The 2021 Global Specialty Lens Symposium (GSLS), presented by Contact Lens Spectrum, was a virtual event held from Jan. 21 to 23 that drew a larger and more global audience than ever seen in the conference’s history (Figure 1): more than 4,000 total registrants from 83 countries, with 2,883 live attendees. In addition, more than 30 companies were sponsors or exhibitors.

The Education Committee of Jason J. Nichols, OD, MPH, PhD (chair); Edward S. Bennett, OD, MSEd; Patrick Caroline; Karen DeLoss, OD; Lynette Johns, OD; and Eef van der Worp, BOptom, PhD, presented a program covering all aspects of specialty contact lenses, with an emphasis on scleral lenses, myopia management, keratoconus, diagnostic technologies, and practice management. Along with the general and breakout sessions were three workshops, free papers, a record number of posters, and even trivia contests presented by May Eye Interrupt hosts Craig Norman and Jason Jedlicka, OD, who gave away prizes for the correct answers to trivia questions about the GSLS sponsors.
This article presents some of the many highlights from the continuing education sessions of this year’s GSLS. All of the virtual sessions are available to view through April 30, 2021 with free registration at https://gsls2021.myconexsys.com/ ; in addition, the CE courses of the program will be housed after April 30 at https://clspectrumce.com .
WORKSHOPS
Three workshops kicked off the educational offerings of the 2021 Virtual GSLS: Orthokeratology, Scleral Lenses, and Irregular Cornea Contact Lens Case Grand Rounds.
Orthokeratology During the two-part orthokeratology (ortho-k) workshop, Patrick Caroline discussed three different ortho-k fitting methods: inventory, empirical, and topography fitting techniques. The goal of the workshop was to take attendees step-by-step through how each of these fitting techniques is used in pediatric clinical practice.
Maria Liu, OD, PhD, MPH, MBA, then showed videos of ortho-k fittings of three different children, each of whom was fit with one of the three fitting techniques. One pearl that she shared is that different techniques to obtain K readings will provide different results; she prefers to use auto K readings from the autorefractor. In addition, horizontal visible iris diameter (HVID) measurements and white-to-white (WTW) measurements are often different, so ask the lab which to use. She also recommends taking baseline axial length measurements and cycloplegic refraction before starting ortho-k; the axial length measurements can be repeated annually unless there are signs of progression, in which case they should be taken at least semi-annually.
Once the ortho-k lenses are on-eye, Dr. Liu gets patients out of the exam room, offering games and other activities to distract from the initial feeling of the lens. She recommended studying the family dynamics to determine whether application and removal training should be directed at the patients or the parents. After lens application at home, patients should do the “2C check” for clarity and comfort, both of which should be good before sleeping in the lenses.
After the first night of wear, patients should return to the office wearing the lenses. Before lens removal, perform autorefraction, visual acuity measurement, and fluorescein evaluation. Dr. Liu cautioned that the autorefractor can overestimate the amount of undercorrection. She also explained how to evaluate and troubleshoot the topography findings after lens removal.
When fitting with a topography-guided system, Dr. Liu recommended that practitioners work on ways to obtain as large a sampling area as possible. In addition, patients may need to move their mask down so that it is not pushing up the lower lid.
A final pearl was that with ortho-k lenses that have a tangential design, a larger-diameter lens that approaches the limbus is often a better fit compared to using a smaller lens that decenters, because it is the midperipheral cornea rather than the limbus that is bearing the weight of the larger lens.
Scleral Lenses This year’s Scleral Lenses workshop was co-hosted by the Scleral Lens Education Society (SLS); all of the presenters were part of the SLS.
Matt Kauffman, OD, detailed the various images that would be included in the presentations such as cross-sectional optical coherence tomography (OCT), white light optic sections, full white light illumination, and full illumination with fluorescein and cobalt blue light. He noted that the directionality of the light and how diffuse or bright it is play a role when assessing a scleral lens fit. He then discussed indications for scleral lens use, including optical indications for both irregular and regular corneas and to protect the ocular surface for post-surgical patients or for those who have ocular surface disease or dryness.
Maria Walker, OD, reviewed scleral lens terminology based on a report by Michaud et al.1 Next, Dan Fuller, OD, provided an overview of fitting steps. Step 1 is to choose a lens design and diameter. It is also necessary to determine the corneal profile (prolate versus oblate). Using the manufacturers’ fitting guide is a good place to start.
