The practice of orthokeratology (ortho-k) has evolved over many decades, from accidental corneal molding with glass contact lenses to highly specialized, topographical data-driven corneal reshaping with GP lenses. While improved uncorrected vision was once just an added bonus for some patients who were wearing hard lenses, it is now a valid option for patients who have many different types and levels of refractive error. Modern contact lens practitioners should find it easier than ever to learn to prescribe and implement ortho-k in their practices, thanks to ongoing research and development of this modality.
FROM ORIGINS TO TODAY
Reports of using contact lenses to shape corneal tissue to modify refractive error date back to the 1950s and 1960s, but they were primarily isolated case reports and incidental findings.1-3 Better-quality research emerged with a collection of clinical studies published by Kerns in the late 1970s.4 Early attempts at refractive error correction were constrained by the lack of computerized topographical corneal data and by the lens materials available at the time (primarily polymethyl methacrylate). Consequently, interest in ortho-k waned, as the utility of unpredictable corneal molding with daytime-only wear of contact lenses was limited.3
Technological breakthroughs in the 1980s and 1990s gave practitioners who were interested in ortho-k significant improvements with which to work. GP materials that reduced the risks of hypoxia and corneal edema allowed for healthier overnight wear of GP contact lenses. Computerized topography and computer-driven lathing systems resulted in better lens design and more patient-specific lens customization to improve the accuracy and predictability of results and to provide faster improvements in uncorrected visual acuity.
A standard corneal GP lens consists of a back-optic-zone radius with peripheral fitting curves, and early ortho-k involved simply flattening or steepening the central base curve of this type of lens. To treat myopia, practitioners commonly prescribed multiple lenses with progressively flatter base curves to reach the desired refractive outcome,5 because going too flat initially would result in poor lens centration and decentered treatment zones.
Modern ortho-k lenses use a reverse geometry design. This consists of a central base curve/optic zone radius surrounded by a reverse/steeper curve that allows for tissue distribution and improves the speed at which corneal molding occurs. Farther out onto the periphery are one or two alignment curves that optimize centration and a peripheral curve region that allows for proper tear exchange.6
In 2002, the first contact lens for overnight ortho-k was approved by the U.S. Food and Drug Administration (FDA). These reverse geometry lenses, labeled Class III devices, were approved to treat myopia up to –6.00D with or without 1.75D of cylinder, with no age restrictions. A few years later, another company received FDA approval for overnight ortho-k to treat myopia and low astigmatism with lens designs manufactured through a number of different laboratories. These approvals gave ortho-k a layer of regulation, adding reassurance for practitioners, patients, and parents who were interested in trying this unique but relatively unknown vision correction technique.
Numerous options and methods for fitting ortho-k lenses have been fine-tuned over decades of research and development. Practitioners need only to become certified in fitting these lenses and to find a laboratory that provides reliable service and consultation to begin fitting this modality.
ENHANCED FITTING CHOICES
Many early ortho-k designs required practitioners to invest in large sets of diagnostic lenses or design-specific fitting software. Having lenses available to address fitting issues in the office can be convenient, but some practitioners felt that the initial investment and the ongoing storage, maintenance, and replenishment of extensive fitting sets could be overwhelming. However, basic modern fitting sets have been streamlined to incorporate only the most commonly needed lenses and are often more affordable or are even reimbursed after a predetermined number of lens orders. As for the fitting software, the learning curve and expense of some applications, while not necessarily outrageous (particularly if chair time is reduced), can be intimidating to some practitioners.
While utilization of fitting sets is still common and sometimes necessary, many ortho-k designs now offer online calculators to fit empirically from refractive and topographical data. Many of these designs boast a first-lens success rate of more than 90%, with easy-to-understand data entry and interpretation. This can be appealing to practitioners who don’t have the means or the patient base to invest in a fitting set.
A cautionary note: Some lenses do not come with warranty support, and costs can add up quickly if multiple lens changes are required. Practitioners must familiarize themselves with lens and shipping costs as well as with warranty availability, length, and conditions. A novice fitter may prefer a 90-day warranty (in case of multiple lens changes) or a fitting set (to facilitate learning while observing different lens parameters on the same day/patient) over the convenience of empirical ordering.
