Practitioners use diagnostic lens fitting sets to design most scleral lenses. We adopted this process early on, because none of our instrumentation could measure enough of the anterior ocular surface to translate to scleral lens design. For fitting purposes, practitioners often use scleral diagnostic lenses to determine primary parameters including the lens sagittal depth, which allows for corneal clearance, and the characteristics of the landing zone.
Modern manufacturing allows landing zone designs to be spherical, toric, quadrant-specific, or fully custom. Although the increased complexity of landing zone designs can improve the fit of a scleral lens, recognizing the type and amount of change necessary to properly fit the landing zone can be a challenge. There is a relatively steep learning curve for novice practitioners to master the art of translating a diagnostic lens fitting to a successful scleral lens design. Macedo-de-Araújo and colleagues found that when using diagnostic lenses, it took up to 60 scleral lens fits to reduce the number of trial lenses and reorders necessary to achieve success.1 To put that into perspective, it could take two years for a practitioner who averages only a few scleral lens cases per month to become a proficient scleral lens fitter.
This article reviews advances in technology and research that have increased our collective knowledge of scleral shape and how we can apply that knowledge to improve scleral lens fitting efficiency and success.
ASYMMETRY AND LANDING ZONES
Scleral lens diagnostic sets and designs in the early 2000s typically employed spherical landing zones. A series of papers by Visser and colleagues in 2006 and 2007 started a shift in the industry toward toric landing zones.2,3 These studies demonstrated that patients preferred scleral lenses designed with toric landing zones compared to those with spherical landing zones. The theory was that the lenses with the toric landing zones had a more evenly balanced weight distribution on the ocular surface. Patients wearing scleral lenses with toric landing zones reported improved comfort, vision quality, and overall satisfaction compared with scleral lenses that had spherical landing zones. These studies highlighted, through lens design, that scleral shape is not spherical.
In 2010, van der Worp et al reported the first published data about scleral shape that was measured using optical coherence tomography.4,5 Perhaps the most important finding from this study was that the typical eye is non-rotationally symmetrical, a term that does not include spherical or toric shapes, only shapes without rotational symmetry.
Van der Worp and colleagues also found that typical scleral shape increases in asymmetry moving away from the limbus toward the periphery. The nasal quadrant is generally flattest, and the profile change of the sclera is tangential. These findings had an enormous influence on scleral lens fitting and design. In fact, they help explain the findings from the Visser papers, because even though the sclera is not necessarily toric, a toric landing zone will more evenly bear on an asymmetric surface than a spherical landing zone would.
KEY DATA FROM CORNEOSCLERAL TOPOGRAPHY
Many specialty lens clinics have Placido-based corneal topographers; however, these instruments cannot reflect light off of—or out onto—the bulbar conjunctival scleral surface. The recent advent of corneoscleral topography has dramatically increased our understanding of scleral shape and how that can be applied directly to scleral lens fitting.
Corneoscleral topographers can measure the entire anterior ocular surface out to 22mm in diameter. When fluorescein is applied to the ocular surface, the instrument recognizes both the clear tissue of the cornea and the bulbar conjunctiva. It creates a three-dimensional model of the eye that can be used for measurement and for lens design.
Sagittal height can be measured at a single location or as a mean for a given chord diameter. Keep in mind that sagittal height is measured from a plane that runs tangential to the center of the ocular surface. Therefore, sagittal height increases in areas of the sclera that are steeper in curvature and decreases where the sclera is flatter.
Sagittal height maps can show sagittal height changes on the eye. The ocular surface is compared to a reference sphere, generating a scleral elevation map in which on the sclera, cooler colors represent relative increases in sagittal height or steepening compared to the reference sphere, and warmer colors represent decreases in sagittal height or flattening.
These data can help determine not only the landing zone design but also the exact micron differences needed between meridians for nonspherical designs, such as toric or quadrant-specific landing zones. In addition, these instruments have virtual automated processing software that uses the measured data to determine parameters of some branded lens designs.
PLOTTING CHARACTERISTIC PATTERNS
A quantitative method for assessing scleral shape is to evaluate circumferential sagittal height at specified chord diameters. The sagittal height is plotted on the Y axis versus position in degrees on the X axis. These plotted data show characteristic patterns that can help identify scleral shape. For example, a toric scleral shape results in a sinusoidal pattern that is symmetric and has a periodicity of 180º (Figure 1). If the scleral shape were spherical, then the plotted line would be straight, because the sagittal height wouldn’t change circumferentially at the selected chord diameter.