Dr. Walker and Karen Lee, OD, showed a series of videos demonstrating scleral lens application. Rob Ensley, OD, discussed the remaining fitting steps. Step 2 is evaluating apical clearance in the optic zone. It’s important when determining clearance to take settling into account, about 25% of which occurs in the first 20 to 30 minutes, so include that time in your fitting.
Step 3 is evaluating limbal clearance in the transition zone; issues can occur with clearance that is either too high or too low. In Step 4, evaluate scleral landing in the landing zone. Look for conjunctival blanching, which would indicate a too-tight fit. Dr. Ensley noted that impingement differs from compression in that impingement usually occurs at the lens edge.
The final step is to perform an over-refraction, first a spherical and then a sphero-cylindrical over-refraction. Be aware of residual astigmatism. Toric haptics can sometimes help with this.
Dr. Kauffman provided images and videos depicting lens removal. He also reviewed lens care systems and how they should be used.
Drs. Walker and Lee discussed patient follow up. They recommended a two-week follow up for every curvature change, a one-month visit after the fit is finalized, a six-month follow up for first-time scleral wearers, and annual follow up thereafter for all scleral wearers.
In the second session of the workshop, the presenters offered a more advanced look at sclerals. Dr. Kauffman detailed the four primary scleral shapes and instruments that can be used for imaging the sclera. Drs. Ensley and Fuller looked further at the landing zone fit. Drs. Walker and Lee discussed possible staining patterns post-lens removal. They suggest getting baseline data and to treat affected patients as though they have a disease. Dr. Kauffman ended the workshop with a discussion of advancements in optics, including options for presbyopes as well as wavefront-guided sclerals.
Irregular Cornea This workshop was co-hosted by the GP Lens Institute and presented by Edward S. Bennett, OD, MSEd; Elise Kramer, OD; and Stephanie Woo, OD. Preceded by brief discussions of the contact lens options being fit during the workshop, it included both live patients and patients whose lens fit had been previously videotaped. Attendees were able to see the live view through the biomicroscope of the contact lenses fit during the workshop by Dr. Woo in her specialty contact lens practice in Las Vegas.
The first part of the workshop included corneal GP, intralimbal GP, and soft lens options for keratoconus. The type of lens to select depends on the type of cone and the severity of the disease. It was emphasized throughout that laboratory consultants can help optimize success.
Small corneal GP lenses are a viable option with nipple cones, whereas intralimbal (often 10.5mm to 11.5mm in overall diameter) represent an option for nipple and oval cones and for mild-to-moderate cases. A high-Dk (i.e., 50 to 99) lens material is recommended for these lenses. Typically, a “three-point” or feather touch fitting relationship is recommended, although very mild apical clearance is acceptable as well. Use the base curve radius recommended by the manufacturer as a starting point.
The panel presented a case of a 79-year-old post-penetrating keratoplasty patient who had glaucoma and large filtering blebs OD and OS. He had been a long-term corneal GP wearer. He was successfully fitted with a 65-Dk, 10.2mm larger-diameter GP design with a reverse geometry back surface to better align with his oblate corneas. The presenters agreed that, although scleral designs are an option in these cases, large corneal designs typically do not compromise the peripheral cornea and limbus, provide good oxygen transmission, and are not likely to impact intraocular pressure.
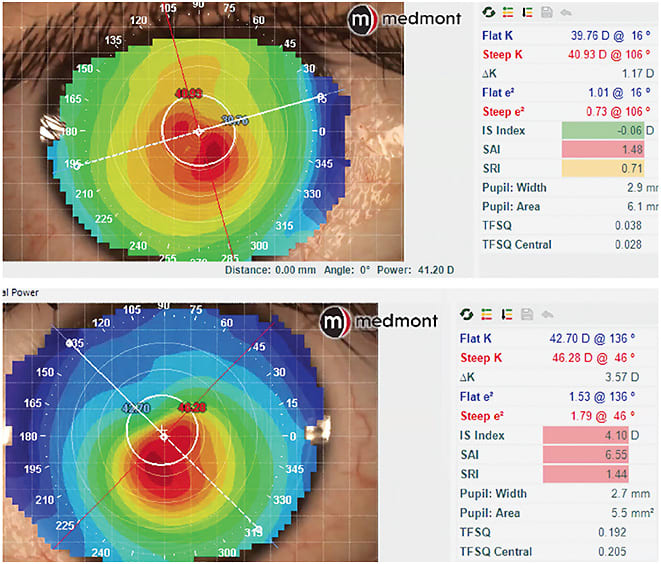
It was emphasized that custom soft and hybrid designs are options that should be in every eyecare professional’s irregular cornea fitting toolbox. Dr. Woo presented a case in which a post-corneal cross-linking (CXL) patient had initially been fit into scleral lenses but discontinued due to dryness. Figure 2 shows her baseline topography. She was successfully refit into a custom soft keratoconus lens design in a silicone-hydrogel material. For mild-to-moderate cases, a reverse geometry vaulted hybrid design is a viable option for patients seeking good initial comfort who may not desire or benefit from scleral lenses.
