What makes something special can be different for everyone. Whatever it is, all share the trait that—according to Merriam-Webster Dictionary—it is “distinguished by some unusual quality.” The distinguishing qualities of specialty contact lenses range from offering cutting-edge care (and the personal satisfaction that accompanies it) to a healthy bottom line.
INVEST IN IDENTITY
It is a fundamental need for all humans to have a personal identity and to “fit in.” How do we see ourselves? Where do we belong in the world? What is our role? How can we make a difference?
Embracing specialty contact lens care provides eyecare practitioners with a sense of identity as contact lens experts. While much time and energy is required to truly “own” this title, the quest provides something in which eyecare practitioners can truly invest themselves and, in turn, this provides a deep sense of satisfaction. This identity as a contact lens specialist also sets practitioners apart from the competition, which helps grow their businesses.
FINANCIAL CONSIDERATIONS
However, prior to investing in any business endeavor, it is important to make sure that it makes sense financially. On this account, specialty contact lenses deliver. One study indicated that contact lenses, in general, generate 60% more income compared to spectacles alone.1 Why? Two primary factors were thought to come into play.
First, contact lens services for average patients can be, and should be, one of the many tools available to provide clear, comfortable vision to the multifaceted folks we serve. With this mindset, many patients acquire both contact lenses and spectacles to meet their needs. This generates revenues from both the contact lens and spectacle side of the practice.
Second, contact lens patients are more likely compared to spectacle wearers to develop a relationship with their provider’s office. Visits for examination and follow-up care with contact lens service tend to be more frequent than for spectacle wearers. During these visits, relationships are built, which, when done well, lead to a long-term relationship with the office. That relationship translates into increased lifetime value. This leads to continuity of care for the patients, professional fulfillment for the practitioner and staff, and a growing bottom line for the practice. Everybody wins.
In an average practice, approximately one-third of revenue is provided by vision insurance plans and one-third by medical insurers, with the remaining revenue generated by private pay.2 Many insurance plans provide limited or no coverage for contact lens services and materials. While frustrating for patients, it can be beneficial to the business. It allows the practice to set fees at a fair level that is in line with the provided services and materials.
THE CONTACT LENS COMMUNITY
Eye care can be delivered in a multitude of settings in numerous ways. Those who choose to focus on contact lens care will find a strong, vibrant, and welcoming community of like-minded individuals. Opportunities to gather and share ideas with colleagues are within easy grasp these days. National and international groups such as the American Academy of Optometry’s Section on Cornea, Contact Lenses, and Refractive Technologies, the American Optometric Association’s Contact Lens & Cornea Section, and the Scleral Lens Education Society are just a few.
In addition, contact lens meetings are held on a regular basis throughout the world, including the Global Specialty Lens Symposium, the American Academy of Optometry’s Annual Meeting, and the Bronstein Contact Lens & Cornea Seminar, among others. These meetings are not only an excellent source of education, they provide a wonderful forum for inspiration and connection with peers.
PERSONAL FULFILLMENT
Finally, specialty contact lens care offers a very direct avenue for personal fulfillment. Contact lenses can change lives and do it in an instant with the application of a lens to the ocular surface. Specialty contact lenses provide the opportunity to be a difference maker in people’s lives on a daily basis.
CHANGING AND GROWING
Part of what makes providing specialty contact lens care special and enjoyable is its ever-evolving nature. Developments in lens materials, manufacturing tools, and how we employ these devices make specialty contact lenses particularly compelling at this time.
Contact lenses entered into the digital era in March 2016 with the approval of an intraocular pressure (IOP)-monitoring contact lens.3 Numerous other digital applications are on the horizon, including enhanced night vision, diabetes and cancer detection, mood regulation, and improved contact lens correction for presbyopia.4
Elusive for many years, we are on the cusp of employing contact lenses as a drug delivery device to treat ocular allergy, inflammation, infection, and glaucoma.
One challenge has been to control the release of medication onto the ocular surface. Techniques employing nanoparticle encapsulation and molecular imprinting technology (MIT), as well as others, are offering great promise in this area.5
MAKING IT REAL
Enough about the future. What about today? High-oxygen materials combined with never-before-seen manufacturing techniques are allowing practitioners to employ specialty contact lenses in many new and innovative ways. Here are a few examples. How would you manage these cases?
Case 1: Providing Clarity and Cleanliness A 37-year-old white male and father of young children presented with bilateral keratoconus, more advanced in the left eye (Figures 1 and 2).