In 2017, the Scleral Shape Study Group (SSSG) categorized scleral shape using scleral shape plots at a chord diameter of 16mm.6 Investigators retrospectively analyzed 140 eyes of prospective scleral lens patients. The threshold sagittal height that was used to differentiate the patterns was 300 microns. Four groups were identified, and the percentage of scleral shapes with pattern descriptions were as follows: 5.7% spherical, 28.6% toric-regular, 40.7% asymmetric, and 25% periodicity different from 180º. Matching these values with scleral lens landing zone designs suggests that the eyes would be best fitted as follows: 5.7% with a spherical landing zone, 28.6% with a toric landing zone, and 65.7% with a quadrant-specific or custom design. Changing the sagittal height difference threshold value to 150 microns results in the following: 0.7% spherical, 18.6% toric-regular, 55.7% asymmetric, and 25% periodicity different from 180º. As the threshold difference decreases, the asymmetric cases increase.
INFLUENCE OF CORNEAL ECTASIA
In 2019, the SSSG explored a potential relationship between corneal ectasia and scleral shape.7 Investigators evaluated 227 eyes that had ectasia and 115 normal eyes. The ectatic eyes were categorized as having either central or peripheral ectasia. Central ectasia was defined as a corneal apex within 1.25mm of the center of the cornea; apexes outside of this zone were considered peripheral ectasias.
Investigators measured and evaluated two features of each eye. The first was microns of scleral toricity over a 16mm chord diameter. The second was a measurement of asymmetry or what was termed a quadrant-specific effect. The results showed that all eye types had significant amounts of mean symmetric scleral toricity with the following values: normal cornea, 172 microns; central ectasia, 210 microns; and peripheral ectasia, 220 microns. However, there were significant differences among normal corneas, corneas that had central ectasia, and corneas that had peripheral ectasia in terms of quadrant-specific effects, with the following mean values: normal corneas, 17 microns; central ectasias, 66 microns; and peripheral ectasias, 289 microns. For the eyes that measured a quadrant-specific effect, the sclera had relatively greater sagittal height or steepness in the same axis as the peripheral corneal ectasia. These results imply an interconnectedness between the cornea and the sclera for eyes that have peripheral ectasia.
When considering lens design, eyes that exhibit central ectasia have scleral shapes that are similar to normal eyes and would, on average, be best fitted with a scleral lens that has a toric landing zone. Eyes that have peripheral ectasia would, on average, require a scleral lens with a more customized landing zone design, such as a quadrant-specific or a free-form design. In a case of inferior peripheral ectasia, the inferior sclera will be steeper, which can cause inferior decentration of a non-customized scleral lens; think of the scleral lens as sliding downhill. Selectively steepening the inferior quadrant of the landing zone to match the patient’s scleral shape often will improve centration of the scleral lens.
POTENTIAL LINK BETWEEN CORNEAL AND SCLERAL SHAPE
Some researchers have investigated a potential relationship between the corneal and the scleral shape. A link between these two distinct tissues could potentially help practitioners predict the scleral shape by assessing the cornea. While several small studies failed to show any such predictable relationship,8-10 studies by Macedo-de-Araújo et al and by Consejo and Rozema did find a relationship between corneal astigmatism and scleral toricity in patients who had normal corneas.11,12
One key difference between the Consejo/Rozema study and other reports is that they used measurements from corneoscleral topography that included data from the paralimbal cornea. It is likely that when astigmatism is confined to the central and paracentral regions of the cornea, there isn’t a match in scleral shape, but corneal limbal astigmatic changes would extend out onto the scleral surface. There are clinical exceptions to this phenomenon.13
The Consejo/Rozema paper suggests that astigmatism is not limited to the cornea but should be considered a property of the eye globe. The SSSG determined that an interconnective relationship exists between corneal ectasia and scleral shape. In the case of ectasia, several questions arise. Is the cornea affecting the scleral shape, or is the scleral shape affecting the cornea? Why are most of the apexes in corneal ectasia located in the inferior quadrant?7 Does a steeper sclera (increased sagittal height) in the inferior quadrant cause the corneal apex to position inferiorly? Or does an inferior cone cause a steeper sclera in the same axis? Some evidence suggests that the cornea influences the sclera, as some clinicians have reported changes in scleral shape after corneal cross-linking.14,15
USING SCLERAL SHAPE DATA FOR SUCCESSFUL FITTING
The following cases demonstrate how scleral shape measurement and assessment led to successful scleral lens design.
