
Improving a Customized Corneal GP Keratoconus Fitting
My patient was a 46-year-old male who had stage II keratoconus OD and stage I OS. My father, Saul Bastos, MD, had fit this patient with specialty GP lenses in the past, but he went to another clinic after my father passed away. He returned to our clinic in 2008 after several unsuccessful attempts to be refit elsewhere.
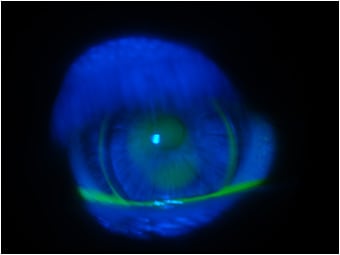
In 2008, we successfully refit him with a customized aspheric corneal GP keratoconus lens. He has been refit every three or four years since that time. The top images show the GPs that he has worn for the past three years. The fitting seemed acceptable, and he had only a few complaints about slightly degraded vision and minor discomfort at the end of the day. The fluorescein pattern is not ideal, but this cornea has a wider zone of corneal irregularity compared to most keratoconus cases.
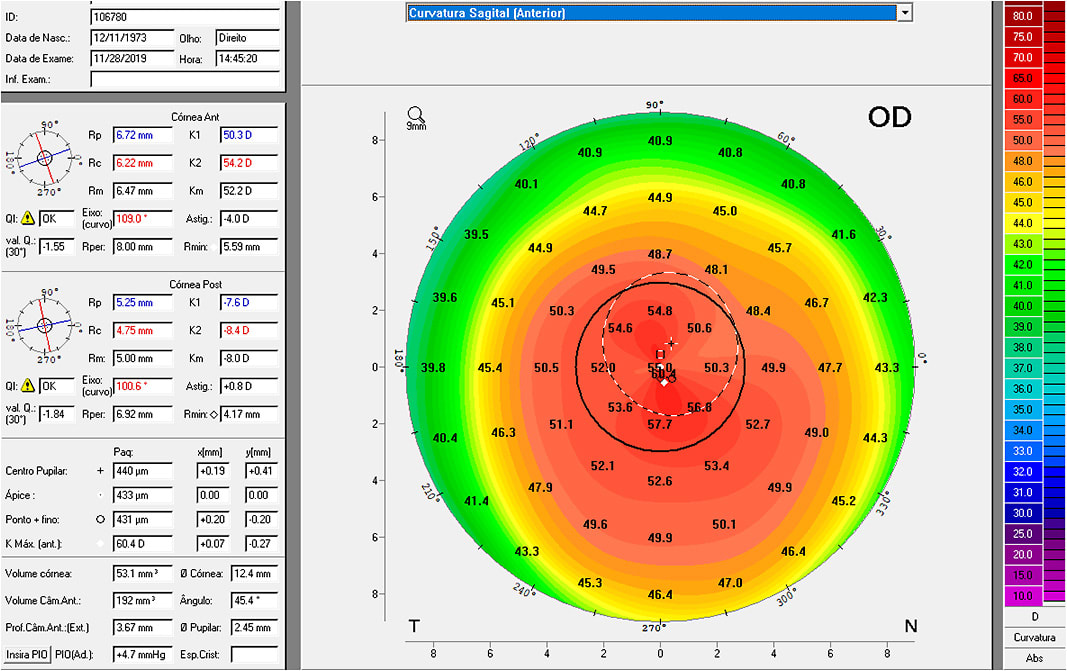
Corneal topography also showed that these were acceptable fittings, but we could see mild touch in the zone immediately below the pupil. It appears as a slight touch only after blinking when there is a small lens movement. This also may be worsened by instability of the lacrimal film, as the patient has a tear breakup time of only six to eight seconds. Figure 2 shows the exact moment after blinking when the lens moves and there is touch in a small area below the pupil OD.
