Managing an Improper GP Lens Fitting
It is relatively common that when we examine new patients who are current corneal GP lens wearers, it is hard to believe that they are able to wear the lenses for a long period of time. In some cases, patients wear their lenses even with discomfort. They use artificial tears to alleviate pain. The main reason why these patients endure this level of discomfort is that they need visual rehabilitation, especially in those who have irregular corneas. Other options, such as scleral lenses, are often not presented or the practitioner simply prefers corneal GP lenses.
Frequent findings in these cases include intense photophobia, ocular pain, conjunctival hyperemia, tearing, and excessive blinking. The patients sometimes force themselves to adapt to these extreme conditions because they need the vision correction to be able to perform activities of daily living, to work/study, and to live their social life as best as possible. Often, these difficulties can lead to excessive emotional stress, especially in highly irregular cornea conditions such as keratoconus, post-graft, and post-refractive surgery complications.
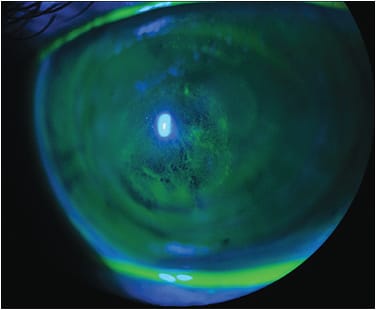
The image above shows a patient who wore the same lens for six years. He experienced extreme difficulty with the fitting and almost gave up lens wear. The image was taken immediately after removing the lens. There is diffuse staining showing keratitis especially around the corneal apex. Either the lens was fit too flat to the cornea or the patient’s keratoconus had progressed. Figure 2 shows the fluorescein pattern of the GP lens that the patient had been wearing.

Management of the Case
We instructed the patient to suspend lens wear for three days and to instill preservative-free artificial tears t.i.d. After this time, the corneal epithelium would be healed and the topography certainly would be much more reliable. Three days later, we performed topography (Figure 3) and were able to test a new customized keratoconus GP design.

The Pentacam (Oculus) instrument was used to produce a series of maps of both the anterior and posterior curvatures, corneal thickness, and Scheimpflug images to provide a good evaluation of the overall corneal condition at that specific time and as a baseline for future measures.
Discussion
Figure 4 shows the new fit in progress. This was the first trial lens tested; note the central pooling, as we did not want any apical touch. The excessive fluorescein at the peripheral curves indicates that we need to change the secondary curve and aspheric periphery. The final GP lens parameters were 61D x 45D base curves, 10.2mm overall diameter, 6.8mm optic zone, and –15.50D power.

Conclusion
Apical touch with keratoconus should be always avoided. It could lead to corneal erosion, keratitis, and subsequent corneal ulcer and scarring if not avoided. Some patients build up a tolerance to the pain resulting from poorly designed GPs. The lenses can induce an anesthetic state in which the patients feel no pain or discomfort. They only notice when the lesion worsens to corneal erosion, ulcer, or an acute corneal hydrops.
As mentioned in a previous column (https://www.clspectrum.com/issues/2018/december-2018/online-photo-diagnosis ), it is possible to use sagittal height (sag) values for corneal GPs to help customize a more complex fitting. The basics are the same, but note that sag values for corneal GP lenses are much more sensitive than for scleral lenses. Scleral lens fitting is more forgiving with respect to the sag. It may help to redesign the lens with different posterior curvatures and maintain or adjust a desirable sag after testing some trial lenses of a known sag.