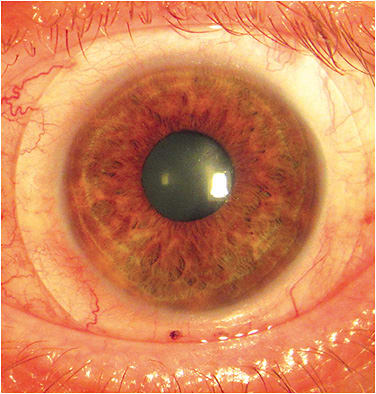
Post-RK Corneal Irregularities and Residual Refractive Error A 58-year-old woman reported for scleral lens fitting of her left eye. Previous radial keratotomy (RK) surgery had left her with residual refractive error, corneal irregularity, and diurnal visual fluctuation. Her left eye refraction was +4.50 –1.50 x 050. She was previously unsuccessful with soft contact lenses. Other than uncomplicated RK incisions, slit lamp examination was unremarkable.
Corneoscleral topography confirmed corneal irregularity, and the scleral elevation map (Figure 2) revealed 302 microns of symmetric scleral toricity. A 16mm diagnostic scleral lens with a spherical landing zone was placed on the eye for over-refraction. This lens showed edge lift (Figure 3) as expected, as it needs selective steepening horizontally to align with the temporal and nasal quadrants.


A 16mm scleral lens that incorporated a customized toric landing zone was designed and manufactured. This lens cleared the cornea, had an alignment landing zone fit, and was comfortable for the patient to wear. It provided 20/20 visual acuity, and the patient experienced no diurnal vision changes when wearing the scleral lens. This is important, as she was previously wearing different pairs of eyeglasses during the day to attain best vision. For this case, measuring the entire anterior ocular surface enabled me to efficiently design a customized toric landing zone, which gave the patient immediate success without complications.
Scleral Asymmetry and Nasal Pinguecula A 56-year-old man who had keratoconus reported for scleral lens evaluation of his left eye. He had been wearing soft contact lenses and desired improved visual acuity. Manifest refraction of the left eye was –2.50 –2.00 x 093, 20/30. Corneal topography confirmed the diagnosis of keratoconus. Slit lamp examination was remarkable for a nasal pinguecula. Corneoscleral topography revealed that the scleral shape had clinically significant irregularity of 200-micron circumferential fluctuations. Using a quantitative sagittal height plot, I determined that the nasal pinguecula had an elevation of 235 microns.
Because the pinguecula had a sagittal height that was greater than the 200-micron threshold of clinical significance, I decided to use software to design a free-form lens that would ensure even alignment of the landing zone (Figure 4). At the dispensing visit, the scleral lens fit well and was comfortable for the patient to wear (Figure 5). With a minimal over-refraction, the patient’s visual acuity was 20/20.

For this case, the combination of scleral asymmetry and nasal pinguecula required a custom design for a perfect match of the landing zone with the anterior ocular surface. Using a lens design that had a preset spherical or toric landing zone would not have matched the surface shape, leading to potential fitting complications.
Not accounting for pingueculas will increase the likelihood of failure. In my experience, pingueculas that have elevations of 200 microns or more within the zone of a scleral lens will cause impingement that leads to proximal edge lift, decentration, and irritation. For this eye, the lens is designed to exactly match the bulbar conjunctiva-scleral surface, including a localized vault that clears the surface of the patient’s pinguecula. Matching the landing zone to the ocular surface rotationally stabilizes the lens to keep the localized vault in position.
Custom Design for Disciform Scar A 47-year-old man reported for scleral lens fitting. He had a history of a disciform scar of his left eye secondary to a herpes simplex infection. His left eye’s uncorrected visual acuity measured 20/70. Corneoscleral topography was performed, and the corneal elevation map showed severe corneal irregularity with a depression that corresponds to the scarring (Figure 6), as confirmed by slit lamp examination. The scleral elevation map indicates scleral asymmetry.

To quantitate scleral shape, we can look at the sagittal height profile of the ocular surface at a chord diameter of 16mm (Figure 7). The plotted sagittal height is significantly asymmetric, which indicates that a toric or spherical landing zone will not provide a satisfactory fitting relationship. I determined that this patient would be best fitted with a customized landing zone that would match the bulbar conjunctival-scleral surface.

A customized free-form scleral lens was ordered, manufactured, and dispensed. The lens exhibited landing zone alignment without compression, blanching, or impingement (Figure 8). The lens is marked with two inferior black dots to indicate to the patient its position for proper on-eye application. The asymmetry of the landing zone rotationally stabilizes the lens during wear. The patient’s resulting visual acuity was 20/20, and he was satisfied with the result.

Attempting to determine a final lens design for this patient using diagnostic lenses, either with a spherical or a toric landing zone, would have been much more challenging. We can hypothesize that multiple remakes may have been required to achieve the customization necessary for a successful fit.