Management of the Case
To improving the fitting, we first calculated the sagittal depth (sag) value of his previous lenses. After careful examination, we designed his new lenses with a greater sag value. It is interesting that we normally work with sagittal depth values only when fitting scleral lenses, but I have found sag values useful in specialty corneal GP fitting as well, especially for a highly complex irregular cornea.1
The previous lens parameters were:
OD 52D x 45D base curve (BC), –15.50D power, 9.8mm overall diameter (OAD), 6.6mm optic zone (OZ), 1.959 sag, HDS 100 material (Paragon Vision Sciences)
OS 48.50D x 44D BC, –13.25D power, 9.8mm OAD, 6.6mm OZ, 1.855 sag, HDS 100 material
I designed the new lenses based on the findings with the previous lenses and on trial fitting. The patient had suspended lens wear for five days, which was acceptable. The goal in this case was to elevate the overall lens to generate a greater vault and to better distribute the tears under the lens while being careful to not exaggerate the increased sag and vault.2
The new lens parameters are:
OD 51D x 46D, 14.75D power, 10.0mm OAD, 7.0mm OZ, 2.081 sag, HDS 100 material
OS 47.50D x 45D, –12.75D power, 10.0mm OAD, 7.0mm OZ, 1.966 sag, HDS 100 material
In this case, we wanted to promote better alignment and prevent the mild corneal touch without creating an excessive central pool. We worked with the parameters that influence and create changes in the sag values; these include base curve (primary and secondary curves or more), central and secondary optical zones diameters, and overall diameter. As I mentioned in a previous column, labs usually do not include sag values on the label for corneal GPs, but most should have these values when the lens is manufactured.
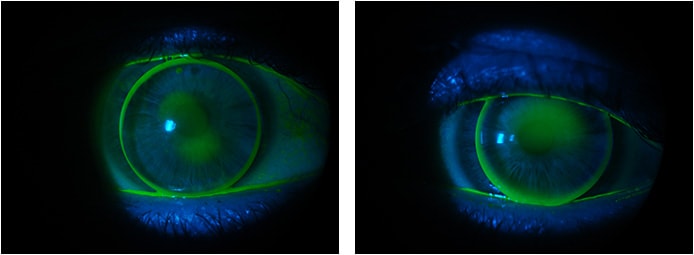
The redesigned lenses resulted in a better fluorescein pattern compared to the previous lenses. Figure 3 shows the new lenses after modifying the parameters and increasing the sag by 0.122 OD and by 0.111 OS. We found that using the sag values in planning the customization was very helpful. We also used the topography images by comparing the previous fluorescein pattern with the sagittal (Figures 4 and 5) and tangential maps.

Conclusion
While not something that you would need to use in every case, it is helpful to use sag values when customizing corneal GP lens designs, especially for challenging cases in which a design’s trial lens set will not be enough to resolve the fit. In such cases, using the sag values can help practitioners make an educated guess about what parameters to change and can more precisely predict an expected result.3
In contrast to scleral lens, corneal GPs tend to be more sensitive to subtle changes in sag values; therefore, the amount of change should be smaller compared to that for sclerals. Also, there is a learning curve and an experience curve in which practitioners over time will be able to better predict these changes, always observing the resultant sag values of the proposed changes.
References
- Douthwaite WA. Contact Lens Optics & Lens Design (2nd edition). The SAG Equation. Butterworth Heinemann, 1995, Pages 53-54.
- Soper JW. Sagittal Value Calculation and Table (1970)
- Girard LJ, Ridley F. Corneal and Scleral Contact Lenses – Proceedings of the International Congress. Contact Lens Fitting Theoretical Considerations. The C.V Mosby Company, 1966, Chapter 24, page 200.
- Bastos L. Online Photo Diagnosis – Refitting a Corneal GP Lens Over a Scar. Contact Lens Spectrum. 2018 Dec;33:9. Available at https://www.clspectrum.com/issues/2018/december-2018/online-photo-diagnosis . Accessed Dec. 5, 2019.
- Bastos L. Online Photo Diagnosis – Managing an Improper GP Lens Fitting. Contact Lens Spectrum. 2019 Mar;34:9. Available at https://www.clspectrum.com/issues/2019/march-2019/online-photo-diagnosis . Accessed Dec. 5, 2019.



