It is important for any eyecare professional to be familiar with cosmetic and therapeutic options for patients who are challenged with scarred or disfigured eyes secondary to trauma or to a congenital defect. These patients need help in managing psychological, cosmetic, and visual problems that afflict them on a daily basis. Many patients are unaware of the options that an eyecare professional can recommend to cosmetically improve their disfigurement or to aid in sighted eyes to eliminate visual challenges. This can be one of the most rewarding and memorable roles as an eyecare provider...changing patients’ lives!
There are approximately 2.4 million eye injuries annually in the United States, and an estimated 10% to 20% result in temporary or permanent vision loss.1 In addition, there are many genetic factors that can challenge patients cosmetically and/or visually, potentially resulting in blindness. Congenital cataracts, congenital glaucoma, optic atrophy, and retinal degeneration account for more than 60% of infant blindness. In addition, the two leading causes of adult blindness include glaucoma and age-related macular degeneration.2
PSYCHOLOGICAL CHALLENGES
Your role as a primary care provider is to inform patients of the various contact lens options available that can minimize the psychological challenges that they encounter daily. In addition, using these lenses can eliminate a range of issues including diplopia, photophobia, poor depth perception, poor mobility, and orientation concerns.
After many years of providing prosthetic lenses to patients, I find that it is important let patients know that you can never make their prosthetic lens look exactly like their real natural eye. However, with current technology and various prosthetic lens options—including scleral shells, soft prosthetic contact lenses, and surgical iris implants—practitioners can have very successful results.
PROSTHETIC OPTIONS
There are many reasons that a patient might be challenged with a disfigured eye and could benefit tremendously from the suggestion of a prosthetic lens (Table 1). There are three options of prosthetic lens designs based on the patients’ situation: rigid scleral shells, iris implants, and soft contact lenses.
| 1) Accident/Injury (trauma/chemical burns) |
| 2) Congenital defects |
| 3) Surgical complications (retinal, corneal, glaucoma) |
| 4) Retinal detachments |
| 5) Infectious diseases (herpetic keratoconjunctivitis, trachoma) |
| 6) Poor nutrition |
| 7) Sjögren’s syndrome |
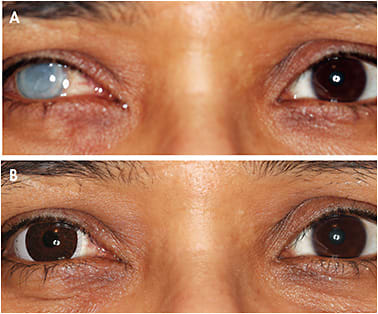
Rigid Ocular Prosthetic Shells When the eye is enucleated, a scleral shell or artificial plastic eye material is the best option; it is placed within the eye socket for dramatic cosmetic benefits (Figure 1). Ocularists—although many are also optometrists—are well trained to help patients when the cavity is no longer inflamed or infected, which is typically one month later.3

To start, practitioners should determine when enucleation is necessary. There are many reasons for surgical removal of an eye to rehabilitate the eye socket and to achieve a better cosmetic appearance including tumors/cancers (e.g., retinoblastoma or choroidal melanomas), severe trauma causing extreme disfigurement, severe pain that is unmanageable in a blind eye (e.g., end-stage glaucoma, phthisis bulbi, or iridocyclitis), and/or grossly disfigured eyes (Table 2). The management of patients afflicted with these extreme challenges is carefully discussed with ophthalmologists, optometrists, and ocularists to determine the best outcome, both cosmetically and psychologically, for each patient. (Note: evisceration may be an option based on the severity of the case).
| 1) Pain | secondary to increased pressure or infection |
| 2) Cosmetic | appearance (e.g., shrunken blind eye) |
| 3) Infection | preventing spread to surrounding tissue |
| 4) Tumors | preventing spread of cancerous growth |
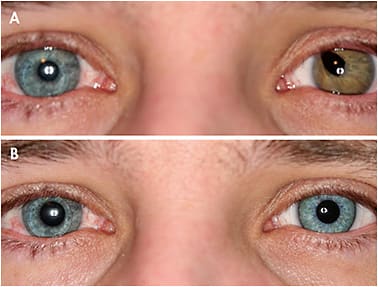
Surgically Implanted Iris HumanOptics AG’s CustomFlex Artificial Iris was approved by the U.S. Food and Drug Administration (FDA) in May 2018, representing the first surgically implanted custom prosthetic iris (Figure 2).5 This device is used to treat congenital and traumatic aniridia, albinism, iris challenges from melanoma, and other needs for a prosthetic iris. It mimics the iris and creates a pupil to reduce photophobia for patients challenged with a complete or partial absence of the iris.

