In a previous article, we reported the results of a retrospective chart review of children fit with orthokeratology (ortho-k) contact lenses in a clinical setting.1 In that article, we assessed whether there was a myopia control effect in children who wore ortho-k lenses compared to accepted rates of refractive error progression in non-wearers. In this publication, we’ll share statistically significant findings of ethnicity and gender on myopia progression among the same young cohort of ortho-k lens wearers.
In collaboration with the Vision Research Institute (VRI) at Ferris State University’s Michigan College of Optometry, a chart review was performed that focused on actual patient findings pre- and post-ortho-k lens wear. From a database of records developed over a 17-year period, children who wore ortho-k lenses for at least 36 months and who discontinued for a minimum of three weeks were selected. A thorough assessment of all applicable exam findings was carried out.
In our initial publication, we revealed that the mean myopia progression in children who wore ortho-k lenses on a long-term basis was –0.13D per year, with the youngest age groups exhibiting the most progression.1 This finding contrasted with published rates of progression in children who do not use any form of myopia intervention whose annual increase in refractive error ranges from –0.50D to –0.70D.2
As we filtered through hundreds of charts, we realized that there was a large representation of both Caucasian and Asian children who wore ortho-k lenses over the years. We know from epidemiological studies that the prevalence of myopia is higher among youth populations in countries in Eastern Asia (Figure 1). For example, in some East-Asian countries, recent reports reveal that more than three-quarters of school-age children are nearsighted.3,4

Although it would be easy to attribute these alarming numbers to genetic disposition alone, we know that this is not the case. In studies in which the prevalence of myopia was evaluated in children of Asian descent residing in different geographical locations, a variation in the reported total number of cases of myopia was observed between the two groups.5 Despite the obvious differences in prevalence rates, it has been shown that once baseline myopia has been established, Asians and Caucasians progress at approximately the same rate on a yearly basis, regardless of whether they were ortho-k lens wearers6 or were non-wearers.7
From our cohort of children who underwent ortho-k, both baseline and post-treatment spherical equivalent refractive error could be analyzed for progression of the refractive error over time. We were interested as to whether these results would differ significantly among the Asian and Caucasian children represented in our retrospective chart review in a manner similar to the patterns reported for myopia prevalence.
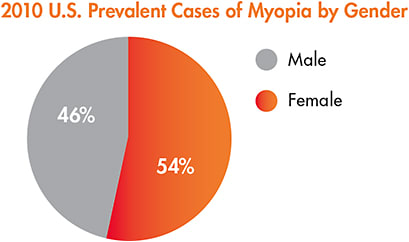
Additionally, among the patients in our chart review, there was a significant number of both male and female children. In recent literature, gender among children who do not use ortho-k is typically not a factor in the prevalence of myopia in the United States.8 In instances in which there is a gender correlation made, females tend to exhibit more cases of myopia and to progress faster compared to their male counterparts.9 As reported by the National Eye Institute,10 once adult stages are reached, the established prevalence rate among males and females is nearly 50/50 (Figure 2). These findings prompted our group to also investigate the proportion of cases of myopia and whether gender played a role in the effectiveness of ortho-k lens wear in slowing the progression of myopia in these children.
METHODS
This retrospective chart review was performed after receiving Institutional Review Board (IRB) approval from Ferris State University’s Human Subjects Committee, and it followed the tenets of the Declaration of Helsinki.
Patient selection began with an electronic medical chart database search of approximately 29,000 records. Patient selection focused on children fitted with ortho-k lenses by one of three optometrists between January 1993 and April 2010. We further identified children 18 years old and younger who presented with a baseline manifest refraction between plano and –6.00D spherical power and up to a maximum of –1.75D of cylinder power. Patients must have worn their ortho-k lenses for at least 36 months and must have stopped lens wear for a minimum of 21 days.
We categorized pre-fit, during-wear, and post-fit data for analysis. An “ideal” fit was defined as the following:
- central lens position after overnight wear
- post-fit refraction with ±0.50D of residual refractive error
- no corneal staining
- the patient was happy with the quality of vision
The Statistical Package for the Social Sciences 21 (SPSS) was used for analysis of the filtered data. For the analysis, a critical p-value (α) of 0.05 was used to denote statistical significance.
RESULTS
The search criteria yielded 105 records (206 eyes) that included age, gender, ethnicity, keratometric readings, manifest refractions, tenure wearing ortho-k lenses, and period of non-wear. The cohort at the time of initial fitting was as young as age 5 and up to 18 years old. The age range for the same group at the time of stopping ortho-k lens wear was 9 to 28 years old.
