Modern corneal topography has greatly advanced our understanding of the shape, power, and profile of the corneal surface to improve the design and prescribing of contact lenses. However, a unique and innovative use of the corneal topographer is imaging over soft multifocal contact lenses to better appreciate where the optics of the contact lens are in relation to key anatomical features.
Multifocal Optics: Location, Location, Location
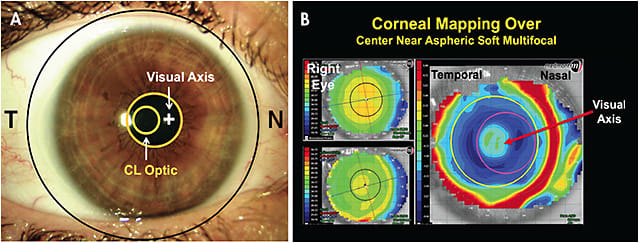
To do this, first capture an image of a patient’s eye without a contact lens as a baseline. Then, perform topography while the patient is wearing a soft multifocal lens. Use a subtractive/difference display map to compare the baseline topography to the image captured over the soft multifocal lens. This technique is possible because the multifocal optics are on the front lens surface.
The most useful map for this technique is the tangential display, as it provides a sensitive interpretation of position. When patients look at the fixation target in the instrument, the map is centered on their visual axis. The warmer colors on the difference map are steeper curves, in this case highlighting the more relative plus powers (i.e., the add within the lens), and the cooler colors highlight the flatter or more minus powers (i.e., the distance correction within the lens).
This technique is helpful in understanding the position of the multifocal optics in relation to a patient’s visual axis and over his or her pupil. Figure 1 shows a center-near aspheric soft multifocal lens on a right eye. The visual axis is at the center of the map, and the add power is temporal to this because the lens is decentered temporally. Temporal decentration is common because the nasal sclera is flatter and higher compared to the relatively steeper and lower temporal sclera (Ritzmann et al, 2017).
How does this affect the performance of multifocal optics? Zheng et al (2016) compared center-distance multifocal lenses that had geometrically centered optics to center-distance multifocals that had the optics offset (0.5mm and 1.0mm nasally). They concluded: “Snellen acuity and subjective vision were decreased with increasing temporal decentration from the visual axis.”
Ramdass et al (2018) fit 20 presbyopic individuals with standard geometrically centered aspheric center-near soft multifocals and then switched them to 1mm nasal offset center-near multifocal soft lenses. They concluded: “1 mm nasal offset optics provided a statically and clinically significant difference for subjective performance and preference when viewing various types of near targets.” Additionally, though the subjects were blinded to the lens type worn, 19 of the 20 preferred the offset near optics at the completion of the study.
When troubleshooting underperforming soft multifocal contact lenses, this technique can help practitioners better appreciate what patients are experiencing and what modifications would better respect patients’ visual axis and pupil. CLS
For references, please visit www.clspectrum.com/references and click on document #298.