Soft Contact Lenses There are several different options when it comes to prosthetic soft contact lenses.
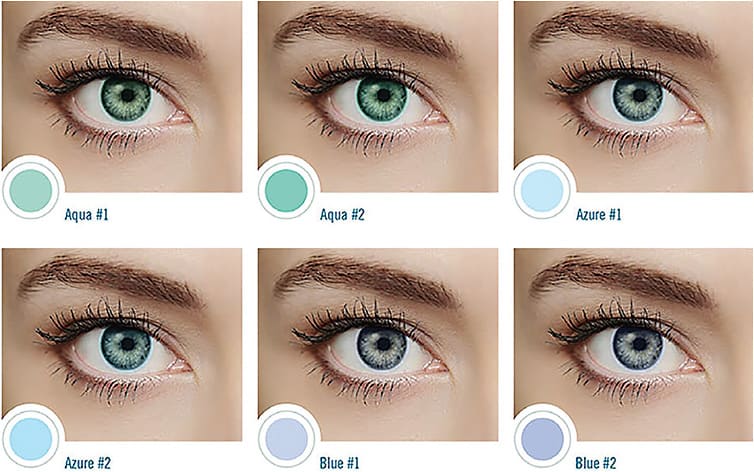
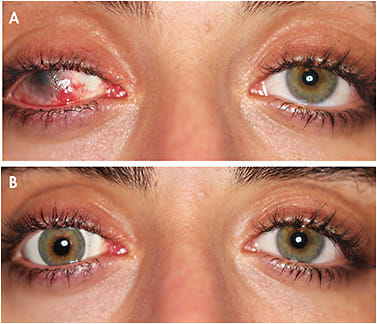
1) Transparent Soft Tinted Lens Designs These are commonly used when patients have mild disfigurements, typically in those who have a darker iris. The transparent lens overlaps the natural iris tones to slightly enhance iris coloring (Figure 3). This generally represents a less expensive and more comfortable lens option that can be very satisfying for patients. These lenses are often used for photophobia, heterochromia, and color blindness.
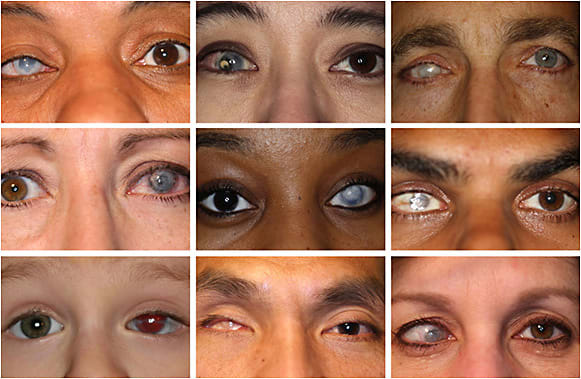
2) Soft Opaque Lens Designs This type of design includes soft dot matrix, computer-generated, and custom hand-painted lens designs. They are necessary to mask deformities, reconstruct an abnormal iris or pupil opening, occlude pupils, and cosmetically align misdirected or strabismic eye posture.
Soft dot matrix/computer-generated lens options provide various base curves, iris measurements, pupil openings/black pupils (for diplopia), and various standard colorings (Figure 4). The possibility of matching a sighted, perhaps non-prosthetic eye to the needed prosthetic with the same coloring is an option. Typically, this option is less expensive and more reproducible while also having quicker availability.

3) Soft Opaque Custom Hand-Painted This lens design offers more customization including various lens diameters, base curves, iris diameters, pupil sizes, and iris colorings, with various emphasis on flecks, coronas, and limbal rings. There are optional techniques in hand-painted lens designs that offer a natural-looking contact lens. The lens can either be one-dimensional, with the painting placed on the front surface of the lens, or three-dimensional, with the color embedded in the lens matrix; color options are company specific. These lenses are typically more expensive, more natural looking, and require more time to receive (Figures 5 to 9).

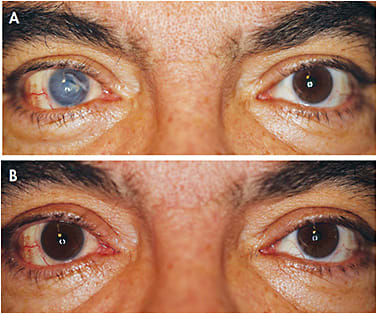

4) Soft Opaque Custom Hand-Painted Scleral These are truncated to stabilize an offset iris to achieve a more natural iris appearance for strabismus alignment challenges (Figures 10 to 13). The lenses can range in diameter from 16mm to 21mm, allowing the iris to be repositioned. For severe strabismus, muscle surgery might be recommended in addition to these custom lenses.



