As eyecare practitioners today, we are fortunate to have a broad spectrum of options when prescribing contact lenses. With a plethora of technological advancements throughout the industry, there have been leaps and bounds in both material evolution and modality consideration. While some may revel in the diversification, others may find that selecting the appropriate material and lens can be intimidating. Are Lens X and Lens Y really that different?
While arguably a common system of classifying the myriad soft contact lenses available is by modality, another method of classification would be to divide the traditional hydroxyethyl methacrylate (HEMA) lenses from their higher-Dk, silicone hydrogel (SiHy) material counterpart lenses. Whether to prescribe hydrogel lenses versus SiHy lenses as a first choice is an ongoing topic of debate, and new technologies in both categories indicate that there is a definite role for the two different material types.
SOFT LENS MATERIALS OVERVIEW
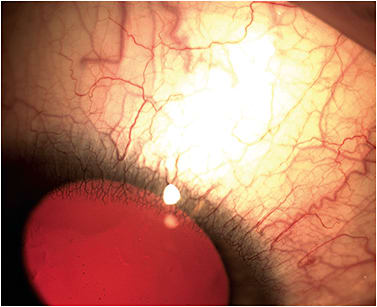
Traditional soft hydrogel contact lenses made from HEMA polymers utilize plastics that contain variable amounts of water. These lenses rely on the amount of water in the polymer to regulate how much oxygen can pass through the lens; the oxygen transmissibility levels (Dk/t) and the amount of oxygen transmitted to the cornea can be manipulated by increasing the water content.1 Clinically, due to relatively lower levels of oxygen transmission, HEMA contact lens wear has been associated with limbal hyperemia, stromal striae, vascularization (Figure 1), and endothelial changes.2,3 These signs were particularly notable in astigmatic patients and in those who have higher prescriptions due to lens thickness as well as in patients who use extended wear lenses. As higher-water-content hydrogel lenses were clinically more successful, it was noted that signs of hypoxia were minimized.3
The U.S. Food and Drug Administration (FDA)’s material grouping of hydrogels based on water content and ionic charge (Table I) has long been a standard of classification. Mid- to high-water content (> 50%) materials have been associated with significant tear film deposition.4 Group II lenses—which have a higher water content and non-ionic polymers—are prone to lipid deposition; meanwhile, Group IV lenses—which also have a higher water content but ionic polymers—have been shown to attract more protein than lipids. These groupings have helped with predicting protein deposition issues as well as potential on-eye interactions with concurrent ocular surface issues and solution incompatibilities. These are all important factors to consider when selecting an appropriate material to best match ocular physiology and lifestyle needs. For example, even though Group IV lenses attract more protein, using a more frequent replacement lens such as a daily disposable could prevent any potential deposits.
| Group I | Non-Ionic | Low water (< 50%) |
| Group II | Non-Ionic | High water (> 50%) |
| Group III | Ionic | Low water (< 50%) |
| Group IV | Ionic | High water (> 50%) |
Since their introduction in the late 1990s,2 contact lenses manufactured in silicone hydrogel materials have gradually become common “go-to” lenses for many practitioners; over time, a large number of practitioners have steadily migrated toward fitting a higher percentage of SiHy lenses. The increased oxygen permeability of SiHy lenses can lessen the stress that contact lens wear may cause to the eye.5 Hypoxia-related complications such as corneal vascularization, corneal edema, striae, folds, microcysts, and limbal hyperemia are less likely with SiHy lenses.1,6 However, are increased levels of oxygen necessary for patients who aren’t sleeping in their lenses? While the Dk/t of SiHy lenses can be four to six times greater than that of hydrogel materials, the oxygenation afforded to the cornea in hydrogel lenses appears adequate for the majority of wearers, particularly in low-to-moderate prescriptions.3,6
Aside from lens thickness and material differences, the amount of oxygen reaching the avascular cornea is also dependent on environmental factors such as atmospheric pressure variations due to altitude and the flux of oxygen across the contact lens. The first study to detail the oxygen levels needed for successful daily wear reported that a Dk/t of 24 Fatt units was required.7 The most-widely accepted re-evaluation of the topic determined that a Dk/t range of 35 Fatt units was needed to avoid corneal hypoxia with daily wear.8 Moreover, it was found that most normal corneas should be protected from vascularization complications by maintaining a peripheral Dk/t above 30 to 40 Fatt units with daily wear lenses.9
As Dk/t criteria has evolved over time, it has been argued as to whether it is truly the most useful index.10 Large changes in Dk/t above approximately 20 (for daily wear) produce only minor changes in corneal oxygenation. The Dk/t maintains a linear relationship to oxygenation only for low-Dk/t lenses; for higher values, the law of diminishing returns applies. A lens can have a significantly higher Dk/t without actually delivering more oxygen to the cornea. In essence, studies and models imply that there is little effect on corneal oxygenation beyond a certain threshold.10
As HEMA technology has advanced, especially with the mid- to high-water-content lenses and the forward momentum of increased replacement with daily disposable lenses, concerns of hypoxia and corneal compromise have lessened. While SiHy lenses have made a tremendous impact on increased oxygen delivery and physiological ocular health, hydrogel lenses can provide successful—and sometimes better—options for many patients. Whether the lenses are worn for refractive necessity or for cosmetic correction, some hydrogel lenses offer unique features that can be advantageous to certain populations and ocular characteristics. Recognizing these opportunities to maximize and integrate hydrogel advances and technologies can increase your successful contact lens fits and elevate your practice. The following are some examples of such applications.
