
Keratoconus GP Fitting Findings— a Clinical History
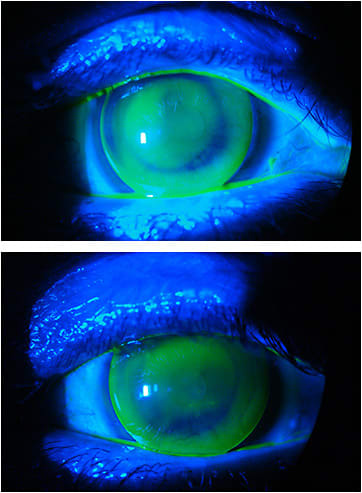
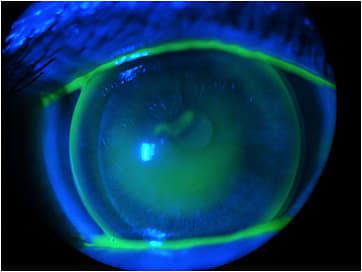
The images this month show a case of keratoconus. We will analyze the history and clinical findings of this case observed over 30 years. The first image shows a new GP keratoconus lens design OD with a nice fluorescein pattern. The fitting demonstrates apical clearance without touch and optimal clearance, and the aspheric periphery provides excellent comfort and lacrimal exchange. We also observed Vogt’s striae near the apex of the cone OD. The second image shows an old lens OS that the patient came in wearing in 2019 because he had lost his newer lens; we can observe severe touch at the apex and excessive fluorescein around the apex of the corneal ectasia.
History
1990
This patient is currently a 71-year-old business entrepreneur who first visited our clinic in March 1990. We fit him with our GP keratoconus lens design, which he has worn since that time. He wore the first pair for three years, then returned with complaints of discomfort and tearing.
1992
In 1992, he presented with a corneal erosion OS. It was treated and resolved, but in 1993 he returned with similar complaints. At that time, we had to cauterize a recidive erosion.
1993
In 1993, the corneal GP lens parameters were:
OD base curve (BC) 52D x 45D, power –11.00D, overall diameter (OAD) 9.4mm, optic zone (OZ) 6.0mm, Dk 45 (VA 20/25)
OS BC 54D x 45D, power –12.00D, OAD 9.4mm, OZ 6.0mm, Dk 45 (VA 20/30)
1996
In 1996, the patient was refit with new corneal GP lenses. We observed that the OD cornea was stable with minimal changes and that the keratoconus had progressed OS. We refit the patient with the following parameters:
OD BC 52D x 45D, power –12.50D, OAD 9.5mm, OZ 6.0mm, Dk 45 (VA 20/25)
OS BC 56D x 45D, power –14.50D, OAD 9.4mm, OZ 6.0mm, Dk 45 (VA 20/30)
Over the next five years, both eyes remained relatively stable, and we observed minimal changes. Refits were done with similar lens parameters.
2000
In May 2000, the patient presented with a corneal erosion OD; it was treated and resolved within a few days. He was refit OD with a BC 52.50D x 45D to avoid recurrent erosion.
2001 to 2003
In November 2001 and also in June 2003, we reordered new lenses with the same parameters:
OD BC 52D x 45D, power –12.50D, OAD 9.5mm, OZ 6.0mm, Dk 50
OS BC 56D x 45D, power –14.50D, OAD 9.4mm, OZ 6.0mm, Dk 50
2008
In 2008, we observed the same recurrent corneal erosion OS, and we refit him with a steeper BC. We also prescribed reading glasses of +2.75D. The OS GP parameters were OS 57.50D x 45D, power –14.00D, OAD 9.5mm, OZ 6.0mm (Figures 3 and 4).
2010
Then in May 2010, we refit the patient OD only, as we observed a paracentral lesion (Figure 5). He was treated with Regencel (retinol acetate, Latinofarma), which is similar to Epitezan (Allergan), and lacrimal tears for healing and lubrication. For OS, in which there were previous findings of corneal erosion, we observed a stabilization and no episodes of erosion since 2008 (Figure 6).

2013
In December 2013, we refitted the patient with the following parameters:
OD BC 52.50D x 45D, power –12.00D, OAD 9.8mm, OZ 6.5mm, Dk 50 (VA 20/25+3)
OS BC 58D x 45D, power –14.50D, OAD 9.8mm, OZ 6.5mm, Dk 50 (VA 20/25–1)
Note that the keratoconus remained relatively stable from 2007 until 2013, and surprisingly VA OS improved one line. The fitting demonstrated an excellent fluorescein pattern, lens position, and mobility (Figures 7 and 8).