EXPANSION OF TREATABLE REFRACTIVE ERRORS
Ortho-k has been, and largely still is, primarily for myopia correction, but we can now address astigmatism, hyperopia, and presbyopia as well. In fact, an excellent way to grow an ortho-k practice is to consider the candidacy of current patients rather than to wait for “ideal” young patients who have myopia to come along. As refractive errors other than myopia are considered off-label for ortho-k, it’s important to inform patients of this before beginning treatment.
Correcting hyperopic refractive errors with base curves that are steeper compared to the central corneal curvature has been possible for decades, but it has not been employed to the same extent as ortho-k for myopia correction has. The amount of hyperopia that can be corrected is significantly less compared to the amount of myopia that can be corrected, and the refractive effect achieved seems to be notably less than what’s predicted by corneal/base curve calculations.8 However, patients who have mild hyperopia or presbyopia can benefit from ortho-k treatment. These patients are often poor candidates for laser-assisted in situ keratomileusis (LASIK), and they may welcome the opportunity for independence from spectacle and daytime contact lens wear.
Good candidates for hyperopic ortho-k include:
- patients who have presbyopia without other notable refractive errors who are open to monovision correction;
- patients who have low-to-moderate, non-presbyopic hyperopia;
- presbyopic hyperopes looking to reduce their dependence on spectacles but don’t mind their occasional use as needed for reading.
Although somewhat more challenging, ortho-k can be prescribed for patients who have less-than-desirable outcomes after refractive surgery. If the shape of the cornea is relatively regular and not excessively oblate, and if there is no ectasia or high refractive error, it is possible to fit these disappointed patients. Ortho-k can work particularly well for patients who have mild myopia regression and are not eligible for a LASIK enhancement procedure.9
When astigmatism is present, modern ortho-k designs offer some solutions. When attempting to correct low-to-moderate astigmatism, the challenge is to maintain centration well enough to establish a well-centered treatment zone. If the corneal toricity is in a small area and is centralized, a spherical ortho-k lens that maintains good centration can effectively treat most of the astigmatic refractive error. If the toricity covers a wider area or is more extensive (i.e., limbus-to-limbus), a design that employs toric peripheries will help maintain centration. Such lens designs are currently available in the United States and internationally.
To treat moderate or high astigmatism, corneal reshaping lenses require toric base curves with or without toric peripheries to fully address the correction needed. These designs are much less common, but they may become more readily available in the future, particularly if interest in myopia control continues to grow.
MYOPIA CONTROL
The increasing demand for effective options for myopia control may offer the best potential for growth in ortho-k. An extensive literature review by Walline and colleagues determined that ortho-k slows axial length growth more effectively than single-vision contact lenses do.10 We don’t have to look far to find numerous studies suggesting that ortho-k-induced peripheral retinal myopic defocus or changes in accommodation may lead to slowed myopia progression.5,11
Whatever the mechanism, a rapidly accumulating body of research supports the use of ortho-k for myopia control. This research, along with the obvious benefits of needing to wear contact lenses only overnight, often convinces patients and parents to consider this modality.
The scientific background supporting ortho-k as a valid contact lens option has never been stronger. Toric ortho-k is effective for myopia control,12,13 as is even partial treatment of myopia in patients who have high myopia.14 Ortho-k in combination with low-dose atropine may be even more effective at controlling myopia compared to ortho-k alone.15 Remember, however, that using ortho-k for myopia control is considered off-label, and this information should be conveyed to patients and parents before beginning treatment.
Toric Peripheries Help Center and Improve an Ortho-k Fit
This case is an example of successful use of toric peripheries to center and improve an ortho-k contact lens fit. A 35-year-old woman who had entering refractions of –1.00 –0.50 x 014 OD and –1.25 –0.50 x 177 OS reported discomfort with various brands of spherical soft contact lenses. She had difficulty handling and removing the lenses and experienced awareness of lens movement, lens decentration during wear, and mild dryness, particularly during outdoor sports and activities.