POOR SILICONE HYDROGEL CANDIDATES
SiHy Non-Adapt or Intolerance As a result of the incorporation of siloxane components, SiHy lenses tend be more hydrophobic compared to hydrogels. The lower water content of these lenses in combination with the siloxane has a notable impact on the modulus of the lens and how flexible or stiff it is. This characteristic may result in foreign body sensation or lens awareness issues if the material has a higher modulus or fits on the looser side.3,11 Materials can affect lens movement whereby increased lens movement results in reduced subjective comfort and less lens mobility increases perceived comfort.12 People who are sensitive to the foreign body sensation due to the stiffer material or increased movement compared to hydrogel lenses may notice better all-around comfort with a hydrogel lens.
Clinically, the higher modulus of some SiHy materials and lenses has been noted to sometimes cause compromise, such as corneal staining and topographical changes, giant papillary conjunctivitis, and superior corneal epitheliopathy in some patients.1,3,12 Other physiological and mechanical complications observed with SiHy lenses have included reduced wettability, elevated levels of mucin balls, and solution-based corneal staining.3 Several reports have indicated that not only does the stiffer modulus cause these negative epithelial changes, but the use of SiHy materials also doubles the relative risk of infiltrative keratitis versus hydrogels.1,3
Additionally, younger patients have typically been found to have a higher likelihood of corneal infiltrative events.13 This has been attributed to poor hygiene habits, solution-based corneal staining, and extended wear or compliance issues. In these cases, it is imperative to prescribe a specific cleaning regimen for planned replacement lenses to avoid the potential for increased corneal staining that may occur with the use of generic or less-compatible multipurpose solutions. These situations would be ideal for refitting into daily disposable lenses, which are protective against infiltrative events relative to reusable lenses.13 Furthermore, hydrogel DDs could help to reduce corneal inflammatory events and to eliminate complications arising from SiHy intolerance as well as help to minimize potential compliance issues and solution incompatibilities.
Poor Tear Film Quality/Lid Margin Disease Several factors can lead to improved wettability during lens wear, and as some materials increase wettability, they can decrease lid interaction with the lens.14 The higher the wettability, the less eyelid friction is produced and the higher the comfort score achieved (Keir and Jones, 2013).15 Accumulation and deposition of tear film components such as proteins and lipids can alter lens wettability and fitting characteristics, ultimately affecting end-of-day comfort and stability of vision for contact lens wearers.12 Patients who are predisposed to be heavy depositors can tend to accumulate lipids on either surface of the lens, thereby causing transient blurriness and potential discomfort with lens awareness. Lens designs such as torics and multifocals, which require consistent centration and alignment for best visual clarity, could be even more noticeably affected compared to spherical prescriptions. As lipid deposition has been noted to increase with SiHy lenses due to their hydrophobic and lipophilic nature, these patients may be more comfortable in HEMA-based lenses.1,12
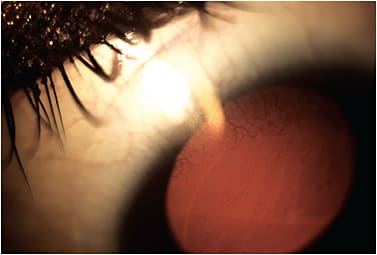
Assessing the quantity and quality of tears interacting with the surface of the contact lens is crucial to a successful contact lens fit. The interaction between the lens and the tear film and mucous layer of the epithelium plays a significant role in sustained comfort and optimal vision.16 Borderline dry eye patients often show an abundance of debris in the tear film, a reduced tear prism height, and a rapid thinning or evaporation of the pre-lens tear film.17 Marginal tear films and excess lipid contamination of the tears, often secondary to meibomian gland dysfunction and to blepharitis (Figure 2), can ultimately lead to intolerance and discomfort with certain lens materials. Because the formation of these deposits can increase the risk of biofilm formation and microbial contamination, utilizing a daily disposable hydrogel lens would further minimize these risks.

