The term pellucid marginal corneal degeneration (PMD) is widely used in the ophthalmic profession to describe a characteristic topographic appearance. A topic of discussion is whether PMD is a variant of keratoconus (KCN) or whether it is a unique disease entity.1 One recognized definition of PMD is “(A) narrow band of corneal thinning, usually from four to eight o’clock, separated from the inferior limbus by an uninvolved area one to three millimeters in width,”2 (Figures 1 and 2). In PMD, the cornea protrudes above the area of thinning, and the cornea above the band of thinning is generally of normal thickness. The result of this particular manifestation of ectasia is a flattening in the vertical meridian accompanied by a high degree of against-the-rule corneal astigmatism.2 This unique anatomic presentation has also been referred to as a “beer belly” configuration.3,4

Unlike keratoconus, which usually stops progressing in the third or fourth decade of life, pellucid marginal degeneration is progressive throughout the patients’ lifetime and is non-inflammatory.5 Corneas are usually clear and without lipid deposition. With these considerations, it is evident that the clinical picture of PMD is indeed different from that of KCN.
FREQUENCY AND SIGNS OF PMD
Pellucid marginal degeneration appears to be a rare entity. Tummanapalli et al surveyed 1,113 patients who had corneal ectasias; they found that of these, only 3% had PMD while the remaining 97% had keratoconus.5 In another study that evaluated 40 eyes of 26 patients, only nine eyes had true PMD.1
While keratoconus seems to be more prevalent in men, there is apparently no difference between genders in PMD; in addition, the incidence is approximately equal.5 The age at diagnosis tends to be younger in keratoconus as well; patients who have keratoconus tend to be diagnosed in adolescence or in their early 20s (±12 years), while PMD seems to be much more elusive, with a mean age at discovery of 37 years of age (±14 years).5
DIAGNOSTIC EVALUATION
As technology has changed, so has our ability to detect all of the various ectasias. In earlier years, a distorted retinoscopy reflex, usually referred to as a “scissors” reflex, caused suspicion of a corneal abnormality. With keratometry came mires that were difficult to focus clearly; they usually appeared “bent” and difficult to resolve. The next leap in technology brought topography utilizing a Placido disk system of reflection rings. The reflection was necessarily of the tear film and relied mainly on anterior curvature maps.2 Being a reflection-based system, this technology was limited to the anterior corneal surface. Placido disk imaging can lead to a misdiagnosis of PMD versus KCN based on a pattern resembling a “crab claw” or “kissing doves.” Such patterns indicate a severe steepening of the inferior cornea without regard to corneal thinning (Figure 3).6 The “crab claw” is a pattern that is seen frequently in keratoconus as well.1

