In the United States, approximately 30% of contact lenses fit are for the correction of astigmatism.1 However, 47% of patients seeking contact lens wear have astigmatism of –0.75D or greater in at least one eye.2 In addition, astigmatic patients experience better visual acuity with lenses that correct astigmatism compared to when they wear spherical lenses.3
There seems to be a discrepancy between the contact lens correction that patients need and the contact lenses that practitioners actually fit. One of the reasons for this discrepancy may be the perception that toric contact lenses are complicated and time consuming to fit. Fitting toric contact lenses for astigmatism does not need to be difficult. There are a few simple factors to consider when managing astigmats that will ensure successful contact lens wear for these patients.
TYPES OF ASTIGMATISM
With regular astigmatism, the eye has a difference in refractive power between two meridians that are 90º apart. The orientation of the different refractive powers creates the axis of the astigmatism. This differs from the irregular astigmatism in conditions such as corneal ectasias or keratoconus in which the different meridians created by the structures of the eye are not 90º apart.
There are two types of regular astigmatism that need to be considered when fitting contact lenses. The first is corneal astigmatism, or astigmatism created by the difference in corneal curvature. This can be measured with corneal keratometry or topography. As the cornea is the primary refractive element of the eye, any difference in the curvature of the cornea between two meridians 90º apart can contribute cylindrical power to a patient’s overall refractive error.
This leads us to the other type of astigmatism to consider: refractive astigmatism, which is the total astigmatism in the patient’s refractive error. This astigmatism is a combination of both the corneal and the lenticular astigmatism of the eye. When the corneal astigmatism is not equal to the refractive astigmatism, other elements in the eye, such as the crystalline lens, are affecting the overall astigmatic power.
CONTACT LENS OPTIONS
The two primary types of contact lens options to correct astigmatism are soft contact lenses and GP contact lenses. Soft lenses are the more popular option, as they offer easy adaptation and are available in different lens replacement modalities. However, they have more limited parameters and powers, and optical quality may be compromised due to the nature of the soft lens material. GP lens options have a reputation for requiring a longer adaptation time, but they may represent a viable alternative to address issues with parameter limitations or failure with soft lens correction for astigmatism.
In GP lenses, an optically significant tear lens between the cornea and the contact lens can contribute power to the overall optical system. Spherical GP lenses can correct corneal astigmatism and can be helpful in situations in which a soft toric lens is inadequate to correct patients’ refractive needs. Toric GP lenses are also an option to correct residual astigmatism as well as cases in which there is high corneal toricity and astigmatism.
Soft contact lenses drape over the cornea when placed on the eye. There is negligible tear film between the lens and the cornea, as the lens conforms to the shape of the ocular surface. Thus, the refractive power of the front surface of a soft contact lens is responsible for all of the refractive correction.
Hybrid contact lenses have a GP center and a soft skirt, which provides the optical characteristics of a GP lens with the fitting characteristics of a soft lens. They are also a good option for correcting astigmatism.
This article will focus on the fitting and management of soft contact lenses for astigmatism.
SOFT TORIC CONTACT LENSES
Soft toric lenses correct the refractive astigmatism in a patient’s refractive error regardless of the amount of corneal astigmatism. These lenses are especially useful when a patient’s corneal cylinder is not equal to the refractive astigmatism. While the concept and use of these lenses is relatively simple and straightforward, there are a few details to consider when fitting soft torics.
Lens Parameters and Design When compared to the spherical soft contact lens of the same manufacturer and material, toric soft lenses typically have slightly larger overall diameters and flatter base curves. A larger diameter improves lens centration and stability on the eye. This is important to ensure that the power and axis of the astigmatism correction are orientated correctly for the refractive error correction. When the diameter of a contact lens is increased, so is its overall sagittal depth. To compensate for this and to maintain the same fitting relationship, the sagittal depth of the soft toric lens should be kept close to that of the same brand’s soft spherical lens. For this reason, the base curves of the toric lenses are often slightly flatter compared to their spherical lens counterparts.
