It’s difficult to estimate how close we are to the “perfect” contact lens—one that is essentially “invisible” to the biological systems of the ocular surface and that provides excellent vision across a range of clinical situations. My guess is that when August Müller reported correcting his own myopia with a glass scleral lens in a dissertation at Kiel University in Germany in 1889,1 he might have speculated that he was within a few years of converting his initial efforts into a more viable solution. Another great contact lens pioneer, Norman Bier, seemed certain that the world was close to the ideal contact lens in 1957 when he wrote that “…it would be safe to say that the days of basic discoveries have passed” in terms of contact lens developments.2
More than 60 years from this declaration, I’m not so sure. I think that there are big developments to come, and in this article, I will outline four contact lens “wishes” that will get the field closer to this “invisible” lens concept—or, at the very least, they will increase the number of new wearers entering the market while simultaneously reducing the number of dropouts.
WISH #1: CONTACT LENSES AND THE OCULAR SURFACE
Although determining the number of contact lens wearers in the world is frustratingly difficult, published reports suggest that 140 million is a reasonable estimate,3 equating to around 4% of those needing vision correction. Given the benefits of contact lenses that are well known to the readers of this journal—including that they are a reversible, modifiable, quasi-natural form of vision correction—this current modest success points to enormous potential for improvements and innovative new products.
Fundamental to this, in my view, is a greater understanding of the biological impact of a contact lens on the ocular surface. The opportunity to greatly improve our knowledge in this area was eloquently summarized by Efron in his 2012 editorial for the British Journal of Ophthalmology titled “Is contact lens wear inflammatory?”4 He argued that modern, clinically accessible techniques allow for evaluation of the subclinical inflammatory status of the ocular surface to a contact lens. This provides access to new measures by which we can assess contact lens designs and materials, and the industry can utilize this new knowledge to develop enhanced products.
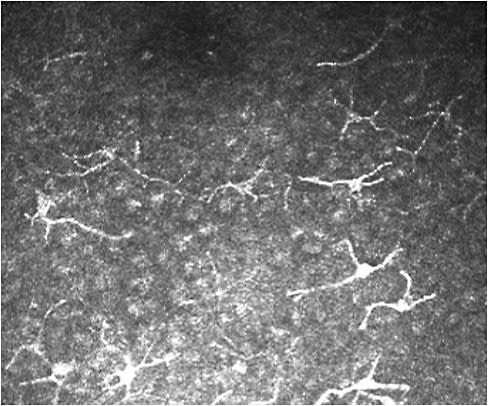
For example, tear film samples from wearers of reusable soft lenses have exhibited increased cytokine levels and inflammatory biomarkers compared with those using daily disposables;5 more dendritic cells are present in the cornea of lens-wearing eyes compared to with no lens wear;6 and, my own group has recently found a greater density of dendritic cells and leukocytes in the bulbar and lid margin conjunctiva when reusable contact lenses are worn compared to daily disposable lenses.7 (Figure 1).
Understanding the biological relationship between a contact lens and the ocular surface at this subclinical level is not some fascinating academic cul-de-sac. The two outstanding clinical issues in the field—manifest inflammatory events and wearer discomfort—may both be explained (and solved) by such research efforts. In turn, this could lead to improved lens materials and designs, greater ongoing wearer satisfaction, and a reduction of that great scourge of the industry: the high rate of contact lens dropouts.
A related matter is the risk of microbial keratitis during contact lens wear. Estimates of infection rates with modern lenses clearly indicate that daily lens wear is “safe” by any reasonable standard, but many are surprised to learn that the risk of acquiring microbial keratitis with daily wear soft lenses is 60 fold that of the risk for non-lens wearers.8 Although the introduction of daily disposable lenses appears to have not diminished infection risk by any meaningful level,9 manufacturers and researchers should continue their efforts to seek imaginative and novel solutions to minimize the increase in risk of infection evident when a patient becomes a contact lens wearer.