The second part of this workshop discussed scleral lenses, which have become a go-to option notably in moderate-to-severe irregular cornea cases.2 A diagnostic technology that is helpful in fitting scleral lenses for irregular corneas is profilometry, which provides elevation data for both the cornea and sclera as well as the sagittal height of the eye. If the scleral toricity is high, a custom lens is needed. In one case, an initial lens exhibited a steep fitting pattern (the presenters recommend approximately 200 microns of clearance after one hour of lens wear) as well as excessive edge clearance, which resulted in debris under the lens (Figure 3). It was recommended to reduce both the central vault and the peripheral edge clearance to optimize the fit.

GENERAL SESSIONS
The General Sessions at the 2021 Virtual GSLS covered some of the hottest topics in contact lenses today: contact lens innovations, scleral lenses, myopia management, and keratoconus. The Scleral Lens Supersession moderated by Dr. Johns is covered in a separate feature article in this issue, so here we’ll focus on the other three general sessions.
Contact Lens Innovations The first general session was “Innovations in Contact Lenses: From Beginning to Present Day.” Dr. Nichols kicked it off with a review of the state of the contact lens industry, based on statistics from Contact Lens Spectrum’s Annual Report.3
Next, in honor of the 50-year anniversary of soft contact lenses, Pat Caroline and Craig Norman, co-curators of the Contact Lens Museum, provided a history lesson on soft lenses. They noted that the story of soft contact lenses began with Otto Wichterle and Drahoslav Lim and their discovery of the plastic polyhydroxyethyl methacrylate (pHEMA) in Czechoslovakia during the early 1950s. Much more on the events leading up to this and their subsequent lens manufacturing can be found in the History of Contact Lenses column.
Of note, on Christmas Eve 1961, Otto Wichterle built a machine using his son’s Merkur set (like an Erector set), the generator from his bicycle light, and a bell transformer. On Christmas Day, he produced the first four soft contact lenses at his kitchen table. After submitting a patent application for spin-casting soft lenses, in 1962, he developed a basic carousel machine for “mass” production. That same year saw the first commercially available lenses, called SPOFA lenses. Another huge innovation happened in 1963, when Dr. Wichterle recreated his hydrogel plastic in a dehydrated state called Xerogel, which basically makes up the buttons that are used in many custom soft lenses today. In honor of Dr. Wichterle’s contributions to the history of contact lenses, he was awarded this year’s GSLS Award of Excellence
Award of Excellence
This year’s annual Award of Excellence was presented posthumously to Otto Wichterle, a Czech chemist who is best known for his invention of modern soft contact lenses. The Education Planning Committee chose this year’s recipient as a nod to the 50-year anniversary of the soft contact lens. In lieu of a physical award, a donation was made by the GSLS in Otto Wichterle’s name to the Contact Lens Museum.


Next, Dr. van der Worp discussed how we fit soft contact lenses today, stating that to be more successful, we need to move beyond base curve. He noted that keratometry is a thing of the past. Instead, a standard ocular sagittal height (OC-SAG) at a chord of 15mm is 3,750 microns. The OC-SAG range between the flattest and steepest eye is about 900 microns. He shared recent research that evaluated the sag heights of various standard daily disposable lenses.4 With this data, if one lens doesn’t fit, we now have more information about which lens to try next. The research also shows information for reusable lenses and compares spherical versus toric for both daily disposable and reusable lenses. He noted that microns of height is the new millimeters of radius.
The final section of the session featured Dr. Johns’ look at correcting higher-order aberrations (HOAs) with scleral lenses. Aberrations can be measured via a Hartmann-Shack aberrometer, a Scheimpflug rotating camera, or a dual-camera aberrometer. Practitioners can use dynamic sciascopy, which Dr. Johns described as fancy automated retinoscopy. Lastly, practitioners can use a laser ray tracing method.
Dr. Johns noted that wavefront-guided lenses are being beta tested. To create a wavefront-guided lens, you must optimize low-order correction, use a test lens with registration marks, use software to measure decentration and rotation of optics, have lens stability, and have a manufacturer capable of submicron lathing to handle your correction. Dr. Johns mentioned that limitations to wavefront-guided lenses include cost, changes in pathology, media opacities, pupil size and custom zone relationship, care and handling, and neural adaptation.