MORE COMPLEX PRESCRIPTIONS
Higher Prescriptions For patients who have degenerative myopia or aphakia, a number of hydrogel materials can be manufactured in powers from +20.00D to –20.00D, in some cases even from +30.00D to –30.00D. While such parameters are available in SiHy materials, the hydrogel spectrum typically offers a wider range of customizable base curves and diameters, which is helpful with post-traumatic or post-surgical patients who have flatter-than-average or steeper-than-average corneas and who also require a higher and more customized refractive correction. Similarly, these irregular cornea cases often require the less-common base curves for enhanced fit stability along with either greater spherical powers and/or an extended range of higher cylinder powers. These options are readily customizable in various hydrogel materials, as compared to the more limited SiHy options or the mass-produced SiHy lenses that are available in only a singular base curve and diameter combination.
Additionally, patients requiring a higher spherical power in a daily disposable lens have options in an extended range of powers—from +8.00D to –15.00D—in a hydrogel material. However, Dk/t should also remain an important consideration with regard to lens thicknesses in both the central and peripheral lenticular areas in extremely high prescriptions (Figure 3).
Aperture Variations For younger children who have smaller apertures or for Asian patients who have tighter lids, a smaller-diameter lens can be a valuable tool. Conversely, a patient who has larger apertures or larger horizontal visible iris diameters (HVIDs) can benefit from a larger-diameter lens to aid in stability and to minimize lid-lens awareness. Smaller-diameter lenses of 13.6mm and larger-diameter lenses of 14.8mm are readily available “off-the-shelf” in a hydrogel material (hioxifilcon A 59%), which is convenient to have in-office for diagnostic and dispensing purposes. As an added bonus, this daily disposable lens gives patients, frequently children and teenagers, the benefits of a fresher and healthier modality.
Toric Multifocals Many of the laboratories that manufacture more extended range contact lenses also offer customizable multifocal and toric multifocal lenses. Custom soft multifocals present niche opportunities to significantly improve multiple points of focus for presbyopic patients, particularly when over-refraction reveals a notable amount of residual astigmatism. Many designs are typically simultaneous vision with adjustable center-near addition powers and zone sizes. Again, similar to extended range sphere and toric lenses, most custom soft multifocal and toric multifocal lenses have a spectrum of available base curves and diameters.
Despite the fact that these lenses can often be manufactured in either a HEMA or SiHy material, it is important to consider the characteristics of the presbyopic population. While the stiffer material of a SiHy lens may help improve handling and overcome dexterity challenges, comfort issues may arise with respect to higher-modulus SiHy materials in older patients who have ocular surface conditions such as blepharitis and dry eye. Adequate tear film support is imperative to maximize the cornea-lens relationship, allowing for adequate corneal coverage, centration, and stability of fit—all key factors in optimal vision with multifocal lenses.
DIFFICULTIES WITH LENS PACKAGING
Patients who have larger hands or those who experience handling difficulties, either generally or secondary to systemic conditions, can sometimes have trouble with the typical packaging for most contact lenses. Between lens manipulation and achieving proper orientation on the fingertip, the excessive handling creates a more hostile application process and can be frustrating.
These patients may have better success with a lens that is flat-packed in such a way that it could never be presented inside-out. One company offers a hydrogel lens in such packaging in which the lens is sandwiched in a soft foil pack with a buffered solution. The amount of handling required is reduced, and the posterior surface of the lens remains as pristine as possible. Chances of tearing the lens with excessive manipulation are diminished as well. It could also serve as a good learning tool for lens handling in new patients of any age.