The first item on my wish list, then, is a continued and long-term effort to better understand the local biological sequelae of a contact lens on the ocular surface. The “oxygen battle” of 1970 to 2010 (which was won by the industry with the introduction of silicone hydrogel materials for both daily wear and extended wear) needs to be supplanted by the “inflammation battle,” which has had only early skirmishes thus far.
WISH #2: CONTACT LENS DROPOUTS
As alluded to above, dropouts are a major issue for patients, practitioners, and industry alike, and my second wish relates to this. Until recently, we knew why people tended to cease using contact lenses,10 but good data on how many were scarce. Some excellent work by Sulley et al within the last four years has provided much needed estimates. Using two different methodologies, they established that the retention rate for new contact lens wearers was around 75% in the first year (that is, a dropout rate of 25%).11,12 Sulley and Veys have recently reported that, for the U.K. market, the dropout rate across all wearers (i.e., new and established) is 17%.13
While ceasing contact lens wear is disappointing for wearers and frustrating for clinicians in the field, the effect on the commercial success of the sector is enormous. In some recent unpublished work, I have been modelling the impact of reducing this chronic dropout rate. My estimates suggest that the average practice attracts about 25% of its wearer base as new wearers each year, combined with an annual dropout rate of 17%. This would mean that if current trends prevail, the practice would double its contact lens base over 10 years. However, if the annual dropout rate is reduced from 17% to 13%, the number of wearers triples. Ten percent discontinuation per year leads to a four-fold increase in wearers over this period.
Such data are doubly positive for eyecare practitioners. First, these market increases are greater compared to any that could be reasonably expected from a new lens material or design. More importantly, the power to instigate such a change is principally in the control of practitioners. The main reasons for discontinuation are familiar to all contact lens practitioners: discomfort, poor vision, and difficult handling.10,12 Critically, however, Sulley and co-workers reported that almost half of wearers who discontinue in their first year do so within the first eight weeks of lens use. This strongly suggests that eyecare practitioners and their staff should remain in close contact with their new wearers over this initial period—via phone, e-mail, or messaging services—to identify those having difficulties and to offer follow-up examinations and advice to address these issues. This proactive approach is key, because most wearers who eventually drop out do so without any communication with their contact lens practitioner.13
Wish list item number two, therefore, is for contact lens practitioners to focus on contact lens dropouts and for industry and researchers to explore evidence-based methods to assist them in this endeavour. Modest improvements in retention will lead to significant growth in the market in the medium term.
WISH #3: CHILDREN
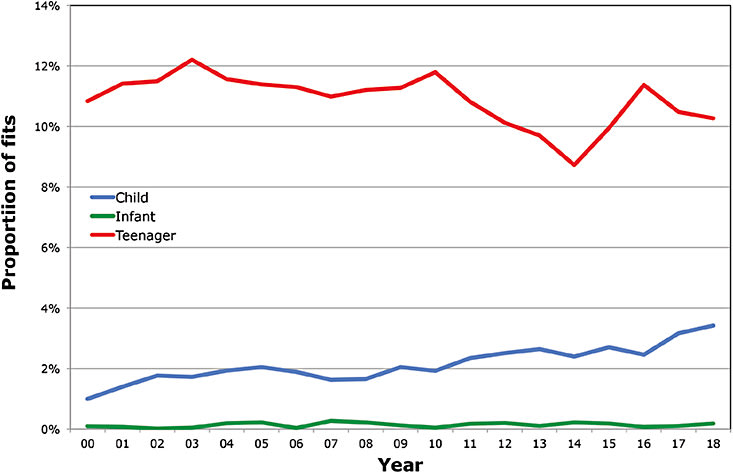
My third aspiration relates to contact lenses for children. A 2011 survey of contact lens prescribing found that about 13% of contact lenses are prescribed to patients aged 17 years and younger,14 and this value has remained approximately similar in recent years (Figure 2). It is evident that contact lenses offer a number of benefits over spectacles for this age group. Related to this, Plowright and colleagues recently reported on a clinical study in which 110 ametropic teenagers were randomly assigned to wear either spectacles or daily disposable contact lenses for a six-month period.15 One, three, and six months after being dispensed with their correction, the subjects were re-examined; the teenagers reported improved quality of life with daily disposable lenses, particularly with regard to appearance, satisfaction, and activities, when compared to spectacle wear. Experienced clinicians are likely unsurprised by these findings, but it is helpful to have this evidence base when discussing the potential benefits of contact lenses with younger patients and their families. Interestingly, in this work, the subjective advantage apparently diminished at the later visits, a trend that the authors ascribed to the wearers becoming adapted to the benefits of contact lenses, which became the “new normal” within a few weeks of wear.