Of the 105 patients, 64.6% were female, and 35.4% were male. The ethnicity of our cohort was 130 (63.11%) Asian and 76 (36.89%) Caucasian unique eyes. The minimum wear time for patients was three years, and the maximum was 14.5 years. The median period of discontinuation of ortho-k lens wear was approximately five weeks.
The reasons for discontinuation of lens wear varied (Table 1). The most common reason for refitting was suboptimal vision during waking hours due to decentered applanation of the cornea. Additionally, if their current design was causing corneal sequelae such as superficial punctate epitheliopathy that did not resolve with parameter changes, a new fit was required. Others permanently transitioned into soft contact lens wear, and some underwent laser vision correction in adulthood.
| Subject was refit into a different ortho-k design. |
| Subject decided to undergo refractive surgery. |
| Subject desired to remain in soft contact lenses/glasses. |
To proceed with a refit, a patient was determined to be adequately washed out when the follow-up topography did not show any residual effect from wearing ortho-k lenses, such as midperipheral corneal steepening.
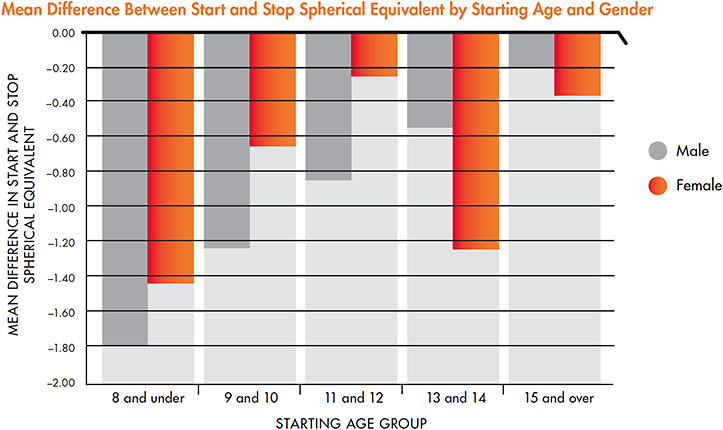
Our analysis revealed that there was a statistically significant difference in the start and stop spherical equivalent when considering starting age groups (Figure 3). The younger age groups, regardless of whether they were male or female, had a larger difference in their final myopic refractive error after the washout of ortho-k lens use compared to their initial refractive error.
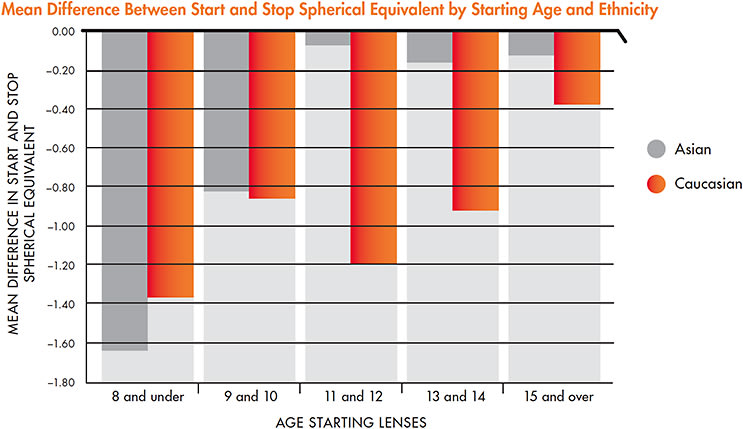
Not only did the younger age groups progress the most in amount of myopia throughout the duration of their ortho-k treatment, but when considering ethnicity, there was a statistically significant difference in the start and stop spherical equivalent between the Asian and Caucasian children of our cohort (F1,196 = 5.384, P < 0.021) (Figure 4). Additionally, certain age groups, namely the 11 to 12 year olds and the 13 to 14 year olds, exhibited a meaningful amount of progression difference between the two ethnic group categories (F4,196 = 3.250, P < 0.013). For example, if two 11-year-olds, one Asian and one Caucasian, began wearing ortho-k lenses at –2.00D of myopia, there was a significant difference in their refractive errors after the washout period, with our results showing that the Caucasian child would be left with a greater amount of myopia progression compared to his or her Asian counterpart.
DISCUSSION
Myopia Progression Differences Among Ethnicities Contrary to popular belief driven by recent reports on myopia prevalence, some of the authors sensed that there would not be a significant difference in myopia progression rates among ethnicities. Their insight stemmed from the hypothesis that when parents were seeking ortho-k as a form of vision correction in an effort to retard myopia progression in their children, those children likely spent a disproportionate amount of time indoors compared to non-ortho-k wearers, regardless of ethnicity.