INCREASE SUCCESS WITH CUSTOMIZATION
The fact that scleral lenses rest on the spongy bulbar conjunctiva rather than on the firm surface of the sclera allows a certain amount of forgiveness with lens design. This is probably what allowed scleral lenses to start growing in popularity before we had the ability to measure and understand bulbar conjunctiva-scleral surface shape. That said, fitting complications often result from a mismatch between the scleral lens landing zone and the ocular surface. Misalignment of the landing zone can result in lens impingement, edge lift, decentration, and flexure.16,17
We now know that most eyes that need scleral lenses have significant amounts of scleral asymmetry. This means that practitioners should be designing more customized lenses to achieve the best fit. This is particularly true for many patients who have corneal ectasias. By taking advantage of instruments that provide profilometry, practitioners will understand the shape of the eyes that they are fitting and thus will be able to efficiently design customized scleral lenses that will have the highest rates of success. It is likely that scleral lenses fitted five years from now will be designed mostly from profilometry, and practitioners will someday wonder how we were ever able to successfully fit patients using diagnostic lenses alone. CLS
REFERENCES
- Macedo-de-Araújo RJ, van der Worp E, González-Méijome JM. Practitioner Learning Curve in Fitting Scleral Lenses in Irregular and Regular Corneas Using a Fitting Trial. Biomed Res Int. 2019 Jan 28;2019:5737124.
- Visser ES, Visser R, van Lier HJJ. Advantages of toric scleral lenses. Optom Vis Sci. 2006 Apr;83:233-236.
- Visser ES, Visser R, van Lier HJJ, Otten HM. Modern scleral lenses part II: patient satisfaction. Eye Contact Lens. 2007 Jan;33:21-25.
- van der Worp E, Graf T, Caroline P. Exploring Beyond the Corneal Borders. Contact Lens Spectrum. 2010 Jun;26-32.
- van der Worp E, Bornman D, Lopes Ferreira D, Faria-Ribeiro M, Garcia-Porta N, González-Meijome JM. Modern scleral contact lenses: A review. Cont Lens Anterior Eye. 2014 Aug;37:240-250.
- DeNaeyer G, Sanders DR, van der Worp E, Jedlicka J, Michaud L, Morrison S. Qualitative Assessment of Scleral Shape Patterns Using a New Wide Field Ocular Surface Elevation Topographer: The SSSG Study. J Cont Lens Res Sci. 2017 Nov;1:12-22.
- DeNaeyer G, Sanders DR, Michaud L, et al. Correlation of Corneal and Scleral Topography in Cases with Ectasias and Normal Corneas: The SSSG Study. J Cont Lens Res Sci. 2019 Apr;3:e10-e20.
- Kinoshita B, Morrison S, Caroline P, Kojima R, Lampa M. Corneal Toricity and Scleral Asymmetry…Are They Related? Poster presented at the Global Specialty Lens Symposium; January 2016; Las Vegas.
- Siebert S, Jedlicka J. Utilizing Corneal Topography to Aid in Predicting Scleral Topography for the Purpose of Fitting Scleral Contact Lenses. Poster presented at the Global Specialty Lens Symposium; January 2017; Las Vegas.
- Lopez-Alcon D, Castejon I. Relationship Between the Stabilization Axis of a Scleral Lens with Toric Peripherals and the Axis of Corneal Astigmatism. Poster presented at the Global Specialty Lens Symposium; January 2018; Las Vegas.
- Macedo-de-Araújo RJ, Amorim-de-Sousa A, Queirós A, van der Worp E, González-Méijome JM. Relationship of Placido corneal topography data with scleral lens fitting parameters. Cont Lens Anterior Eye. 2019 Feb;42:20-27.
- Consejo A, Rozema JJ. Scleral Shape and Its Correlations With Corneal Astigmatism. Cornea. 2018 Aug;37:1047-1052.
- DeNaeyer G. Corneal and Scleral Toricity. Contact Lens Spectrum. 2020 May;35:52.
- DeNaeyer G, Sanders D. Collagen Crosslinking for Keratoconus Can Change Scleral Shape. J Cont Lens Res Sci. 2018 Mar;2:e15-e21.
- Visser ES, Soeters N, Tahzib NG. Scleral lens tolerance after corneal cross-linking for keratoconus. Optom Vis Sci. 2015 Mar;92:318-323.
- Fadel D. Scleral Lens Issues and Complications Related to a Non-Optimal Fitting Relationship Between the Lens and Ocular Surface. Eye Contact Lens. 2019 May;45:152-163.
- Vincent SJ, Kowalski LP, Alonso-Caneiro D, Kricancic H, Collins MJ. The influence of centre thickness on miniscleral lens flexure. Cont Lens Anterior Eye. 2019 Feb;42:63-69.