Toric Lens Power Availability and Selection When fitting a frequent replacement soft toric lens, there are a few factors to consider when selecting the contact lens power. Most contact lens manufacturers attempt to offer lens powers that satisfy the greatest number of patients possible with the fewest number of lenses. From a production efficiency standpoint, this means that it is difficult to make a large enough quantity of lenses for annual supplies in every possible parameter. Considering the combination of spherical power, cylinder power, and cylinder axis, the number of different lens powers that need to be manufactured increases exponentially as the power ranges increase. For this reason, there are limits to the lens powers available. However, with modern manufacturing methods, soft toric lenses are available in higher power ranges now than in the past. If a lens power that is outside of the common ranges or availability is needed, custom soft toric lenses can be ordered in any parameter necessary with a much wider range of power, cylinder, and axis availability.
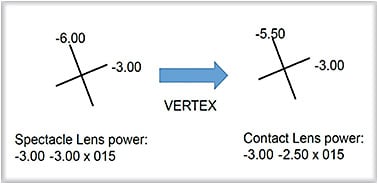
Before selecting the contact lens power, vertex the spectacle lens power to the corneal plane. This is required for each meridian of astigmatic powers greater than 4.00D. For example, a spectacle prescription of –3.00 –3.00 x 015 has 3.00D of minus power in the horizontal meridian and 6.00D of minus power in the vertical meridian. The horizontal meridian does not need to be vertexed because it is less than 4.00D, but the vertical meridian vertexes to –5.50 at a 12mm vertex distance. The lens power at the corneal plane will be –3.00 –2.50 x 015 (Figure 1).
For the spherical lens power, most frequent replacement soft toric lenses are available in a particular power range in 0.25D steps for the lower powers—such as +4.00D to –6.00D—and then in 0.50D steps in the higher sphere powers.
For the cylinder powers, remember that 0.50D of cylinder (DC) is equal to 0.25D of spherical power (DS) (spherical equivalent). For patients who have a refractive cylinder of 0.50DC, we can add the 0.25DS spherical equivalent to their sphere power to compensate. This usually provides acceptable vision for patients, especially in cases of high spherical refractive error in which the 0.50DC is only a small percentage of the overall refractive error.
The next higher cylinder power is –0.75DC, for which the spherical equivalent is more than 0.25DS, and this typically represents the lowest amount of cylinder power correction with most available standard soft toric lenses. Taking into account the just-noticeable difference of 0.25DS spherical equivalent, the next logical step of cylinder correction would be in 0.50DC steps to –1.25DC, –1.75DC, –2.25DC, etc. These steps minimize the number of lenses that need to be manufactured while providing sufficient lens options to meet the needs of the majority of the patient population. If the cylinder lens power that a patient needs falls between two available powers, select the lower cylinder lens power to prevent over-correction of astigmatism. Patients who have a higher spherical component compared to the amount of astigmatic correction are often able to tolerate slight under-correction of the cylinder power more compared to patients for whom the cylinder power is equal to or higher than the spherical power.
In terms of cylinder axis, most lenses are available in 10º steps in lower cylinder powers up to about –2.25DC and then in 5º steps in higher cylinders powers. Some lenses are available in axis steps around the clock from 10º to 180º. Other lenses, to be produced efficiently, are available in axes that are closer to the major meridians and not in oblique axes. Custom lenses can be made in any axis (i.e., 1º steps). When selecting a cylinder axis that is between two available axes, it is best to bias toward the major meridians, either 90º or 180º. For example, if an axis of 175 is required for a lens that is available in 10º steps, select the lens with axis 180 rather than 170.
When performing a diagnostic fit of a toric soft lens, the initial lens selection can make the fitting process easier. To save space, the toric lens diagnostic trial sets usually do not have every 0.25D sphere power and may not be available in every axis. Keep in mind that it is relatively easier to demonstrate a spherical power change over the eye and diagnostic lens than it is to demonstrate a change in the cylinder power or cylinder axis. When selecting the diagnostic lens in the fitting set, start with the cylinder axis first and then the cylinder power. It is always best to under-correct the cylinder power so that patients are not over-minused. If the cylinder power is under-corrected, a compensating spherical equivalent power can be added to the spherical component of the lens to minimize the blur from the cylinder power under-correction. Select the spherical power last, as it is easiest to demonstrate any under-correction of that power.