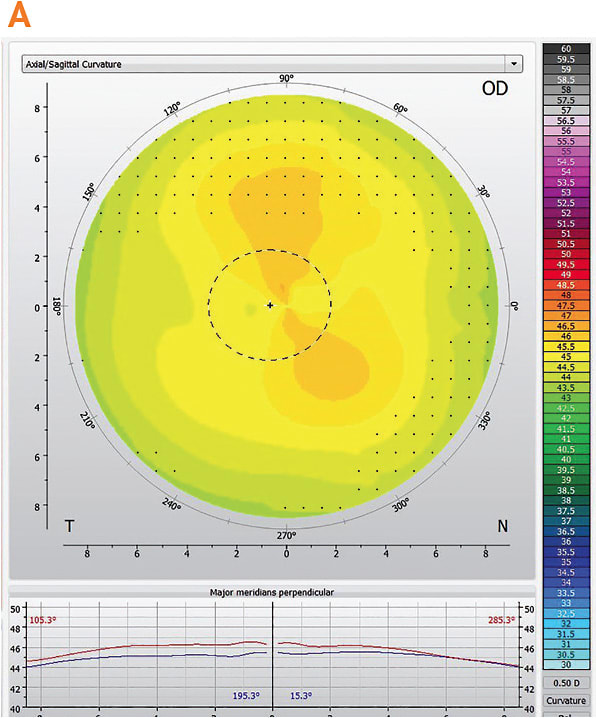
After I ruled out coexisting conditions, such as giant papillary conjunctivitis and ocular surface disease, we decided to try orthokeratology. Figure 1 shows the pretreatment topography for the right eye.
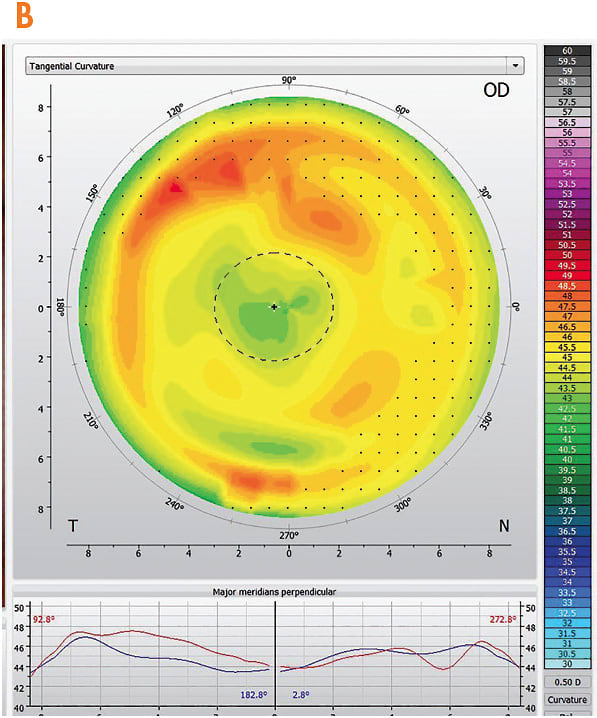
Considering the low refractive cylinder, I chose an initial lens with spherical base curves and peripheries. After a few nights of wear and adaptation, the patient reported excellent comfort, but her vision was still mildly blurred OD and OS. After about two weeks of wear, these symptoms did not improve. The topographies demonstrated mild lens decentration; the ring of midperipheral corneal steepening was not well established (Figure 2).
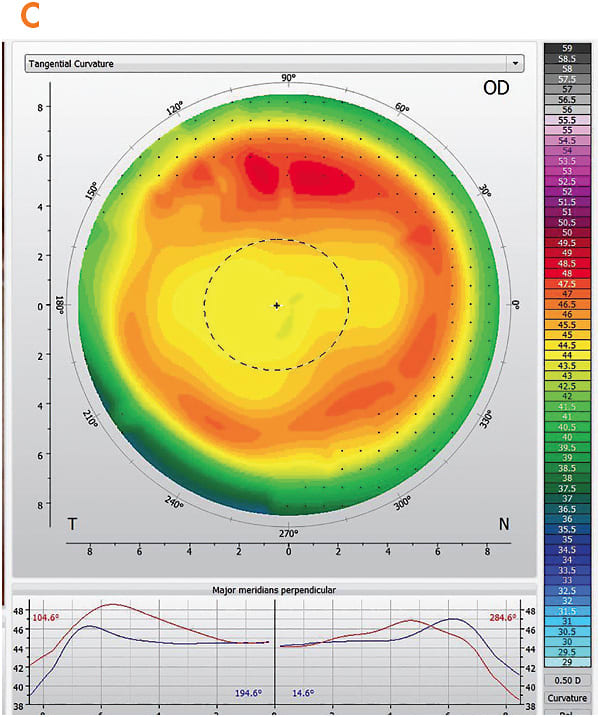
Reviewing the patient’s initial topographies, I noted that, although the corneal cylinder was mild, the toricity extended nearly limbus-to-limbus. I prescribed an adjusted ortho-k lens with toric peripheries.
