Billing and coding are a source of frustration for both practitioners and patients. Reimbursement methods and rates vary drastically between carriers and even sometimes between patients. Often, it is difficult to obtain a clear answer on what the proper method is, what codes to use, and how to determine coverage. This was a challenge for me as I entered into a private practice that had no experience with billing and coding for specialty lenses, so it took much time and effort (and many mistakes) to finally learn some of the best tactics. I hope to share some of those strategies with you so that you may avoid a few of the headaches and mistakes that I made early in my career.
As a general rule of thumb, I like to think of billing and coding like taxes: you can take the exact same receipts, bills, and income to one accountant, and he or she will interpret them differently than would another accountant looking at the same information. This can be extremely annoying, as it seems like billing and coding should be very black and white. But, sorry folks, it is not.
Each insurance company has its own guidelines, reimbursement rules, and fee structures. Even worse, you can’t even get comfortable with Insurance Plan A, because the plan could vary from patient to patient. The best thing to do is be prepared; practitioners should also be willing to deal with (or have staff members handle) insurance companies for authorizations and clarifications.
FOLLOW THE STEPS
Step 1 The first step for specialty lens billing is to contact a patient’s insurance (vision and/or medical) and obtain a prior authorization for medically necessary contact lens coverage. This may not occur until after you see patients, so often it cannot be done prior to their appointment. For this reason, I see all patients for an initial consultation so that I have data and information to use when contacting the insurance companies. You will often need the following information when speaking with an insurance company:
- Patient’s full name, date of birth (DOB), identification (ID) number, etc.
- Diagnosis, with proper ICD codes
- Proper CPT code (this is the type of lens fitting)
- V code(s) (this is the lens type)
- Usual and customary (U+C) rates
- Patient’s remaining deductible, co-pays, and co-insurance rates
- Expected reimbursement rate from insurance company. This is extremely important because often the insurance company will say “The patient is fully covered,” and practitioners will assume that this means that their entire usual and customary rate will be reimbursed, but this is usually not the case. Make sure to ask the representative how much you can expect in reimbursement so that you and the patient are not surprised. Sometimes, they will refer you to the manual and contract that was signed when you originally signed up for the insurance, so you may need to search for that or access that information online.
An example may look like this:
- Jane Doe, 1-1-2001, ID# 1234, Plan XYZ
- Diagnosis: corneal transplant status, ICD 10 code Z94.7
- CPT code(s): 92310 (Prescription of Optical and Physical Characteristics of and Fitting of Contact Lens, with Medical Supervision of Adaptation; Corneal Lens, Both Eyes, Except for Aphakia)
- V code(s): V2511-RT and V2511-LT (contact lens, GP, toric, per lens)
- Usual and customary rate: $500 for 92310, $250 for V2511-RT, and $250 for V2511-LT
- Patient has met his or her deductible in full; the co-pay for medically necessary contact lens services and materials is $25
- The expected reimbursement from the insurance based on diagnosis code, CPT code, V codes, and allowed amounts is $400 total, according to Mary at Insurance Company A.
In this example, you can see that, even though the amount being billed is $500 for the fitting and $250 per lens, the insurance company will only pay $400, per the patient’s plan. You must check the insurance contract to see whether balance billing is allowed (in most cases, it is not). Balance billing means that it is acceptable to bill the remaining difference to the patient; in this case, the U+C is $1,000 and the insurance payment is $400, so the difference would be $600. Each patient plan and insurance plan is unique, so it is important to check every time.
Tip: Be sure to obtain the representative’s name or employee ID and the date/time of the phone call along with a reference number for the phone call. That way, if there are questions later, you can call the insurance company and reference the past conversations. If you can obtain the information in writing (for example, in a fax or online authorization), this is also helpful; having information in writing can help if any discrepancies should arise.
