit of a scleral lens is warranted. Patients could be wearing a lens that fits poorly, and modifications to their current design are unrealistic.
One important element to keep in mind when considering a refit is that wearing a previous scleral contact lens temporarily changes the conjunctival scleral shape. Figure 1 shows an impression ring immediately after scleral lens removal and fading of the impression ring 30 minutes post-lens removal. A recent study showed a mean conjunctival flattening of 122 microns after scleral lens removal, with the superior quadrant having the greatest change (Consejo et al, 2018).
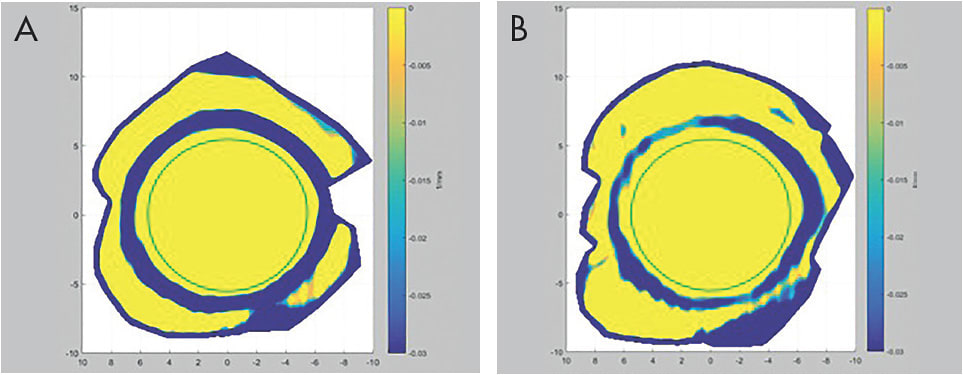
The same paper also showed increased limbal radius after scleral lens removal. Neither of these changes had completely resolved three hours post-scleral lens removal. Currently, the best advice for refitting a scleral lens is to have patients not apply the lens the day of the fitting, which will allow for overnight rebound of the bulbar conjunctiva. Evaluating a curvature map from corneo-scleral topography is valuable for determining conjunctival rebound.
Update When Needed
In some cases, an exact duplicate scleral lens makes sense. But, as technology and information continue to build, make sure that patients are up to date to maximize success and reduce complications. CLS
For references, please visit www.clspectrum.com/references and click on document #276.