TORIC LENS ROTATION
Rotational stability is very important in a soft toric contact lens. Any rotation in the contact lens will cause the axis of the astigmatic correction to be misaligned on the eye. The combination of the incorrectly rotated cylinder of the contact lens with the astigmatic error of the eye results in uncorrected astigmatism. For every 10º of rotation and misalignment, about one-third of the cylinder power will be uncorrected.4 For example, if a lens with a cylinder power of –1.75DC is rotated 10º, more than 0.50DC will be left uncorrected. The amount of uncorrected cylinder increases as the cylinder power or the misalignment increases. Some frequent replacement soft toric lenses with higher cylinder powers are available in 5º steps compared to 10º steps in the lower cylinder powers to minimize axis misalignment with higher cylinder powers.
In addition to larger overall diameters, soft toric contact lenses employ various design techniques to orient the power of the astigmatism in the correct axis. These lens designs also need to maintain rotational stability to minimize vision fluctuations with eye and lens movement.
Blink forces of the eyelids and position of the lids play a large role in the fit of soft contact lenses. A normal blink creates forces in a vertical direction along with forces that move nasally toward the puncta. This action helps generate tear flow from the ocular surface to the lacrimal drainage system. A properly fitted soft toric contact lens needs to work with the vertical lid forces for adequate vertical movement without decentering. However, the nasal direction of the lid movement will generate rotation in a soft lens. A good soft toric lens design will resist the rotational force of the blink while providing sufficient vertical lens movement for a good lens fit. Unfortunately, there is not a strong correlation between lid position and predicting rotation of the toric lens.5
Lens Stabilization Designs There are several different stabilization techniques on the market today. It is important to understand the stabilization design for each lens to aid in both troubleshooting the lens fit and managing vision issues.
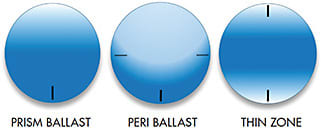
Prism-ballasted lenses are thinner at the top and become thicker toward the bottom of the lens, creating base-down prism. The primary force acting on the lens is the upper eyelid exerting pressure on the thin upper edge of the lens, causing the thicker edge to move away from the upper lid with each blink. One disadvantage of this design is that the prism throughout the lens generates vertical optical prism. This becomes problematic if a patient wears a prism-ballasted toric lens on only one eye, resulting in vertical prism, and a spherical lens on the other eye without the vertical prism. The increased thickness of the center and inferior edge of a prism-ballasted lens can also decrease the oxygen transmission through the soft lens material and potentially induce hypoxia-related lens wear complications.
Peri-ballasted design lenses are similar to prism-ballasted lenses in their interaction with the lid during the blink. The primary difference is that the prism is not in the optical zone of the lens. The thickness variable is only in the lenticular periphery of the lens. This design can result in a decreased center thickness and improved optical quality.
Both prism-ballasted and peri-ballasted lenses have the base of the lens orienting inferiorly on the eye. For this reason, these lenses typically include rotation markings at the most inferior portion of the lens at 6 o’clock.
Thin-zone design lenses are thinnest at the superior and inferior edges and are thicker in the middle portion of the lens. The thinner superior and inferior edges of the lens interact with the upper as well as with the lower lids during the blink to stabilize the lens. A variation of this design has four thicker areas in the midperiphery adjacent to the optic zone, with a thinner superior and inferior edge. These “bumps” on the lenses interact with the position of the eyelids to stabilize the lens. As thin-zone design lenses are not base-down lenses, there is no “up” or “down”; so, these lenses will often have two orientation markings that are either in the horizontal positions (3 o’clock and 9 o’clock) or the vertical positions (12 o’clock and 6 o’clock) (Figure 2).