I had fit him with intracorneal GP lenses over a decade earlier, but refit him with scleral lenses when he developed problems with stability of the left lens. He wore his scleral lenses with good comfort and vision, but often wore his glasses because it was easier than applying the contact lenses during his “chaotic” morning activities. He had largely limited contact lens wear to outside activities and long drives.
He presented at this visit reporting a growing need to wear his scleral lenses due to higher visual demands associated with increased computer use in his new job. He had worn his lenses for two hours at the time of the visit. He had small apertures, so he had been fit with relatively small-diameter scleral lenses with parameters of OD base curve radius (BCR): 7.14mm, power: –7.00D, overall lens diameter (OAD): 15.4mm and OS BCR: 6.62mm, power: –11.50D, OAD: 15.4mm. Best-corrected vision with contact lenses in place was 20/25-1 in both the right and left eye with an over-refraction of OD –0.25DS and OS –1.00DS.
Following lens removal, best spectacle refraction was:
OD: –1.50 –2.50 x 090 20/40
OS: –16.50 –1.25 x 010 20/400
Slit lamp examination revealed classic vertical picket fence striae and corneal thinning in each eye. The cornea of the left eye also had a small raised opacity at the tip of the cone. Fortunately, the scleral lens bridged over this area adequately.
He was informed that he was responding well to contact lens wear, but a power change was recommended. New lenses were ordered incorporating the power found in the over-refraction. The lenses were dispensed two weeks later, and he was released for one year.
Nine months later, he returned reporting regular, daily scleral lens wear of 15 hours a day. He stated that his vision remained good, but he complained of increasing light sensitivity in both eyes, gradually getting worse over the prior three months. He stated he was “not sure if it is allergies.”
My impression was either that his keratoconus had progressed, leading to corneal touch to the base curve of his contact lenses, or that his lenses were coated. Visual acuity had dropped to 20/40 in the right eye and 20/30 in the left eye, unimproved by an over-refraction. The lens fit was good, with adequate central clearance over the cornea. Slit lamp findings were consistent with prior findings. However, both lenses were found to have a band of heavy central deposits (Figure 3). We then reviewed lens care and discovered that he had not been using his daily lens cleaner. His lenses were chemically cleaned in the office, proper lens care was reviewed, and he was released for one year.

Case 2: Providing Clarity and Comfort A 45-year-old patient who had granular corneal dystrophy in both eyes had been wearing daily disposable soft lenses (spherical in the right eye and toric in the left eye) for about three years. She presented with longstanding discomfort in the right eye and blurry vision in both eyes, stating “I barely passed my driver’s license test!”
Visual acuity with her soft contact lenses in place was 20/50 and 20/70 at distance and 20/100 and 20/80 at near in the right and left eyes, respectively. The over-refraction was quite variable with limited impact on vision, so scleral lenses were recommended and pursued. Reading glasses were prescribed to be worn over her contact lenses for near tasks.
Visual acuity with scleral contact lenses in place (Figure 4) improved to a stable 20/30 in the right eye and 20/20 in the left eye. Additionally, comfort of the right eye during lens wear was dramatically improved. She continued to do well with her scleral lenses at her one-week, one-month, and three-month visits. She was released and asked to return in six months.

Case 3: Providing Visual Stability A 65-year-old woman presented with complaints of variable vision suffered since undergoing radial keratotomy on each eye many years earlier. She had been prescribed glasses, but complained that her vision changed throughout the day. Even with glasses in place, she experienced constant glare and shadowing of images. She had best-corrected spectacle acuity of 20/50 and 20/40 in the right and left eyes, respectively, with the following refraction:
OD: +4.50 –1.50 x 145 +2.75 add
OS: +6.00 –1.25 x 110 +2.75 add
Slit lamp examination showed incision lines from her radial keratotomy surgery, but otherwise a healthy ocular surface.
She was fit with scleral lenses. At dispensing, the lenses appeared to fit well (Figure 5), with good comfort and vision of 20/20 in each eye. However, she returned one week later wearing her glasses. She reported frustration and difficulty applying the 16.0mm diameter scleral lenses to her eye. After numerous sessions of application and removal instruction, it was decided to refit her with reverse geometry intracorneal lenses.