WHO IS A CANDIDATE FOR PROSTHETIC SOFT CONTACT LENSES?
There are many situations in which an eyecare professional should be cautious when recommending both a surgical intervention and a soft prosthetic lens, including chronic or active eye infections (e.g., acute or chronic uveitis); active or untreated glaucoma or retinal detachments; pregnancy; and active disease with blood vessel growth (rubeosis), diabetic retinopathy, and Stargardt’s.
However, when a patient has the globe of the eye intact, no infections, no corneal complications or sensitivity issues (excessive dryness), and has the ability to wear a contact lens and/or possibly be sighted, there are several lens choices to help enhance a patient’s appearance and, in some cases, therapeutically enhance vision. As noted above, there are various soft prosthetic options that should be considered to help a patient both cosmetically and in certain cases therapeutically. As with any lens, a discussion of cost as well as therapeutic and/or cosmetic expectations should be had with the patient at the beginning of the consultation.
12 STEPS TO SUCCESSFUL SOFT PROSTHETIC CONTACT LENS FITTING
Step #1) Discuss patients’ goals. Realistic expectations should be discussed prior to moving forward with a fitting of a prosthetic lens. Make patients aware that a prosthetic soft lens will never be exactly like a real eye. However, with new technology and advancements in the industry, the end result should be very pleasing and beneficial to the patient.
Step #2) Take a patient history. Take note of whether patients are in need of a prosthetic lens due to a congenital complication or a traumatic injury. There also may be a time element because a more custom lens obviously take longer to provide to a patient. In addition, it would be helpful to be informed about whether any previous prosthetic lens had been used and whether there were any concerns with previous materials (e.g., previous sensitivity issues with contact lenses, dryness, etc.).
Step #3) Be aware of a patient’s emotional state. A congenital eye defect or a sudden traumatic injury can cause extreme psychological damage to a patient. This means that eyecare professionals may be dealing with patients who are presenting with low self-esteem and insecurity about their appearance. It is not uncommon to have patients attempt to conceal their challenged eyes with sunglasses, hats, hair style, etc. Discuss the daily challenges that patients confront, and emphasize that the goal is to make a difference in their life.
Step #4) Choose the material. There are many considerations prior to selecting the initial material. The most important is to confirm whether the globe of the eye is intact. A shrunken globe or a recessed eye cavity will be problematic in terms of proper alignment for a soft contact lens. A scleral shell versus soft contact lenses would likely be the consideration.
Step #5) Evaluate transparent versus opaque designs. If the decision is to use a soft lens material, the next step is to determine whether an opaque lens is needed to mask a severely disfigured eye, occlude a pupil (diplopia), reconstruct a pupil opening, or realign a misdirected eye (strabismus). Another option would be to use a transparent tinted lens for a mild scar or photophobia.
Transparent lenses are less expensive, readily available, and reproducible; however, more severe defects will require an opaque lens design ranging from a standard to a custom lens design. For more exacting detail, iris flecks, limbal rings, and coronas can be hand-painted on a custom lens design.
Step #6) Know your resources. There are various prosthetic lens companies that can provide more options for patients and practitioners. There are standard stock lenses that can inexpensively provide various results depending on what is needed. Some companies might recommend that patients come to their specific location to provide the best outcome, with exacting measurements including an extensive range of trial lenses and photography equipment for maximum color match, etc.
A TRIBUTE TO DR. MORTON GREENSPOON
One of the most gratifying moments in any practice is when you can change a patient’s life. More than 20 years ago, I realized that there was a need to help patients who have scarred or disfigured eyes resulting from congenital abnormalities or traumatic injuries. I was determined to get involved to help patients manage these ocular challenges, which include psychological, cosmetic, and/or visual concerns.
Early on in my career, I was introduced to the colored contact lens sector of the market through a patient who needed a special effect lens for a theatrical production. My determination to help this patient led me to Morton Greenspoon, OD, whose father, Reuben Greenspoon, OD, was the first person to place a colored contact lens onto an actor’s eye in the movie industry. Dr. Greenspoon was very instrumental in providing me with insight into the colored lens industry.
Dr. Greenspoon also helped me realize that the same colored lens techniques that help to make actors’ eyes appear scarred and/or disfigured could also be used to help patients who have scarred and/or disfigured eyes to look “normal” (a 180º turn). Here is a sampling of patients who could benefit from prosthetic lenses.