SOFT COSMETIC OR PROSTHETIC LENSES
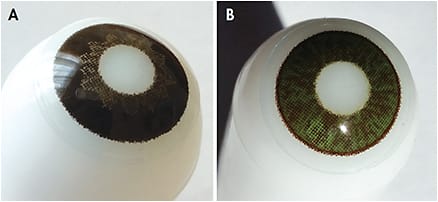
Even though there are colored contact lenses available in a SiHy material, a wider range of options for cosmetic colored lenses is available in hydrogel materials. This is because most of the pigments used to make colored contact lenses can bond with hydrogel materials but not with silicone hydrogel materials. Cosmetic hydrogel frequent replacement and planned replacement lenses are available in a palette of varying hues to best suit patients’ needs. For those who may seek a different twist in a mass-produced cosmetic lens, limbal-enhancing hydrogel contact lenses are available in a range of limbal darkness and intensity to provide definition to the iris areas.
Custom soft prosthetic lenses (Figure 4) provide a distinctive way to enhance and balance cosmetic appearance in cases in which patients have a history of traumatic injuries, congenital conditions, strabismic imbalances, or color deficiencies. These lenses are also used for those who require a sports-centric tint or who want a more unique lens for theatrical purposes. The small number of manufacturers and laboratories offering these types of lenses again offer a material selection limited to hydrogels due to tinting requirements. Nonetheless, these lenses can be made in a wide range of base curves, diameters, and powers not to mention in various pupillary and iris sizes and locations. As such, these types of HEMA lenses have a prominent place in specialty contact lens care.
NOT ALL DAILY DISPOSABLES ARE CREATED EQUAL
Daily disposable lenses account for 35% to 46% of contact lens fits in the United States18 and for 27% of fits on average internationally.19 From a safety standpoint, as discussed previously, daily disposables are protective relative to reusable lenses because they minimize compliance issues and lessen the likelihood of corneal infiltrative events. Additionally, certain conditions—such as giant papillary conjunctivitis (GPC), seasonal allergic conjunctivitis (SAC), and general ocular allergies—warrant strong consideration for daily disposable lens wear.20 Hydrogel daily disposables currently represent the only option that has FDA clearance for seasonal allergies, and many allergy sufferers don’t want to give up on wearing their contact lenses. Replacing the lenses daily prevents unnecessary buildup of allergens, airborne debris, and tear film deposition. Along with appropriate pharmaceutical treatment, using a Group I or II non-ionic hydrogel daily disposable lens could help minimize deposits, thereby reducing the symptoms of SAC and increasing comfortable maximum wearing time.
Over recent years, the rate of daily disposable usage has been on an upswing compared to other modalities. Innovative technology and rapid advancements in both HEMA and SiHy materials have helped expand usage of daily disposable lenses among practitioners. In the hydrogel daily disposable sector, many novel and unique strategies have been targeted at augmenting comfort and optimizing vision throughout the day. These technologies have included the addition of wetting agents to packaging solution, which aids initial on-eye comfort; the addition of wetting agents in the lens that release with wear throughout the day; the incorporation of coatings on the lens surface and buffering solution for enhanced comfort; the availability of an ultra-high-water-content (78%) hydrogel; and the availability of an innovative material with a SiHy core and hydrogel-like surface. Among all of these advancements in hydrogel technology, the universal goal has aimed to minimize friction, retain moisture, and prevent dehydration on the lens; thereby, patients can essentially benefit from increased end-of-day comfort.3
Having such a wide armamentarium of hydrogel daily disposable lenses has allowed more contact lens wearers to experience the ocular health benefits. For patients prioritizing spectacle use, the convenience of a single-use lens for part-time contact lens wear is invaluable. Considering their reduced wearing schedule, the question of oxygen transmissibility may be less crucial from a practical standpoint. These patients can enjoy the benefits of these new technologies coupled with hassle-free maintenance.
Aside from the advances in technology, every practitioner must deal with the perpetual question of cost. For cost-conscious patients, and particularly for children and teenagers, hydrogel daily disposable lenses typically can be offered at a lower price point versus SiHy daily disposables, making hydrogel daily disposables more economical. Patients still benefit from avoiding potential solution and preservative hypersensitivities, lowered risk of CIEs or toxic events, and lowered chance of biofilm formation on the lens surface.11 As most lens care products are composed of biocides, wetting agents, chelating agents, surfactants, and buffering agents, removing the need for a care solution prevents potential sources of allergies or discomfort, simplifying matters significantly.12 Hence, in many cases, hydrogel daily disposables may be the best choice considering all physiological and socio-economic factors.