In addition, the pressure to perform well academically was often apparent, as evidenced by many wearers ultimately attending Ivy League universities. In the United States, many children are encouraged to follow a path of higher learning, in which bachelor’s degrees are seen as a prerequisite to greater economic achievement. This observation is not isolated to one ethnicity.
Furthermore, many of the parents seeking ortho-k for their child’s vision correction were doing so because they themselves were myopic and empathized with their child’s dependency on vision correction. Therefore, genetic predisposition was frequently a factor. In this sense, our cohort faced pressures from both genetic and environmental factors. We know that both play a role in myopia epidemiology.
However, in our chart review, there was a statistically significant difference in myopia progression among children of different ethnicities. This finding was not clinically significant across all of the age groups analyzed. When considering variables of age and ethnicity, certain age groups exhibited a greater amount of progression of their myopic refractive error throughout the course of ortho-k lens wear.
The interplay of genetic and environmental factors on the development and progression of myopia in children is complex and has been well documented. On the one hand, we know from studies carried out with identical twins11 and from those looking at the role of myopia-associated inheritance patterns12 that there is strong evidence for nurture developmental theories. We often hear the phrase “myopia epidemic” due to the reported rise of myopia prevalence globally, specifically among adolescent populations, despite stable rates of myopia in their parents and older generations.
When it comes to the notion of a myopia epidemic, the question arises: Have we witnessed an evolutionary change due to a more demanding scholastic environment,13 or is it simply an expression of a genetic predisposition?13
We believe that genetics alone cannot explain the stark increase in myopia prevalence among school-aged children within industrialized countries. Environmental demands must be playing a more significant role than previously observed. From our retrospective review of established myopic children who wore ortho-k lenses, it would appear that there were also differences in the amount of absolute progression of their refractive error. Surprisingly, greater progression of myopic refractive error was seen in certain Caucasian, rather than in Asian, age groups.
Although not analyzed in this report, the direct impact of the lens used may have been an additional “factor” that impacted the amount of progression over time in addition to the aforementioned environmental considerations. More than five different ortho-k designs were used throughout the 17-year time period of this chart review, and changes in fitting philosophies may have resulted in variable therapeutic efficacies that contributed to the amount of myopia progression observed.
Today, we hear of differences in the shapes of Asian eyes when compared to shape profiles of Caucasian eyes,14 and we may have inadvertently observed some of these effects over time in our cohort. We echo the suggestion pointed out by Korszen and Caroline that further analysis is required to determine not only whether ethnicity plays a role in myopia progression during ortho-k lens wear, but whether it impacts ortho-k lens design to achieve the same desired treatment effects.15
Myopia Progression Differences Among Genders Despite the greater prevalence of myopia in females, which was reflected in our cohort in that nearly 65% were female, our medical chart review did not find a statistically significant gender difference in children wearing ortho-k lenses regardless of the absolute dioptric change in baseline versus washout amounts of myopia. There have been varying reports on the extent of myopia progression among girls and boys. While some population cohort studies investigating non-wearers have found that myopia progressed faster in females,16 others have found no difference between the genders.8 The subjects in our cohort grew up in a rather geographically homogenous group of schoolchildren, mainly from the upper east coast of the United States. Again, we believe that similar environmental pressures faced by both males and females may be influencing the similar rates of myopia progression observed, as was clinically the case across the youngest age groups in our analysis of the different ethnicities.
CONCLUSION
Our chart review of 105 records of children wearing ortho-k lenses for three years or longer revealed a statistically significant difference in ethnicity—a finding that was clinically significant only in certain age groups—yet no gender differences in myopia progression. We found that Caucasian children in their late-elementary-school to early high-school years exhibited greater amounts of progression in myopia when comparing their baseline level of myopia to their refractive error post-washout of ortho-k lens wear. Although the differences among ethnicities was unexpected, we hypothesize that over the 17-year time span of this chart review, the differences in lens designs used may have impacted the overall effect of ortho-k treatment, specifically in the children older than 10 years of age.
While myopia prevalence is unquestionably higher among Asian populations compared to Caucasian populations, the amount of myopic refractive error change over time with a treatment modality in place may differ. It appears that once myopia is established, the course of the progression in this cohort of children growing up in comparable environmental conditions followed a similar path with respect to gender only. However, this is nearly clinically indistinguishable when considering the youngest children in our ethnically mixed cohort. CLS
The authors would like to thank Paragon Vision Sciences, Inc. for providing an unrestricted educational grant toward the completion of this published work. We would also like to thank Laurel Whitehead for her assistance in collecting the patient data and Noah Tannen, OD, for his editorial review.