In addition to the “cold data” of this sort of project, it is informative to also hear the verbal, anecdotal reports of individual participants. At the conclusion of this same project, a number of the subjects were filmed (sometimes with a parent) to convey in their own words how they felt about the experience of contact lenses. In addition to some surprise that the lenses were simple to handle and that any adaptation was minimal, many of the children reported feeling much more confident when wearing their contact lenses compared to spectacles, with the consequent accompanying lifestyle benefits. Contact lenses can really transform lives in this age group.
While contact lenses are a good vision correction option for children per se, there is of course much current interest in contact lenses as an option for myopia control. The two current “frontrunners” are dual-focus-type soft lenses16-18 and orthokeratology with GP lenses,19-21 which offer the tantalizing promise of a significant, positive impact on long-term ocular health by limiting eye growth and reducing the levels of myopia-associated retinopathy,22 retinal detachment,23 glaucoma,24 and cataract.25
As such, then, my third wish is for further evidence on the success of contact lenses as a myopia therapy. At the same time, practitioners should not lose sight of the fact that lenses are an excellent option for more routine ametropia “correction” (versus treatment) in young people.
WISH #4: PRESBYOPIA
Wish number four relates to a major untapped market for contact lenses: presbyopia. A recent estimate suggests that in 2020, there will be 2 billion presbyopes worldwide.26 In developed countries, the proportion of presbyopes is greater compared to the world average. In the United States, for example, 136 million people are aged 45 years or greater (42% of the total population).27 Further analysis of data generated by the International Contact Lens Prescribing Survey Consortium28 indicates that, at most, the uptake of contact lenses by this age category is 10%, and it is much less in many markets. The specific use of multifocal lenses (versus other contact lens design options) for vision correction in this group is typically between 1% to 6% of presbyopes across markets.28
Clearly, then, the opportunities in this market segment are considerable. There are good precedents in the soft lens market for improved lens designs quickly gaining traction, suggesting that practitioners respond positively to enhanced products. Perhaps the best example of this is the prescribing of soft toric lenses. In 2013, we reported that over the first decade of the current century, the proportion of patients receiving at least one toric lens at the point of prescription had risen from around 20% to 35% (with the notable exception of Japan, where the use of toric lenses is much lower).29 This trend has continued subsequently, and toric lenses are now prescribed to about 40% of soft lens patients—a value that is close to the 45% “threshold” of the number of people in a population who have 0.75D of refractive cylinder or more in one or both eyes.30 This example suggests that the contact lens market can change quickly and that new lens types for presbyopes may lead to similar modifications in prescribed products.
Indeed, there is some evidence that a) a greater proportion of presbyopes are being fitted with contact lenses, and b) of those fitted, an increasing number are being prescribed with multifocal or monovision lenses (rather than a single-vision-distance correction). Figure 3 shows that, on average, across 14 global markets, the proportion of all soft lenses fitted to people in the presbyopic age category (45 years of age or older) has increased from less than 20% of fits in 2003 to more than 30% in 2018. The designs of lenses fitted to this group have altered significantly. In 2003, only around 20% of presbyopes were fitted with a multifocal lens design compared with about 50% in 2018. In addition to these fits, approximately 10% of presbyopes have been fitted each year with a monovision correction.