THE BOTTOM LINE
From a clinical standpoint, some patients simply feel more comfortable in a hydrogel contact lens. Even though the broad spectrum of SiHy lenses varies in levels of wettability and performance, different anecdotal scenarios have indicated that these patients tend to be unsuccessfully refit from their existing HEMA lenses. Recent reports have indicated that neither HEMA nor SiHy daily disposable lens materials showed superiority in comfort.21 At the end of the day, the ideal goal for patients, after all, is to feel as if “nothing” is on the eye. While it may be difficult to pinpoint causative contributions from variances in tear film chemistry or meibomian gland disease, these patients prefer the feel of a hydrogel material. Therefore, they can truly benefit from the aforementioned advancements in HEMA technology, whether it be increased moisture enhancements, improved Dk/t, or the disposability that offers a fresh clean lens every day.
Ultimately, countless elements affect successful contact lens wear for patients, and being versatile in implementing different material technologies appropriately will enable practitioners to address virtually every patient’s needs. Even though SiHy materials offer distinct advantages of oxygen transmissibility, it is important to be mindful that HEMA-based lenses can also play a critical role in our toolbox. In our rapidly-evolving world of contact lenses, be proactive! This will not only prevent contact lens discomfort and maximize comfortable wearing time, it will also increase the range and types of patients who can be successfully fit. To ensure the best success, it is paramount to take the time to ascertain the best material to offer patients optimal comfort and vision, essentially giving them the visual freedom that they desire. CLS
REFERENCES
- Schorner, S. Some facts about SiHy lenses. Rev Optom. 2010 July. Available at https://www.reviewofoptometry.com/article/some-facts-about-sihy-lenses . Accessed April 16, 2018.
- Fonn D, Dumbleton K, Jalbert I, Sivak A. Protecting Your Patient’s Eye Health: Benefits of Silicone Hydrogel Lenses. Contact Lens Spectrum. 2006 Feb;21(Special Edition):38-44.
- Jones L. Hydrogel contact lens materials: dead and buried or about to rise again? 2013 Oct. Available at http://contactlensupdate.com/2013/10/07/hydrogel-contact-lens-materials-dead-and-buried-or-about-to-rise-again . Accessed April 16, 2018.
- Subbaraman LN, Srinivasan S. A Lens Fit for Dry Eye. Rev Optom. 2013 March. https://www.reviewsce.com/ce/a-lens-fit-for-dry-eye . Accessed April 7, 2017.
- Dumbleton KA, Chalmers RL, Richter DB, Fonn D. Vascular response to extended wear of hydrogel lenses with high and low oxygen permeability. Optom Vis Sci. 2001 Mar;78:147-151.
- Townsend W. Lessons Learned: Contact Lenses, Adverse Events and Bacterial Keratitis. Rev Optom. 2014 Jan. Available at https://www.reviewsce.com/ce/lessons-learned-contact-lenses-adverse . Accessed April 16, 2018.
- Holden BA, Mertz GW. Critical oxygen levels to avoid corneal edema for daily and extended wear contact lenses. Invest Ophthalmol Vis Sci. 1984 Oct;25:1161-1167.
- Harvitt DM, Bonanno JA. Re-evaluation of the oxygen diffusion model for predicting minimum contact lens Dk/t values needed to avoid hypoxia. Optom Vis Sci. 1999 Oct;76:712-719.
- Yeung KK, Yang HJ, Nguyen AL, Weissman BA. Critical Contact Lens Oxygen Transmissibility and Tear Lens Oxygen Tension to Preclude Corneal Neovascularization. Eye Contact Lens. 2018 Sept;44 Suppl 1:S291-S295.
- Brennan NA, Morgan PB. Another View of Oxygen Transmission. Contact Lens Spectrum. 2005 Dec;20:47-48.
- Miller JR, Wesley G. Alternatives to Silicone Hydrogel Contact Lenses. Rev Optom. 2011 Dec. Available at https://www.reviewsce.com/ce/alternatives-to-silicone-hydrogel-contact-lenses . Accessed April 7, 2017.