After only a few days of lens wear, the patient reported that her vision was much improved. The tangential map of this follow-up examination (Figure 3) showed better centration and a more established treatment zone and midperipheral ring.
This same process was completed for the patient’s left eye. She was happy with both lenses after three months of wear.
ADDRESSING MODERN LIFESTYLE CHALLENGES
Compared with just a decade ago, contact lens wearers today present new challenges. Increased use of computers and digital devices has worsened dry eye and asthenopia symptoms, and the more frenzied, active lifestyles of many contact lens wearers have left little room for compromises in vision or comfort during daytime lens wear. Rather than abandoning contact lens wear, symptomatic patients can consider ortho-k to address these issues. Improvements in subjective symptoms (using dry eye questionnaires) and objective signs of dryness (via measurements of conjunctival goblet cell density, redness, and staining) can occur with ortho-k.16,17 Not having to worry about ocular irritations stemming from allergies, dryness, foreign body sensation during daily lens wear, or lost or torn lenses—and more—can be appealing to patients.
Many parents prefer managing their children’s contact lens wear at home, thus avoiding worry about issues that might arise while a child is at school or engaged in other activities. It’s not unusual for a child today to be busy every night of the week with athletics or extracurricular activities, and wearing soft contact lenses for extended hours every day can be deleterious to ocular health and comfort. With ortho-k, lenses are worn and cared for in a controlled environment. While occasional lens breakage or loss does occur, with modern laboratory and shipping efficiencies, replacement lenses can be ordered and received easily and quickly, often before patients notice significant regression.
RESEARCH REVEALS NEW OPPORTUNITIES
Despite numerous improvements in technology and extensive data on the benefits of overnight ortho-k, Morgan and colleagues report only “niche” interest and slight/low levels of growth internationally.18 To achieve future growth in this modality, patients and practitioners need to become more familiar with—and more comfortable trying—ortho-k.
Further research into the biomechanics of corneal molding may reveal new opportunities to apply and improve ortho-k treatment. Lam and colleagues recently found that certain corneal properties, such as corneal hysteresis and stiffness, may be used to proactively identify how successful a patient will be with ortho-k.19 Utilizing machine-learned algorithms that consider numerous additional fitting parameters—such as corneal eccentricity, topographical elevation, anterior chamber depth, and more—are likely superior to traditional refractive and keratometric datasets in choosing the best fitting parameters.20 Reducing the uncertainty of success through more accurate first-lens choices will, without a doubt, encourage more practitioners to attempt corneal reshaping.
In a novel study by Liao and colleagues, corneal cross-linking slowed the regression of ortho-k on rhesus monkey corneas, although the effect was not permanent.21 In humans, ortho-k may show promise in permanently reshaping a myopic cornea or in halting or even reversing keratoconus progression.22 If it were possible to wear ortho-k lenses on a more limited basis (such as one night per month) or to treat irregular astigmatism by combining it with cross-linking, it is highly likely that patients and practitioners would be even more interested in pursuing ortho-k.
FROM FRINGE TO MAINSTREAM
As interest in ortho-k and myopia control grows, so will industry support and organizational contributions. Educational opportunities in ortho-k are abundant; it is already the basis for conferences and symposiums, webinars, continuing education courses, and more. Ortho-k is no longer a fringe interest of a few clinicians. It is a research-based treatment for refractive error and myopia progression that deserves a spot in every ophthalmic curriculum and in most primary eyecare offices.
While the ortho-k lenses of today share many similarities with their predecessors, modern corneal reshaping is easier, faster, and more predictable than it ever was before. Practitioners have easy and convenient access to training, research, and marketing materials for this modality. As technology continues to improve, future evolution in ortho-k likely will provide opportunities for even more patients to enjoy better unaided daytime vision without surgical intervention. CLS
REFERENCES
- Swarbrick HA. Orthokeratology review and update. Clin Exp Optom. 2006 May;89:124-143.