While these stabilization designs are mostly generated on the front surface of the lens, some lenses add back-surface toricity to aid in additional stabilization, especially in cases in which there is a great amount of corneal astigmatism.
The lens markings in a given lens brand will be in the same location on the lens regardless of the lens power or axis. The lens edge and periphery can be thought of as a carrier or frame for the optics in the center of the lens, where different cylinder axes are orientated accordingly while the outer carrier is in the same position on the eye.
Managing Lens Rotation The goal of the lens stabilization designs is to minimize lens rotation on the eye to provide stable correction of astigmatism and to minimize visual blur. Even with the best design, some lens rotation is still possible. Consistent rotation of the lens can be compensated for by adjusting the cylindrical axis of the lens power. However, if the rotation is not consistent, any attempt to compensate for this moving target of the axis will not be effective.
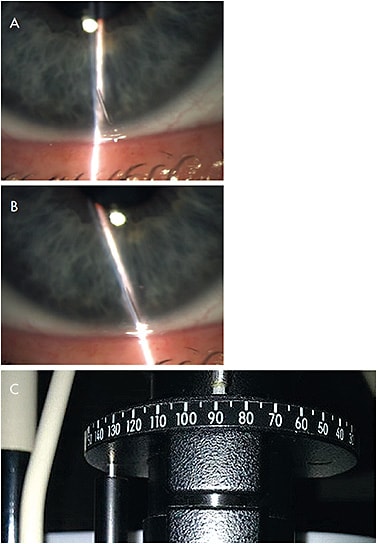
The first step in managing soft toric lens rotation is to know the amount and direction of the rotation. This can be determined during slit lamp evaluation of the lens fit. While viewing the lens, observe the toric markings and the lens position. A thin vertical beam of the slit lamp light can be lined up with inferior lens markings. If the markings of the lens are oriented horizontally, the slit lamp beam can be rotated or set perpendicular to the horizontal marking. If the lens is rotated and the markings are not straight up and down, rotate the slit lamp light beam to align with the lens marking (Figure 3). Note the amount of rotation of the slit lamp beam, which is indicated in degrees on the slit lamp, and observe the direction of the rotation from the examiners’ view. If the marking is sitting to the right of the 6 o’clock position, the lens is rotated counter-clockwise. Conversely, if the marking is to the left, the lens is rotated clockwise.
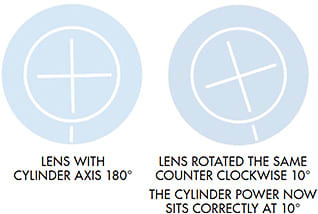
When the lens is rotated counter-clockwise, the cylinder axis in the contact lens is in a position with an increased axis. For example, if the lens has an axis of 10º, a counter-clockwise rotation puts the cylinder axis at 20º on the eye (Figure 4).

To compensate for the counter-clockwise rotation, subtract the amount of rotation from the cylinder axis of the lens in the optic zone. In the previous example, 10º will be subtracted from the original 10º lens axis, so a lens with an axis of 180º should be placed on the eye. With a consistent 10º counter-clockwise rotation, this lens with a cylinder axis of 180º should now sit at the correct 10º on the eye (Figure 5). The opposite is true for a lens rotated clockwise, in which the amount of rotation is added to the cylinder axis of the lens. In our example, the new lens axis would then be 20º. A simple pneumonic to remember this is LARS: Left Add, Right Subtract. This compensation is successful only when the rotation of the lens is very stable. The lens marking and the amount of rotation should be in the same location in the compensated lens; only the axis of the lens power on eye will change.
If poor vision persists with a stable fitting lens after cylinder axis compensation, the next step is to perform a sphero-cylindrical over-refraction (SCOR) in the phoropter to refine the lens power. When two cylindrical lenses are put together in different axes, the cross-cylinder creates a cylinder power in a different magnitude and axis.