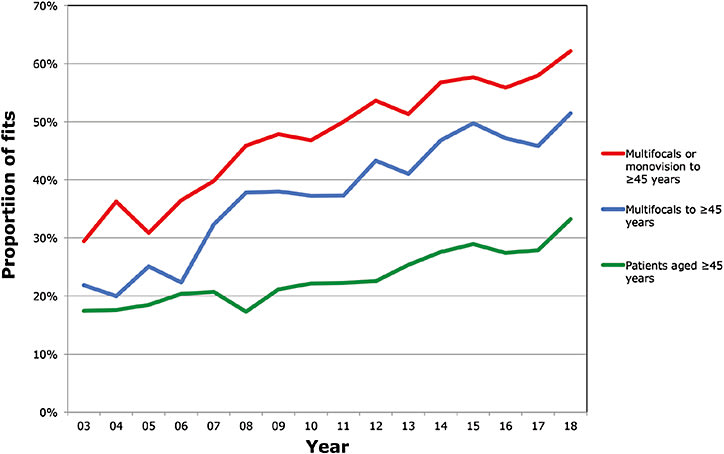
This important change suggests that both multifocal designs and practitioner confidence in this lens type are improving. The main challenges for the future are to continue to increase the uptake of multifocal lenses to presbyopes who are presenting for contact lens fitting and, more significantly, to address the great majority of presbyopes—all of whom, by definition, require vision correction—who are not considering contact lenses as an option.
It is worth stating that various novel solutions are currently being evaluated for presbyopia such as corneal inlays, which often employ a pinhole design to improve depth of focus; intraocular designs including trifocals, quadrifocals, and “accommodating” designs; pharmaceutical options including drugs that essentially soften the natural hardening of the crystalline lens with age; and laser surgical approaches including “presbyLASIK.”31 Other industries are moving forward in this area, and the contact lens community must do so, also.
One positive modification that can be employed by contact lens practitioners globally is to adopt a more proactive approach to multifocal lens prescribing. Proactive prescribing (in which contact lenses are suggested as a vision correction option to all potentially suitable patients based on their refractive error, clinical history, and ocular examination) is effective in pre-presbyopes; in 2009, we published the results of an in-practice experiment in which 91 presenting patients were randomly assigned to either a test group (in which contact lenses were proactively offered as an aid to facilitate spectacle frame selection on the same day) or a control group (in which normal contact lens procedures would commence if the patient mentioned or asked about this form of correction).32 Eighty-eight percent of the test group were happy to try contact lenses, and lenses were successfully fitted to 98% of this sub-cohort. Three months later, 33% of the full test cohort (and 38% of patients agreeing to be fitted) had purchased contact lenses from the practice. This proportion compared to 13% of patients in the control group. In other words, the simple suggestion of contact lenses as a potential option for vision correction results in a 2.5-fold increase in lens purchasing.
This work was recently repeated for presbyopes.33 Here, 196 subjects were randomized to be proactively offered multifocal lenses (test group) or for contact lenses to be considered only if mentioned by the patients (control group). After three months, 17% of the test subjects versus 8% of the control subjects had purchased contact lenses, a statistically significant difference. A key finding in this experiment was the greater propensity for women to accept the offer of contact lenses. In the test group, 53% of females accepted the offer to be fitted with lenses, and three months later, 25% of the women at the initial eye examination had purchased contact lenses.
These findings, once again, confirm the importance and authority of eyecare practitioners in contact lens prescribing. However, it is important to consider that with this authority comes a clinical obligation to outline the benefits of all forms of vision correction—including multifocal lenses for presbyopes—to our patients, and in doing so, we should reasonably expect to see an increase in the numbers of multifocal lens wearers in the future.