You may also need to submit a letter of medical necessity along with information such as refraction, best-corrected visual acuity, topography, and clinical notes. In some cases, this information is reviewed before determining coverage. In other odd cases, insurances require the best-corrected visual acuity through a contact lens (to determine whether the vision is improved through a contact lens).
Keeping in mind that the practitioner is ultimately responsible, be sure that you or a staff member are fully aware of the eligibility for medically necessary contact lens benefits, and be certain that you obtain all necessary information required in case of an audit. For example, if an insurance company requires a topography of steep keratometry values greater than 59D, make sure that information is readily accessible in the event that a company requests it.
Step 2 After your office has determined insurance coverage, it is time to explain everything to the patient. This is extremely important and represents a critical step in the billing process. During this phase, it is helpful to have an Advanced Beneficiary Notice (ABN) and a written contract that outlines all of the pricing and office visits. An ABN is a written notice that a provider gives to patients before any services are received. Essentially, it explains that if the insurance company does not pay for the services rendered, the patients are financially responsible for payment. This is important to have patients sign, especially in cases in which you are uncertain whether the insurance company will accept the submitted billing codes. A written contract is also advisable, because it outlines all of the patient visits, along with fees, so that patients are fully aware of all costs involved. The contract also should outline the global period (if applicable) start and end date, so that patients know on what date their predicted services will end. Other information should include lens upgrade fees and lens warranties (i.e., what occurs if a lens cracks or gets lost). Describing all fees in detail will ensure that patients have a good understanding of the entire process and will prevent many headaches.
Step 3 Once insurance coverage is verified and a patient has signed the ABN and/or written contract, it is time to proceed with the specialty contact lens fitting. After the fitting is complete, it is OK to bill the insurance company with the proper ICD and CPT codes. Please check with each insurance company on the billing structure for medically necessary contact lenses; some require practitioners to bill each visit separately, while others want them to bill the entire fitting and follow-up care as one fee (see example below).
| CODE | YOUR FEES |
|---|---|
| Scleral lens fit OD & OS 92313 | $200 |
| Scleral lens device V2531-RT | $400 |
| Scleral lens device V2531-LT | $400 |
| One-week follow up | Included in global fee (99xxx code not used) |
| Total billed to vision insurance | $1,000 as one lump sum for all services and lenses |
With Insurance A, you would bill the lens fitting and both lenses along with any follow-up care to the insurance as one lump sum. Most vision insurances are billed this way. They usually accept a contact lens fitting code (9231X) as one fee, then the V codes as another fee. They usually do not accept 99XXX codes that you may use for the follow-up care, so make sure to account for this when billing as one global fee.
| CODE | YOUR FEES |
|---|---|
| Scleral lens fit OD & OS 92313 | $200 |
| Scleral lens device V2531-RT | $400 |
| Scleral lens device V2531-LT | $400 |
| Scleral lens dispense 99213 | $100 |
| Scleral lens follow up 99213 | $100 |
| Scleral lens follow up 99213 | $100 |
| Total billed: $1,300; each visit is billed separately |
In the example for Insurance B, you would bill every visit to the insurance company. This company doesn’t require a global fee; each time that you see a patient, it is billed to the insurance company. Most medical insurances are billed this way. Keep in mind that just because you bill a certain amount to the insurance does not mean that you will receive that amount. You must refer to the contracted insurance rates in the provider manual to determine how much will be reimbursed.
| CODE | YOUR FEES |
|---|---|
| Scleral lens fit OD & OS 92313 | $200 |
| Scleral lens device V2531-RT | $400 |
| Scleral lens device V2531-LT | $400 |
| Total billed to vision insurance | $1,000 as one lump sum for all services and lenses |
| CODE | YOUR FEES |
|---|---|
| Scleral lens fit OD & OS 92313 | $100 |
| Scleral lens device V2531-RT | $200 |
| Scleral lens device V2531-LT | $200 |
| Total collected from insurance | $500 |
In this example, you billed out $1,000 for the contact lens fitting and devices, but according to your contracted rates for that insurance, the insurance company only paid you $500. This is very typical, and each insurance has a different contracted rate. This is why it is so important to obtain prior authorizations before fitting medically necessary lenses. As the practitioner, you should be fully aware of the expected reimbursement prior to initiating any contact lens fitting.