If the SCOR results in a cylinder power that has the same axis as the spectacle prescription, that contact lens is not correcting the cylinder power needed. When this happens, fit another lens with the cylinder power increased by the amount of the SCOR. If the SCOR results in a cylinder power that is 90º from the spectacle and contact lens axis, this lens is over-correcting the astigmatism. A lens with less cylinder correction should be selected.
If the SCOR results in a spherical equivalent of plano in a different axis compared to the spectacle prescription—for example, +0.50 –1.00 x 035—then the reason for the poor vision is rotation of the toric lens and misalignment of the axis. If rotation is noted on lens evaluation, the misaligned axis can be compensated for as long as the axis for the cylinder power needed is available. If the spectacle axis falls in between available contact lens axes, a cross cylinder can create some visual blur even if the lens does not appear to be rotated.
When the result of the SCOR does meet any of the criteria mentioned previously, there is a significant cross-cylinder effect that may be resulting from incorrect contact lens power in combination with axis misalignment. In this case, a cross-cylinder calculator can be used to calculate the power of the correct contact lens needed. Such calculators require input of the spectacle prescription as well as the contact lens power and resultant SCOR to calculate the power of a new contact lens that should provide improved vision for the patient. These calculators are available on online websites as well as through software applications for computers and personal handheld devices.
Inconsistent rotation of a soft toric lens can result in fluctuating vision. Unfortunately, no amount of lens power or cylinder axis compensation will correct this variable vision. A lens parameter change to adjust the fit of the lens is necessary to stabilize the lens and vision. In a custom soft toric lens, the base curve and diameter can be changed to modify the sagittal depth of the lens to better fit the eye and improve stability of rotation. Another possibility is to change the lens stabilization design, for example, from a peri-ballasted lens to a thin-zone design. Lens material bulk properties, such as modulus or water content, can also affect the lens stability on the eye.
Custom soft toric contact lenses may be able to manage issues with unsatisfactory performance of standard soft toric lenses. Custom lenses can be made in a wide range of base curves and diameters for patients whose horizontal visible iris diameters (HVIDs) or central corneal curvatures fall outside of common dimensions and who may find that standard soft toric lenses are uncomfortable with excessive lens movement. Many custom soft lens manufacturers have online tools and calculators that use a patient’s HVID and corneal curvature to help determine the appropriate base curve and diameters for the patient. As custom lenses are made to order, they are available in any specific power that is needed, with cylinder powers in 0.1DC steps and axes in 1º steps. If rotational stability is an issue, the amount of prism ballast can also be adjusted to decrease axis misalignment of the lens.
CONCLUSION
Fitting soft toric lenses to manage astigmatic refractive error is relatively straightforward. Soft toric lenses correct the refractive astigmatism in the spectacle correction. Becoming skilled at fitting contact lenses for astigmatism can help improve the vision and the contact lens experience for patients who have low astigmatism and have experienced visual compromise with spherical lenses.
There are still so many patients who have been told that they are not contact lens candidates because of their astigmatism. Being able to help these patients enjoy the vision and benefits of contact lens wear can be very rewarding and can address an important unmet need of the contact lens-wearing population. CLS
REFERENCES
- Nichols J, Fisher D. Contact Lenses 2018. Contact Lens Spectrum. 2019 Jan;34:18-23, 50.
- Young G, Sulley A, Hunt C. Prevalence of astigmatism in relation to soft contact lens fitting. Eye Contact Lens. 2011 Jan;37:20-25.
- Richdale K, Berntsen DA, Mack CJ, Merchea MM, Barr JT. Visual acuity with spherical and toric soft contact lenses in low- to moderate-astigmatic eyes. Optom Vis Sci. 2007 Oct;84:969-975.
- Jackson JM. Toric Lenses for Today and Tomorrow. Contact Lens Spectrum. 2016 Aug;31:28-32.
- Young G, Hunt C, Covey M. Clinical evaluation of factors influencing toric soft contact lens fit. Optom Vis Sci. 2002 Jan;79:11-19.