- Coon LJ. Orthokeratology: part I historical perspective. J Am Optom Assoc. 1982 Mar;53:187-195.
- Lui WO, Edwards MH, Cho P. Contact lenses in myopia reduction – from orthofocus to accelerated orthokeratology. Cont Lens Anterior Eye. 2000;23(3):68-76.
- Kerns RL. Research in orthokeratology. Part I: Introduction and background. J Am Optom Assoc. 1976 Aug;47:1047-1051.
- Nti AN, Berntsen DA. Optical changes and visual performance with orthokeratology. Clin Exp Optom. 2020 Jan;103:44-54.
- Charm J. Orthokeratology: clinical utility and patient perspectives. Clin Optom (Auckl). 2017 Feb 7;9:33-40.
- Food and Drug Administration. Summary of safety and effectiveness data of paragon CRT. http://www.accessdata.fda.gov/cdrh_docs/pdf/P870024S043b.pdf . Accessed August 26, 2020.
- Gifford P, Swarbrick HA. Refractive changes from hyperopic orthokeratology monovision in presbyopes. Optom Vis Sci. 2013 Apr;90:306-313.
- Park YM, Park YK, Lee JE, Lee JS. Effect of orthokeratology in patients with myopic regression after refractive surgery. Cont Lens Anterior Eye. 2016 Apr;39:167-171.
- Walline JJ, Lindsley KB, Vedula SS, et al. Interventions to slow progression of myopia in children. Cochrane Database Syst Rev. 2020 Jan 13;1:CD004916.
- Lipson MJ, Brooks MM, Koffler BH. The Role of Orthokeratology in Myopia Control: A Review. Eye Contact Lens. 2018 Jul;44:224-230.
- Chen CC, Cheung SW, Cho P. Toric orthokeratology for highly astigmatic children. Optom Vis Sci. 2012 Jun;89:849-855.
- Zhang Y, Chen YG. Comparison of myopia control between toric and spherical periphery design orthokeratology in myopic children with moderate-to-high corneal astigmatism. Int J Ophthalmol. 2018 Apr 18;11:650-655.
- Charm J, Cho P. High myopia-partial reduction ortho-k: a 2-year randomized study. Optom Vis Sci. 2013 Jun; 90:530-539.
- Kinoshita N, Konno Y, Hamada N, Kanda Y, Shimmura-Tomita M, Kakehashi A. Additive effects of orthokeratology and atropine 0.01% ophthalmic solution in slowing axial elongation in children with myopia: first year results. Jpn J Ophthalmol. 2018 Sep;62:544-553.
- Carracedo G, Martin-Gil A, Fonseca B, Pintor J. Effect of overnight orthokeratology on conjunctival goblet cells. Cont Lens Anterior Eye. 2016 Aug;39:266-269.
- Garcia-Porta N, Rico-del-Viejo L, Martin-Gil A, Carracedo G, Pintor J, González-Méijome JM. Differences in Dry Eye Questionnaire Symptoms in Two Different Modalities of Contact Lens Wear: Silicone-Hydrogel in Daily Wear Basis and Overnight Orthokeratology. Biomed Res Int. 2016;2016:1242845. Epub 2016 Aug 31.
- Morgan PB, Efron N, Woods CA, Santodomingo-Rubido J; International Contact Lens Prescribing Survey Consortium. International survey of orthokeratology contact lens fitting. Cont Lens Anterior Eye. 2019 Aug;42:450-454.
- Lam AKC, Hon Y, Leung SYY, Shu-Ho L, Chong J, Lam DCC. Association between long-term orthokeratology responses and corneal biomechanics. Sci Rep. 2019 Aug 29;9:12566.
- Fan Y, Yu Z, Peng Z, et al. Machine learning based strategy surpasses the traditional method for selecting the first trial lens parameters for corneal refractive therapy in Chinese adolescents with myopia. Cont Lens Anterior Eye. 2020 May 14;S1367-0484(20)30097-7.
- Liao C, Lin X, Keel S, Ha J, Yang X, He M. Effects of corneal crosslinking on corneal shape stabilization after orthokeratology. Sci Rep. 2020 Feb 11;10:2357.
- El Hage S, Seiler T. Corneal cross-linking and orthokeratology. Contact Lens Spectrum. 2011 Dec;26.