In addition to better patient management of this kind, we may see radical new contact lens options coming to the market. A number of companies have described their intent to develop contact lenses in which power can switch from a distance to a near correction during wear. For example, the requirements for a liquid crystal-based lens have been described in some detail by Bailey and colleagues.34 Such lenses can take various design forms and would need to be suitably powered and to contain the necessary circuitry. They would also need to be triggered in some manner, perhaps using some form of external controller. Such developments might seem far-fetched, but lenses with electric circuitry for glaucoma monitoring purposes are already available.35
My fourth and final wish, therefore, is for contact lenses for presbyopia to continue to advance and for practitioners to consider the suitability of contact lenses for each presbyope whom they examine.
SUMMARY
These four wishes cover the complete gamut of the contact lens development spectrum. I believe that we can significantly advance the field with better knowledge from the laboratories of biological scientists to provide the insights needed for future products; continued advances within industry and university research centers to bring about improved lenses for myopia control and presbyopia; and, in eyecare practices and offices globally, improved patient management so that we can better serve presbyopes and minimize dropouts. CLS
REFERENCES
- Pearson RM, Efron N. Hundredth anniversary of August Müller’s inaugural dissertation on contact lenses. Surv Ophthalmol. 1989 Sep-Oct;34:133-141.
- Bier N. Contact Lens Routine and Practice. 2nd ed. Butterworth Scientific; 1957.
- Swanson MW. A cross-sectional analysis of U.S. contact lens user demographics. Optom Vis Sci. 2012 Jun;89:839-848.
- Efron N. Is contact lens wear inflammatory? Br J Ophthalmol. 2012 Dec;96:1447-1448.
- Chao C, Stapleton F, Willcox MDP, Golebiowski B, Richdale K. Preinflammatory Signs in Established Reusable and Disposable Contact Lens Wearers. Optom Vis Sci. 2017 Nov;94:1003-1008.
- Alzahrani Y, Pritchard N, Efron N. Changes in corneal Langerhans cell density during the first few hours of contact lens wear. Cont Lens Anterior Eye. 2016 Aug;39:307-310.
- Saliman N, Morgan PB, MacDonald AS, Maldonado-Codina C. Sub-clinical inflammation of the ocular surface in soft contact lens wear. Cornea. In press.
- Brennan NA, Coles ML. Proposed performance criteria for extended wear contact lenses. Cont Lens Anterior Eye. 2000;23(4):135-139.
- Dart JK, Radford CF, Minassian D, Verma S, Stapleton F. Risk factors for microbial keratitis with contemporary contact lenses: a case-control study. Ophthalmology. 2008 Oct;115:1647–1654, 1654.e1-1654.e3.
- Dumbleton K, Woods CA, Jones LW, Fonn D. The impact of contemporary contact lenses on contact lens discontinuation. Eye Contact Lens. 2013 Jan;39:93-99.
- Sulley A, Young G, Hunt C, McCready S, Targett MT, Craven R. Retention Rates in New Contact Lens Wearers. Eye Contact Lens. 2018 Sep;44 Suppl 1:S273-S282.
- Sulley A, Young G, Hunt C. Factors in the success of new contact lens wearers. Cont Lens Anterior Eye. 2017 Feb;40:15-24.
- Sulley A, Veys J. Pay attention to retention. Optician. 2017 Jun;253:26-30.
- Efron N, Morgan PB, Woods CA; International Contact Lens Prescribing Survey Consortium. Survey of contact lens prescribing to infants, children, and teenagers. Optom Vis Sci. 2011 Apr;88:461-468.
- Plowright AJ, Maldonado-Codina C, Howarth GF, Kern J, Morgan PB. Daily disposable contact lenses versus spectacles in teenagers. Optom Vis Sci. 2015 Jan;92:44-52.
- Ruiz-Pomeda A, Pérez-Sánchez B, Valls I, Prieto-Garrido FL, Gutiérrez-Ortega R, Villa-Collar C. MiSight Assessment Study Spain (MASS). A 2-year randomized clinical trial. Graefes Arch Clin Exp Ophthalmol. 2018 May;256:1011-1021.
- Chamberlain P, Peixoto-de-Matos SC, Logan NS, Ngo C, Jones D, Young G. A 3-year Randomized Clinical Trial of MiSight Lenses for Myopia Control. Optom Vis Sci. 2019 Aug;96:556-567.