WHAT QUALIFIES AS A MEDICALLY NECESSARY CONTACT LENS?
Each insurance company has its own rules and guidelines on what qualifies for medically necessary contact lenses. Some have a definitive list of patient diagnosis codes that would qualify them for medically necessary lens benefits. Some may also further differentiate diseases into mild, moderate, and severe. For example, Eyemed insurance separates keratoconus patients as mild/moderate or advanced/ectasia. The provider manual has a section specifically for the classification, so it is important to refer to that section when classifying a patient so that you know into which category that patient falls.
Medically necessary contact lenses can range from simple soft contact lenses to GP lenses to custom scleral lenses. For example, if patients have high ametropia, defined as –10.00D or higher according to their insurance plan, they could qualify for medically necessary contact lenses. Even though a standard soft contact lens might be used, because of the patients’ vision, they could qualify for that benefit. Again, every insurance company defines this differently; one insurance may define high ametropia as –10.00D, while another defines it as –12.00D.
CPT Codes CPT codes are used to bill the fitting portion during the medically necessary contact lens fitting. Your U+C fees will be set by your office. Table 1 provides a sample list of common CPT codes used for contact lens fittings.
| CODE | DESCRIPTION |
|---|---|
| 92310 | Use this code for any corneal lenses, except in the case of aphakia. This would include soft contact lenses, corneal GP lenses, intralimbal lenses, and, in some cases, hybrid lenses and custom soft lenses. |
| 92311 | Use this code when you are fitting aphakia in one eye only with a corneal lens. |
| 92312 | Use this code when you are fitting aphakia in both eyes with a corneal lens. |
| 92313 | Use this code when fitting a corneoscleral lens or scleral lens. There is currently not a CPT code for a full scleral lens, so this one is the closest for now. |
| 92072 | Use this code when fitting a patient who has keratoconus. Keep in mind that many insurances have strict guidelines on what qualifies as keratoconus. Also, please refer to the provider manual for subsequent fittings. Some practitioners previously believed that this code could only be used once for the lifetime of the patient; however, this is an incorrect assumption. |
| 92071 | Use this code when fitting a contact lens for treatment of ocular surface disease. I tend to reserve this code for when I am using a bandage contact lens to treat diseases such as superficial keratitis, corneal abrasions, recurrent corneal erosions, etc. |
Note: Some insurance companies allow only a set of CPT codes from which to select. For example, an insurer may have 92310 and 92313 as the only options. In this case, either refer to the provider manual or contact the insurance company so that it can help you select the most appropriate code for your specific patient case.
V Codes These codes are used to bill the supply of the lens. In some cases, the supply is not billed separately, but the majority can be billed with a separate supply, which is the V code. Many practitioners are probably accustomed to billing V codes when billing for ophthalmic lenses, such as single vision or bifocals. The same holds true with contact lenses; use the proper V code to bill for the unique contact lens type.
V codes may have modifiers indicating right and left eye, and you may also have to indicate the quantity of lenses. For example, V2521 RT quantity 12 would mean that you are billing a hydrophilic soft toric contact lens for the right eye, and the quantity is 12 lenses; this assumes that the insurance plan allows for an annual supply and that the prescribed lens has a monthly replacement schedule. Table 2 provides a sample list of common V codes used for medically necessary contact lenses.