REFERENCES
- Ramdass S, Despotidis N, Rosen CM, et al. A Retrospective Look at Children Fit with Ortho-k Lenses. Contact Lens Spectrum. 2016 Oct;31:38-42.
- Donovan L, Sankaridurg P, Ho A, Naduvilath T, Smith EL 3rd, Holden BA. Myopia progression rates in urban children wearing single-vision spectacles. Optom Vis Sci. 2012 Jan;89:27-32.
- He M, Zeng J, Liu Y, Xu J, Pokharel GP, Ellwein LB. Refractive error and visual impairment in urban children in southern china. Invest Ophthalmol Vis Sci. 2004 Mar;45:793-799.
- Jung SK, Lee JH, Kakizaki H, Jee D. Prevalence of myopia and its association with body stature and educational level in 19-year-old male conscripts in seoul, South Korea. Invest Ophthalmol Vis Sci. 2012 Aug 15;53:5579-5583.
- Saw SM, Shankar A, Tan SB, et al. A cohort study of incident myopia in Singaporean children. Invest Ophthalmol Vis Sci. 2006 May;47:1839-1844.
- Wen D, Huang J, Chen H, et al. Efficacy and Acceptability of Orthokeratology for Slowing Myopic Progression in Children: A Systematic Review and Meta-Analysis. J Ophthalmol. 2015;2015:360806.
- French AN, Morgan IG, Mitchell P, Rose KA. Risk factors for incident myopia in Australian schoolchildren: the Sydney adolescent vascular and eye study. Ophthalmology. 2013 Oct;120:2100-2108.
- Sherwin JC, Reacher MH, Keogh RH, Khawaja AP, Mackey DA, Foster PJ. The association between time spent outdoors and myopia in children and adolescents: a systematic review and meta-analysis. Ophthalmology. 2012 Oct;119:2141-2151.
- Rudnicka AR, Kapetanakis VV, Wathern AK, et al. Global variations and time trends in the prevalence of childhood myopia, a systematic review and quantitative meta-analysis: implications for aetiology and early prevention. Br J Ophthalmol. 2016 Jul;100:882-890.
- National Eye Institutes/National Institute of Health. 2010 U.S. Prevalent Cases of Myopia (in thousands) by Age, Gender, and Race/Ethnicity. Retrieved from https://nei.nih.gov/eyedata/myopia .
- Hammond CJ, Snieder H, Gilbert CE, Spector TD. Genes and environment in refractive error: the twin eye study. Invest Ophthalmol Vis Sci. 2001 May;42:1232-1236.
- Dirani M, Chamberlain M, Shekar SN, et al. Heritability of refractive error and ocular biometrics: the Genes in Myopia (GEM) twin study. Invest Ophthalmol Vis Sci. 2006 Nov;47:4756-4761.
- Lin LL, Shih YF, Hsiao CK, Chen CJ. Prevalence of myopia in Taiwanese schoolchildren: 1983 to 2000. Ann Acad Med Singapore. 2004 Jan;33:27-33.
- Wu R, White L, Caroline P, Hayes J, Turner S, Clamp J. Ethnic difference in ocular profiles between Chinese and Caucasians. Poster presented at the 2017 Global Specialty Lens Symposium, Jan. 2017, Las Vegas.
- Korzen E, Caroline P. The Anatomy of a Modern Orthokeratology Lens. Contact Lens Spectrum. 2017 Mar;32:30-32,34,35,40.
- Pärssinen O, Lyyra AL. Myopia and myopic progression among schoolchildren: a three-year follow-up study. Invest Ophthalmol Vis Sci. 1993 Aug;34:2794-2802.
- Williams KM, Hysi PG, Plomin R, Hammond CJ. Prevalence of myopia in an adolescent British cohort and cognitive associations during childhood. Invest Ophthalmol Vis Sci. 2014 Apr;55:3628.
- Vitale S, Sperduto RD, Ferris FL 3rd. Increased prevalence of myopia in the United States between 1971-1972 and 1999-2004. Arch Ophthalmol. 2009 Dec;127:1632-1639.
- Quek TP, Chua CG, Chong CS, et al. Prevalence of refractive errors in teenage high school students in Singapore. Ophthalmic Physiol Opt. 2004 Jan;24:47-55.
- Jang JU, Park I. The status of refractive errors in elementary school children in South Jeolla Province, South Korea. Dove Press, 2015 Jul 8:45-51.