- Lam CS, Tang WC, Tse DY, Tang YY, To CH. Defocus Incorporated Soft Contact (DISC) lens slows myopia progression in Hong Kong Chinese schoolchildren: A 2-year randomised clinical trial. Br J Ophthalmol. 2014 Jan;98:40-45.
- Cho P, Cheung SW. Retardation of myopia in Orthokeratology (ROMIO) Study: A 2-year randomized clinical trial. Invest Ophthalmol Vis Sci. 2012 Oct 11;53:7077-7085.
- Santodomingo-Rubido J, Villa-Collar C, Gilmartin B, Gutiérrez-Ortega R. Myopia control with orthokeratology contact lenses in Spain: refractive and biometric changes. Invest Ophthalmol Vis Sci. 2012 Jul 31;53:5060-5065.
- Smith MJ, Walline JJ. Controlling myopia progression in children and adolescents. Adolesc Health Med Ther. 2015 Aug 13;6:133-140.
- Vongphanit J, Mitchell P, Wang JJ. Prevalence and progression of myopic retinopathy in an older population. Ophthalmology. 2002 Apr;109:704-711.
- Ogawa A, Tanaka M. The relationship between refractive errors and retinal detachment--analysis of 1,166 retinal detachment cases. Jpn J Ophthalmol. 1988;32(3):310-315.
- Mitchell P, Hourihan F, Sandbach J, Wang JJ. The relationship between glaucoma and myopia: the Blue Mountains Eye Study. Ophthalmology. 1999 Oct;106:2010-2015.
- Lim R, Mitchell P, Cumming RG. Refractive associations with cataract: the Blue Mountains Eye Study. Invest Ophthalmol Vis Sci. 1999 Nov;40:3021-3026.
- Fricke TR, Tahhan N, Resnikoff S, et al. Global Prevalence of Presbyopia and Vision Impairment from Uncorrected Presbyopia: Systematic Review, Meta-analysis, and Modelling. Ophthalmology. 2018 Oct;125:1492-1499.
- Duffin E. Population of the U.S. by sex and age 2018. Last edited 2019 Aug. Available at www.statista.com/statistics/241488/population-of-the-us-by-sex-and-age . Accessed Sept. 21, 2019.
- Morgan PB, Efron N, Woods CA, International Contact Lens Prescribing Survey Consortium. An international survey of contact lens prescribing for presbyopia. Clin Exp Optom. 2011 Jan;94:87-92.
- Morgan PB, Efron N, Woods CA, International Contact Lens Prescribing Survey Consortium. An international survey of toric contact lens prescribing. Eye Contact Lens. 2013 Mar;39:132-137.
- Young G, Sulley A, Hunt C. Prevalence of astigmatism in relation to soft contact lens fitting. Eye Contact Lens. 2011 Jan;37:20-25.
- Wolffsohn JS, Davies LN. Presbyopia: Effectiveness of correction strategies. Prog Retin Eye Res. 2019 Jan;68:124-143.
- Atkins NP, Morgan SL, Morgan PB. Enhancing the approach to selecting eyewear (EASE): A multi-centre, practice-based study into the effect of applying contact lenses prior to spectacle dispensing. Cont Lens Anterior Eye. 2009 Jun;32:103-107.
- Plowright AJ, Morgan PB. A new approach to presenting presbyopes the option of multifocal contact lenses. Poster presented at the Clinical Conference of the British Contact Lens Association. May 2019.
- Bailey J, Morgan PB, Gleeson HF, Jones JC. Switchable Liquid Crystal Contact Lenses for the Correction of Presbyopia. Crystals. 2018 Jan;8:29.
- Cutolo CA, De Moraes CG, Liebmann JM, et al. The Effect of Therapeutic IOP-lowering Interventions on the 24-hour Ocular Dimensional Profile Recorded With a Sensing Contact Lens. J Glaucoma. 2019 Mar;28:252-257.