Reverse geometry GP lenses of 10.0mm were fit to each eye (Figure 6), providing excellent vision, good comfort, and a healthy ocular response. Application and removal of the lenses was easily achieved by the patient with the assistance of a rubber suction cup device.

Case 4: Restoring Binocular Vision and an Occupation A 47-year-old police officer had undergone surgery for a brain tumor one year earlier. The fifth and seventh nerve were damaged, leading to facial numbness and loss of blinking control on the right side. This eventually led to the development of a neurotrophic ulcer of the right cornea, which had been treated nine months prior to his visit with a tarsorrhaphy of the right eyelid. Aside from the untoward cosmetic effects, this treatment occluded vision in his right eye. For these reasons, his surgeon recommended that he consult with me regarding the possibility of a GP contact lens on this eye. The tarsorrhaphy was released by the surgeon only two days prior to the visit to enable the evaluation. He had been aggressively instilling ocular lubricants to keep his cornea moist.
His best-corrected vision was 20/25 and 20/20 in the right and left eyes, respectively, with the following refraction:
OD: +0.75 –0.75 x 150 +1.75 add
OS: +0.25 –2.00 x 003 +1.75 add
Slit lamp examination revealed an intact epithelium with an inferior corneal opacity just peeking into the line of sight. A partial, incomplete blink was observed in the right eye.
We discussed the pros and cons of contact lens correction versus tarsorrhaphy. I shared the importance of his daily monitoring of vision and ocular redness, as his diminished ocular sensitivity robbed him of pain as an alert that things were amiss. I further explained the importance of good hygiene, proper lens and lens case care, and regular visits for follow-up assessment. He elected to pursue scleral contact lens correction of the right eye.
He has now worn a scleral lens successfully on the right eye for 2.5 years. He achieves 20/25 vision in the right eye, and by regaining binocular vision, he has been able to return to work on a limited basis as a police officer.
Case 5: From Trauma to Triumph A 68-year-old male was referred by his retinal surgeon to our office for contact lens consultation for the right eye. Ten months earlier, he had suffered blunt trauma to the right eye. This led to a retinal detachment repair four months later, followed by cataract extraction five months after that. Due to damage to the anterior chamber, no intraocular lens was inserted, leaving the patient aphakic in this eye. He presented complaining of both blur and light sensitivity in this eye.
A refraction of +10.50 –0.75 x 104 yielded acuity of 20/30+2 in the right eye. The left eye achieved 20/20 vision with –0.25 –0.75 x 070.
Fortunately, slit lamp examination of the right cornea was relatively clear, with only a small inferior nebular corneal opacity. However, the right pupil was fixed and dilated at 7.5mm. The left pupil was 3.5mm in diameter under normal room light (Figure 7).

We decided to pursue aphakic soft contact lens correction with a painted iris and occluder underlay. The laboratory providing the cosmetic treatment of the lens stated that they could not apply the painting nor the underlay to a silicone hydrogel lens, so a hydrogel lens material would be required. This provided some concern for oxygen transmission through the thick aphakic correction.
A 55% water, clear hydrogel lens was initially fitted with parameters of BCR: 8.6mm, OAD: 14.0mm, power: +11.75D. This lens provided 20/30-2 acuity with good comfort and health response, so a dry lens with these parameters was sent to the specialty laboratory for application of the iris and underlying occluder ring. The lens was accompanied by indoor and outdoor photos of the patient’s eyes taken approximately 12 inches from his face.
At dispensing, the painted iris lens appeared to fit well, but the patient returned later complaining that the “painting is not positioned correctly.” Examination revealed the lens to indeed decenter slightly temporally.
A new lens with a steeper base curve and larger diameter was ordered to improve centration in parameters of BCR: 8.4mm, OAD: 15.5mm, power: +11.75D.
The new lens was dispensed, and the patient returned one week later. He was quite pleased with his vision, comfort, and cosmesis (Figure 8). The lens had been worn for five hours on the day of the visit. The right cornea appeared clear, and pachymetry demonstrated no significant corneal swelling associated with lens wear. The patient was released for three months.