| CODE | DESCRIPTION |
|---|---|
| V2510 | Contact Lens, GP, Spherical, Per Lens |
| V2511 | Contact Lens, GP, Toric, Per Lens |
| V2512 | Contact Lens, GP, Bifocal, Per Lens |
| V2513 | Contact Lens, GP, Extended Wear, Per Lens |
| V2520 | Contact Lens, Hydrophilic, Spherical, Per Lens |
| V2521 | Contact Lens, Hydrophilic, Toric, Per Lens |
| V2522 | Contact Lens, Hydrophilic, Bifocal, Per Lens |
| V2523 | Contact Lens, Hydrophilic, Extended Wear, Per Lens |
| V2531 | Contact Lens, GP, Scleral, Per Lens |
| V2599 | Contact Lens, Other Type (i.e., Hybrid) |
| V2627 | Scleral Cover Shell |
| V2799 | Vision Item or Service, Miscellaneous |
HOW DO I SET UP A FEE SCHEDULE FOR MEDICALLY NECESSARY CONTACT LENSES?
This is a common question that is asked by many providers, and I also had to determine what was fair for my practice. There are a few strategies for determining an appropriate fee schedule. There is no right or wrong method; practitioners should use the one that works best for them.
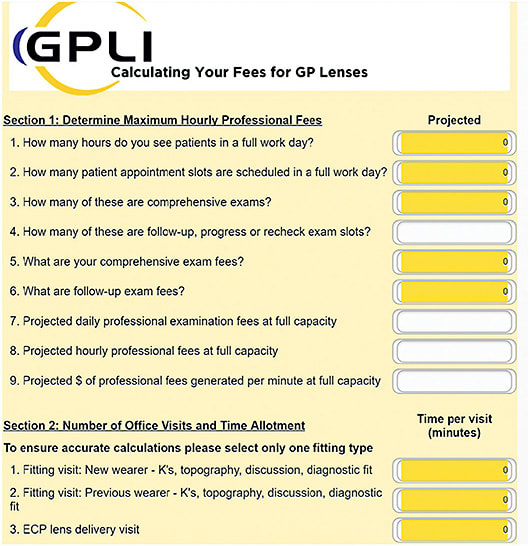
Method 1 Use a fee calculator. The GP Lens Institute (GPLI) offers a free calculator on its website (www.gpli.info ). Simply click on “Resources” and then “Professional Fee Calculator.” You can then plug in answers to the questions, and the tool will calculate some of the fees (Figure 1).
Method 2 Determine your fixed costs and divide by the number of complete annual examinations to determine chair cost (Fixed costs / complete annual examinations = chair cost per examination). For example, $260,876 / 2,156 = $121 per examination. In this example, once the chair cost per examination is known, determine how many visits the contact lens fitting may take to calculate the grand total.
Method 3 Determine the amount of profit per examination and the number of examinations per hour. For example, let’s assume the following:
- Profit per examination = around $250
- Examinations per hour = 2 = $500 per hour
- Time spent with scleral lens patient (fit + dispense + follow-up care) = ~3 hours = $1,500
Let’s also assume that you know that per examination, the amount of profit is about $250. If you see two examinations per hour, then that would mean you generate approximately $500 per hour. You can then use the numbers above as a benchmark to determine a fair price for a contact lens fitting. In this example, a fitting takes one hour, the dispense will take another hour, and two follow-up visits will take 30 minutes each. Therefore, you have a total of three hours with this patient. So, if you generate $500 per hour and you expect to spend three hours with this patient total, the cost would be, at minimum, $1,500. However, you should charge more than this because if you just kept your schedule the same and continued to see regular examinations, you would have generated that $1,500 anyway. Therefore, because medically necessary contact lenses are a specialized service, you should charge more for your time and expertise with this case.
FINAL THOUGHTS
To maximize efficiency and understanding of billing medically necessary contact lenses, it is advisable to read through your provider manual to know exactly what that specific insurance carrier will cover. Contacting insurance companies and having them walk you through the information can also be useful. Also be sure to obtain prior authorization before initiating any contact lens fitting so that there are no surprises.
As with everything, practice makes perfect. The more you bill medically necessary contact lenses, the easier it will become for you and the staff. Take advantage of articles in magazines, webinars, boot camps, and lectures to learn more and to stay relevant. CLS