- Srinivasan S, Subbaraman LN. The Science of Contact Lens Discomfort. Rev Optom. 2015 Aug. 15. Available at https://www.reviewofoptometry.com/article/the-science-of-contact-lens-discomfort . Accessed April 17, 2017.
- Chalmers RL, Keay L, McNally J, Kern J. Multicenter case-control study of the role of lens materials and care products on the development of corneal infiltrates. Optom Vis Sci. 2012 Mar;89:316-325.
- Miller JF. I Don’t Want to Prescribe an Uncomfortable Lens. Contact Lens Spectrum. 2017 Feb;32:47.
- Keir N, Jones L. Wettability and silicone hydrogel lenses: a review. Eye Contact Lens. 2013 Jan;39:100-108.
- Tan J, Keay L, Jalbert I, Naduvilath TJ, Sweeney DF, Holden BA. Mucin balls with wear of conventional and silicone hydrogel contact lenses. Optom Vis Sci. 2003 Apr;80:291-297.
- Fuller, D. Yes, dry eye patients can wear contacts. Rev Optom. 2015 Aug 15. Available at https://www.reviewofoptometry.com/article/yes-dry-eye-patients-can-wear-contacts . Accessed April 16, 2018.
- Nichols JJ, Fisher D. Contact Lenses 2018. Contact Lens Spectrum. 2019 Jan;34:18-23, 51.
- Morgan PB, Woods CA, Tranoudis IG, et al. International Contact Lens Prescribing in 2018. Contact Lens Spectrum. 2019 Jan;34:26-32.
- Brujic M, Kading D. Daily disposables: effective from allergy to astigmatism. Rev Cornea Contact Lenses. 2017 Jan/Feb. Available at http://www.reviewofcontactlenses.com/content/c/65382 . Accessed April 16, 2018.
- Diec J, Tilia D, Thomas V. Comparison of Silicone Hydrogel and Hydrogel Daily Disposable Contact Lenses. Eye Contact Lens. 2018 Sep;44 Suppl 1:S167-S172.
- Zhao Z, Naduvilath T, Flanagan JL, et al. Contact lens deposits, adverse responses, and clinical ocular surface parameters. Optom Vis Sci. 2010 Sept;87:669-674.
- Fonn D, Sweeney D. The Benefits of Silicone Hydrogel Daily Disposable Lenses. Contact Lens Spectrum. 2015 Dec;30:42-45.
- Szczotka-Flynn L, Diaz M. Risk of corneal inflammatory events with silicone hydrogel and low Dk hydrogel extended contact lens wear: a meta-analysis. Optom Vis Sci. 2007 Apr;84:247-256.
- La Hood D. Daytime edema levels with plus powered low and high water content hydrogel contact lenses. Optom Vis Sci. 1991 Nov;68:877-880.
- Bergenske P, Eiden SB, Russell G, Epstein A. Experts Advise Caution in Abandoning Hydrogel Lenses. Contact Lens Spectrum. 2005 Oct;20:15-16.
- Lowther GE. Environmental Gases and Contact Lens Wear. Considerations in Contact Lens Use Under Adverse Conditions: Proceedings of a Symposium. National Research Council (US) Working Group on Contact Lens Use Under Adverse Conditions; Ebert Flattau P, ed. Washington (DC): National Academies Press (US); 1991. Available from: https://www.ncbi.nlm.nih.gov/books/NBK234120/ .
- Chang A, Compañ V, Weissman BA. Evolution of the Critical Oxygen Tension. Contact Lens Spectrum. 2018 Mar;33:36-39.
- Chhabra M, Prausnitz J, Radke C. Modeling corneal metabolism and oxygen transport during contact lens wear. Optom Vis Sci. 2009 May;86:454-466.
- Brennan NA. Beyond flux: total corneal oxygen consumption as an index of corneal oxygenation during contact lens wear. Optom Vis Sci. 2005 Jun;82:467-472.
- Zimmerman AB. Contemporary CL Complications. Contact Lens Spectrum. 2018 Dec;33:20-25, 27.
- Weissman BA. Corneal Oxygen: 2015. Contact Lens Spectrum. 2015 Nov;30:25-29, 55.
- Morgan PB, Brennan NA, Maldonado-Codina C, Quhil W, Rashid K, Efron N. Central and peripheral oxygen transmissibility thresholds to avoid corneal swelling during open eye soft contact lens wear. J Biomed Mater Res B: Appl Biomater. 2010 Feb;92:361-365.