2017
In March 2017, we reordered a new pair of GPs with the same parameters from 2013; VA remained 20/25 OD and OS. We prescribed a preservative-free lubricating eye drop t.i.d.
In August 2017, during a follow-up visit, we observed apical touch OS (Figure 9). We refitted the patient with a new GP keratoconus lens (Figure 10) with the following parameters:
OS BC 60D x 45D, power –16.50D, OAD 9.8mm, OZ 6.5mm, Dk 50


The new lens OS fit with a steeper central base curve, and minor adjustments to the posterior curves resulted in an excellent fitting pattern. Despite the advanced keratoconus OS, the corneal pachymetry remained stable with a reasonable stromal volume, which was good because it did not indicate a serious risk of acute hydrops.1
Also, the patient never developed central corneal scars, which would reduce visual acuity. The goal of GP fitting in keratoconus is to always preserve the corneal apex. Fitting a keratoconus lens to avoid touch at the apex and to allow good tear exchange is a healthy direction to go.
2019
In May 2019, we saw the patient to refit a new pair of lenses. We observed minor changes at the fitting. The overall fit seemed stable, but we adjusted BC and power to prevent new erosion or keratitis and also to achieve the best possible visual acuity. The new pair had the following parameters:
OD BC 53D x 45D, power –12.00D, OAD 9.9mm, OZ 6.5mm, Dk 50 (VA 20/20–3)
OS BC 60D x 45D, power –17.00D, OAD 9.9mm, OZ 6.5mm, Dk 50 (VA 20/30+3)
In June 2019, we observed a light apical touch and a mild erosion OD (Figures 11 and 12), so we decided to change the base curve. The OS remained stable, with an excellent fluorescein pattern.

The new GP lens OD was a perfect fit, showing an optimal fluorescein pattern, lens position, and mobility (Figure 13). The lens parameters were:
OD BC 54D x 45D, power –13.00D, OAD 10.0mm, OZ 6.5mm, Dk 50 (VA 20/20)

Corneal Biomicroscopy
It is interesting to mention that over all of these years of caring for this patient, we did not need topography or anterior corneal tomography to help with the fittings. The corneal evaluation was always by slit lamp biomicroscopy observation. The fluorescein pattern of a known lens was quite sufficient to estimate the changes observed during the last 30 years.
At the June 2019 visit, we decided to perform corneal tomography and specular microscopy. The findings were compatible with his condition. The specular microscopy showed a normal endothelial cell density average.3,4 It is important to reiterate that this patient has worn corneal GPs for 30 years, always with a medium-Dk material and a design that allows the best tear exchange. Also, due to his age, we educated him about the importance of blinking when using a computer or smartphone and also to instill nonpreserved lacrimal tears t.i.d.
Discussion
Keratoconus patients and those who have other irregular cornea conditions such as pellucid marginal degeneration, post-graft, and post-refractive surgery represent almost 85% of the patient base in our clinic, but keratoconus is the main pathology that we see for specialty lens fitting. In almost 100% of the fittings, we use specialty corneal GPs or scleral lenses that range from 16.0mm up to 21.0mm in diameter. The main goals in fitting these irregular cornea conditions with corneal GPs or sclerals are to offer comfort, the best visual acuity possible, and also to maintain the corneal physiological health. It is of utmost importance to offer the proper option at the right time and also to instruct patients to not rub their eyes, to properly clean their lenses, and also to visit us for periodic follow ups.
Many patients put off visiting us while the contact lenses feel fine; sometimes we don’t see them again for three or four years, sometimes even more. In some cases, this can lead to an interruption of lens wear for a few days until we can perform a valid new exam and determine the new fitting.
Keratoconus progression generally happens more aggressively in younger patients, usually from 14 to 25 years, and then the episodes of progression tend to be less acute and more spaced out in time. During the 30 years that we cared for this patient, we saw a few other cases that we referred for penetrating keratoplasty or for the more recent deep lamellar keratoplasty. But in the majority of cases, keratoconus patients may benefit from corneal GP or scleral fittings that help them achieve very reasonable visual acuity, with good comfort and health.
Conclusion
In the 50 years of our clinic, we’ve seen that specialty contact lens fitting still is and will continue to be one of the most important options to help patients who have irregular cornea conditions. In most keratoconus cases, the visual acuity will be much more predictable and accurate than that with any surgical treatment. Some cases may benefit from intracorneal ring segments in mild cases and from corneal transplants, especially when central corneal opacities are present. However, even in most cases that have mild opacities, specialty contact lenses may allow these patients to achieve a satisfactory visual acuity.
References
- Greenwald MF, Vislisel JM, Goins KM. Acute Corneal Hydrops. Eye Rounds.org. 2016 Aug 3. Available at https://webeye.ophth.uiowa.edu/eyeforum/cases/241-Acute-Corneal-Hydrops.htm . Accessed June 1, 2020.
- Thimons J. Managing Acute Corneal Hydrops in Keratoconus. Review of Cornea and Contact Lenses. 2015 April. Available at https://www.reviewofcontactlenses.com/article/managing-acute-corneal-hydrops-in-keratoconus . Accessed June 1, 2020.
- El-Agha MS, El Sayed YM, Harhara RM, Essam HM. Correlation of Corneal Endothelial Changes With Different Stages of Keratoconus. Cornea. 2014 Jul;33:707-711.0
- Goebels S, Eppig T, Seitz B, Szentmàry N, Cayless A, Langenbucher A. Endothelial alterations in 712 keratoconus patients. Acta Ophthalmol. 2018 Mar;96:e134-e139.