Case 6: Slowing of Myopia and Progression of Personality A quiet, withdrawn 7-year-old Caucasian girl presented to our office. Her father was a mild myopic astigmat, but her mother was highly myopic with a spectacle prescription of OD –11.50 –0.25 x 065 and OS –10.50 –1.00 x 115. Having one myopic parent increases the risk of developing myopia by two to three times. Both parents being myopic increases the risk up to six times.6
Upon examination, 20/20 vision was obtained with a refraction of OD –1.25DS and OS –1.25DS. The normal refractive error for a child of seven years old is +1.25D.7 Single-vision glasses were prescribed, and she was instructed to return in one year. At that time, her myopia had progressed by 1.00D in each eye. Glasses of the following power were prescribed, incorporating a progressive bifocal in the hopes that it would slow down the myopia progression:
OD: –2.25DS +1.50 add
OS: –2.25DS +1.50 add
The patient returned one year later, now at age nine. Her myopia had progressed by 1.75D in each eye, with a prescription of OD –4.00DS and OS –4.00DS.
This was concerning, as patients who reach –5.00D of myopia or higher are at greater risk for ocular complications such as glaucoma, retinal detachment, and cataract, resulting in a 34% risk of visual impairment.6
Obviously, prescribing the progressive spectacle lens had had very little effect on slowing her myopia progression. Subsequent studies have found large, lined bifocals that are positioned high (just below the pupillary margin) to be more effective.8,9 This is thought to result from a larger portion of the retina being impacted by the myopic defocus created by the plus power in a large add segment.
However, the patient was reluctant to wear a lined bifocal. Her mother had successfully worn corneal GP lenses for many years, so when the option of orthokeratology was presented, both mother and child were excited to pursue it.
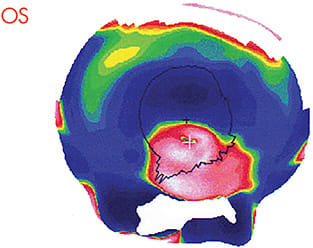
Both eyes were fit with orthokeratology lenses, which we refer to as “devices” in our office to distinguish them from standard contact lenses. She returned the following morning wearing her devices. They both appeared to ride up slightly, but topography following lens removal demonstrated good centration of the treatment zone (Figures 9 and 10), so no changes were made.


Now 22 years old and a college student, she continues to wear her orthokeratology devices for an average of nine hours per night. Over all of these years, we have made only one base curve adjustment following the initial fitting. At her most recent visit five months ago, a very confident and engaging young woman presented with no visual complaints and was able to read 20/20 with each eye uncorrected.
MULTIPLE MOTIVATIONS
Whether motivated by the impact that you can have on patient’s lives, the benefits to the bottom line, or both, investing in specialty contact lenses can be very rewarding from many perspectives. You might even describe it as something special. CLS
REFERENCES
- Ritson M. Which patients are more profitable? Contact Lens Spectrum. 2006 March;21:38-40,42.
- American Optometric Association. Survey of Optometric Practice. 2012 Nov.
- Duffy M. The FDA Approves Marketing of the Triggerfish “Smart” Contact Lens Sensor to Monitor Glaucoma Eye Pressure. VisionWare. Available at https://www.visionaware.org/blog/visionaware-blog/the-fda-approves-marketing-of-the-triggerfish-smart-contact-lens-sensor-to-monitor-glaucoma-eye-pressure-2338/12 . Accessed on Aug. 3, 2018.
- Legerton JA. Technology in your practice. Contact Lens Spectrum. 2017 Aug;32:28-34.
- Hui A, Willcox M, Jones L. In Vitro and In Vivo Evaluation of Novel Ciprofloxacin-Releasing Silicone Hydrogel Contact Lenses. Invest Ophthalmol Vis Sci. 2014 Aug;55:4896-4904.
- Brien Holden Vision Institute Academy. Managing Myopia course. Available at https://academy.brienholdenvision.org/browse/australia/courses/myopia . Accessed on Aug. 6, 2018
- Zadnik K, Sinnott LT, Cotter SA, et al; Collaborative Longitudinal Evaluation of Ethnicity and Refractive Error (CLEERE) Study Group. Prediction of Juvenile-Onset Myopia. JAMA Ophthalmol. 2015 Jun;133:683-689.
- Cheng D, Woo GC, Drobe B, Schmid KL. Effect of bifocal and prismatic bifocal spectacles on myopia progression in children. JAMA Ophthalmol. 2014 Mar;132:258-264.
- Berntsen DA, Sinnott LT, Mutti DO, Zadnik K. A randomized trial using progressive addition lenses to evaluate theories of myopia progression in children with a high lag of accommodation. Invest Ophthalmol Vis Sci. 2012 Feb 13;53:640-649.