You may wonder why the topographic pattern appears as a “crab claw.” This characteristic pattern is an artifact produced by a marked flattening of the vertical meridian. At the same time, there is an accompanying steepening of the inferior periphery that extends into the midperipheral oblique meridians. The resulting crab claw pattern is thus a product of the method and instrumentation and does not accurately portray the cornea’s true shape.1 We must keep in mind that corneal protrusion is more peripheral in PMD than in keratoconus.4,6
Inferior steepening or asymmetric curvature can appear in normal eyes when the measurement axis differs from the visual axis. As is stated in the Oculus Pentacam Interpretation Guide, 3rd Edition: “Curvature is a reference-based measure. An asymmetric curvature pattern can occur with a completely normal cornea when the apex, line-of-sight, and measurement axis does not line up. This is a normal variant and in itself not indicative of pathology.” In these instances, the display will show an inferior steepening with an asymmetric “bow tie” but will not have skewed axes and corneal thinning. Misdiagnoses lead to confusing and often inaccurate terms such as “form fruste,” “subclinical,” or “suspect.”
There are some topographic clues that will help in minimizing misdiagnosis of PMD:
- Keratoconus is more likely to have mixed or hyperopic astigmatism.1
- The spherical equivalent is usually more minus in PMD.1
- Note the amount of asphericity. The “Q” value (negative in normal) has a higher sensitivity and specificity compared to the usual “e” value.5 Positive “Q” values indicate an oblate profile.
Recognizing the differences between PMD and KCN is more than simply an academic exercise. The treatment strategies are different. As previously mentioned, the cornea with PMD continues to change into the middle decades of life, possibly requiring more lens changes. Corneal shape will influence contact lens selection, whether a corneal lens, a custom soft lens, a hybrid lens, or a scleral lens. The proper diagnosis is also extremely relevant for when surgery is a consideration. For example, if intracorneal ring implants are contemplated, the area of greatest ectasia may fall outside of the zone of the intracorneal rings. The risk of corneal dissection or perforation is greater in the area where the corneal thickness changes abruptly.2 In penetrating keratoplasty, a PMD cornea may require a much larger donor cornea. Such a donor button may even be eccentric in shape. The possibility of higher rates of rejection must be considered along with significant amounts of postoperative astigmatism.1,4,7
Corneal tomography has become more common over the last decade in clinics that specialize in corneal disease. Webster’s dictionary defines tomography as “a method of producing a three-dimensional image of the internal structures of a solid object (such as the human body).” In our example, the image is of the anterior eye including the cornea, lens, iris, and parts of the ciliary body.
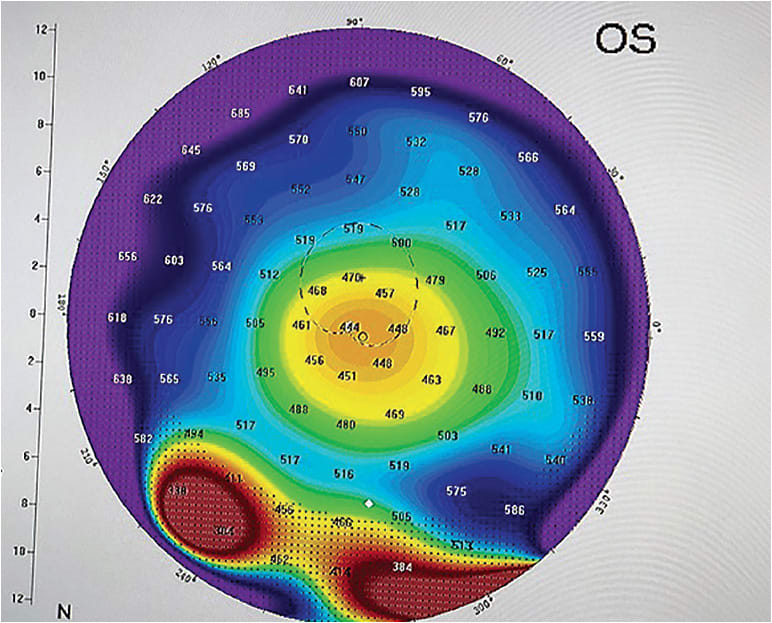
Tomography offers a number of advantages over Placido-ring-based topography. Tomography is not dependent on reflection from the tear film. In a very ectatic cornea, the profound irregularity of the corneal surface along with the presence of ocular surface disease may result in a poor topographic image of little clinical value. Tomography is a camera system not based on reflection. Its ability to penetrate the cornea makes global pachymetry possible. Without the ability to measure corneal thickness along the outer margins, the diagnosis of PMD may be missed. The image diameter is also larger in tomography, up to 12 millimeters.
Perhaps the most important feature of tomographic instruments is their ability to image the corneal back surface. It is now recognized that corneal thinning is the result of elevation of the posterior cornea.8 Tomography, which measures elevations in increments of microns, can detect minute changes long before they are evident on the anterior surface. This feature makes disease staging possible. Metrics, such as the “ABCD” (anterior curvature, posterior curvature, corneal thickness and best visual acuity) and the Belin/Ambrósio (elimination of the most ectatic region to create a normal reference sphere) are two such examples.9
A PLAN FOR FURTHER STUDY
It has been suggested by Belin et al that future studies include some minimum testing standards.2 To date, many investigations have not incorporated posterior elevation or global pachymetry. At minimum, a comprehensive analysis should include the following: anterior and posterior elevation maps, corneal topography, tomography, and pachymetry of the entire cornea. Elevation data should be true data derived via Scheimpflug photography (Figure 4), anterior segment optical coherence tomography, or newer technologies yet to be developed. By “true data,” we mean not extrapolated. Thickness should be measured in microns (µm).

These measurements would be most meaningful when taken at the corneal apex, the center of the pupil, and at the thinnest point. CLS
REFERENCES
- Lee BW, Jurkunas UV, Harissi-Dagher M, Poothulil AM, Tobaigy FM, Azar DT. Ectatic disorders associated with a claw-shaped pattern on corneal topography. Am J Ophthalmol. 2007 Jul;144:154-156.
- Belin MW, Asota IM, Ambrosio RJ, Khachikian SS. What’s in a name: keratoconus, pellucid marginal degeneration, and related thinning disorders. Am J Ophthalmol. 2011 Aug;152:157-162.
- Wolf N. Pellucid Marginal Degeneration Challenges Overcome with Scleral Contact Lenses: A Case Report on Avoiding a Penetrating Keratoplasty. Scleral Lens Education Society. 2018 Sep. Available at https://sclerallens.org/wp-content/uploads/2018/09/Standard-Case-Report-Example-3.pdf . Accessed July 15, 2019.
- Moshirfar M, Edmonds JN, Behunin NL, Christiansen SM. Current options in the management of pellucid marginal degeneration. J Refract Surg. 2014 Jul;30:474-485.
- Tummanapalli SS, Maseedupally V, Mandathara P, Rathi VM, Sangwan VS. Evaluation of corneal elevation and thickness indices in pellucid marginal degeneration and keratoconus. J Cataract Refract Surg. 2013 Jan;39:56-65.
- Koc M, Tekin K, Inanc M, Kosekahya P, Yilmazbas P. Crab claw pattern on corneal topography: pellucid degeneration or inferior keratoconus? Eye (Lond). 2018 Jan;32:11-18.
- Maharana PK, Dubey A, Jhanji V, Sharma N, Das S, Vajpayee RB. Management of advanced corneal ectasias. Br J Ophthalmol. 2016 Jan;100:34-40.
- Gomes JA, Tan D, Rapuano CJ, et al. Global consensus on keratoconus and ectatic diseases. Cornea. 2015 Apr;34:359-369.
- Belin MW, Duncan JK. Keratoconus: The ABCD Grading System. Klin Monbl Augenheilkd. 2016 Jun;233:701-707.