Step #7) Take measurements.
Base Curve It is not unusual to have severe irregularity or the inability to obtain accurate topography measurements due to traumatic or congenital corneal defects. The base curve of various lens designs is often determined empirically. The best-fitting lens would have optimal—not excessive—movement, with the lens positioned central to a patient’s globe to have maximum symmetry while providing a natural cosmetic appearance.
Iris Diameter The goal is to measure the iris diameter in 0.5mm steps, providing total coverage of any disfigurement and ensuring that the eyes match in size to maximize the overall appearance. The average iris measurements range from 10.2mm to 13mm.
Pupil Diameter Pupils vary in size depending on lighting conditions. It is best to measure the pupil size in normal room illumination. The average pupil size in adults ranges from 2mm to 4mm in bright light to 4mm to 8mm in the dark. A patient presenting with a darker-pigmented iris is more difficult to measure; in these cases, use a Burton Lamp to enhance the visibility of a pupil because the fluorescence of the crystalline lens, in ultraviolet light, makes the measurement of the pupil much easier. Note whether a patient needs a black occluder pupil or a clear opening. When attempting to eliminate diplopia, measure the pupil in dim illumination to record the maximum size needed to prevent light from entering the eye.
Iris Coloring Recognize that the iris is translucent and can change coloring, especially in lighter iris coloring/tones; changes can be based on lighting conditions, clothing, etc. For more accurate results, have digital professional photographs taken in natural lighting or refer to an eyecare professional who specializes in prosthetic lenses. An inventory of iris coloring samples and the ability to record the proper coloring and measurement is crucial to achieve the best possible outcome.
Step #8) Determine cost. There are given situations in which a patient might be reimbursed under the special procedure code 92499. The material fees will vary depending on the lens design that is needed. There is a range in fees, depending on a standard stock lens versus a customized hand-painted lens design.
Step #9) Discuss delivery time. Not surprisingly, a more customized hand-painted prosthetic lens design will take more time compared to a transparent or standard opaque lens option. Recognize a patient’s situation and carefully discuss the delivery time and expectations of the final lens.
Step #10) Dispense the lens. Specific wearing and caring instructions should be provided when dispensing a lens. Patients should be aware that this is a medical device that requires special care and handling. Various solutions can maximize comfort and longevity of the lens material. Hydrogen peroxide solutions may be contraindicated with certain hand-painted opaque lens designs because they will cause color to fade.
Step #11) Recommend safety glasses. Many prosthetic patients are non-sighted or present with decreased visual acuity in one or both eyes depending on the situation. Emphasizing safety—by recommending protective glasses—is paramount to these patients, because they can lose their only sighted eye from an unexpected traumatic injury in a split second. Camouflaging the prosthetic lens and/or balancing the lid aperture size symmetrically can be achieved by using a refractive correction to magnify or minify overall appearance with glasses.
Step #12) Perform annual eye examinations. An annual eye examination to maintain the health of the sighted eye is extremely important. In addition to following up on the patients’ prosthetic device, recommending sunglasses to prevent early cataracts in their sighted eye should be emphasized. Note: advise patients to have a spare lens at all times in case their lens needs to be replaced (e.g., comfort issues, color changes, sensitivity issues, etc.).
THE END RESULT
Prosthetic contact lenses become a part of patients’ daily routine. And often, it completes their overall appearance to make them feel whole again; in turn, these lenses help them feel great about themselves and interacting with the public without any apprehension. CLS
REFERENCES
- Prevent Blindness America. The Scope of the Eye Injury Problem. 2019. Available at www.preventblindness.org/sites/default/files/national/documents/fact_sheets/FS93_ScopeEyeInjury_0.pdf . Accessed Oct. 14, 2019.
- Cleveland Clinic. Inherited Eye Disease. 2019. Available at https://my.clevelandclinic.org/health/diseases/17130-inherited-eye-disease . Accessed Oct. 14, 2019.
- American Society of Ocularists. When You Should See an Ocularist. 2017. Available at www.ocularist.org/resources_see_ocularist.asp . Accessed on Oct. 14, 2019.
- Günalp I, Gündüz K, Ozkan M. Causes of enucleation: a clinicopathological study. European Journal of Ophthalmology. 1997 Jul-Sep;7:223-228.
- US Food and Drug Administration. CustomFlexTM Artificial Iris – P170039. 2018 June 4. Available at www.fda.gov/medical-devices/recently-approved-devices/customflextm-artificial-iris-p170039 . Accessed Oct. 20, 2019.