Myopia Management Dr. van der Worp moderated the session “Customizing the Treatment of the Myopic Child,” which included a very contemporary look at all current options, their effectiveness, and bottom-line recommendations on how and when to implement these options, either solely or in combination.
It is evident that the incidence and severity of myopia continue to increase. In fact, there is good evidence that the effect has increased greatly just in the past year. A recent study with well over 100,000 children reported that a large myopic shift of –0.30D was observed in 2020 school screenings as compared to previous years (2015 to 2019) for 6- to 8-year-old children.5 An increase in near tasks (including smartphone use) accompanied by less time outdoors, especially during the pandemic, can likely explain these results. The ocular health consequences of high myopia—notably later in life—make it imperative to incorporate a myopia management strategy in clinical practice today. Every 1.00D reduction in myopia decreases the risk of myopic maculopathy by 40%.6
Kate Gifford, BAppSc(Optom)Hons, PhD, analyzed the literature and found that ortho-k is the modality with the longest track record of high (approximately 50%) effectiveness, and it has a more robust amount of supportive evidence. The effect of ortho-k can be enhanced by optimizing the lens design. Notably, a recent study reported that ortho-k lenses with a > 5mm treatment zone diameter (TZD) resulted in twice the increase in axial length (i.e., 0.16mm/year versus 0.08mm/year) when compared to lenses with a TZD ≤ 5mm.7 This becomes especially important when you factor in pupil size. Langis Michaud, MSc, reported on research from his university that treatment zone diameter can significantly influence choroidal thickness (i.e., large treatment zones result in reduced choroidal volume and, therefore, longer eyes).
High-order aberrations, particularly spherical aberration, may serve as a possible mechanism to slow axial elongation in myopia treatment.8 Spherical aberration is notably increased as the TZD decreases and the pupil size increases.
Peripheral-plus-power soft lenses introduce positive myopic defocus to the retinal image and overall have an efficacy that tends to range from 30% to 50%. As with ortho-k, most lens designs introduce increased levels of positive spherical aberration. Other factors that impact efficacy and success include pupil size and lens centration. In addition, as accommodation introduces negative spherical aberration, which would reduce the amount of peripheral myopic defocus, children doing more near work would need a modality with increased myopic defocus. One such option may be to simply increase the add power.9 However, it is also important to consider a child’s functional vision when prescribing a specific add power lens design.
With regard to atropine, it is evident that the concentration impacts both the efficacy and the side effects and potential for rebound. Dr. Gifford noted that 0.05% atropine results in about 50% efficacy, 0.025% atropine results in about 33% efficacy, and 0.01% atropine has little effect. However, 0.01% atropine combined with ortho-k appears to create a better overall effect on reducing myopia and axial length progression.
Finally, we cannot forget about the impact of the environment on myopia progression. A significant association exists between more outdoor exposure and less myopia development.10 Bright light exposure plays a key role in lessening myopia development.11-13 In addition, smartphone use is a risk factor for myopia progression.14 Jan Roelof Polling, BOptom, reported that young people can spend an average of four hours per day on their smartphone and that continuous use for a minimum of 20 minutes without a break increases myopia and axial length. According to Scott Read, BAppSc(Optom), PhD, outdoor time of > two hours per day while wearing ultraviolet protection is recommended to either prevent myopia or to serve as an adjunct to other therapies in established myopes.
The bottom line is that the efficacy of any one—or combination of—treatment(s) varies from patient to patient such that practitioners should never guarantee that their selected modality will have a certain effect or that other modalities are to be ruled out.
Keratoconus The final general session was “Keratoconus and Corneal Ectasia: IS the paradigm shifting?” Moderated by Karen DeLoss, OD, this session had the following objectives: deep dive into the pathophysiology of keratoconus; how can this be linked to earlier detection, prediction of progression, and improve patient discussion; update on corneal imaging; understand key clinical considerations and treatment options; discuss how and when to implement treatments and/or combine treatments; discuss changes or shifts to clinical considerations with the introduction of corneal cross-linking (CXL) and with advances in specialty contact lenses and penetrating keratoplasty options; and discuss the long-term outlook for keratoconus patients given recent advancements.
Jan Bergmanson, OD, PhD, PhD.h.c., DSc, provided clinical insights from within the keratoconic cornea, the knowledge of which can help with clinical understanding of what is going on in these corneas and may help practitioners better manage patients. He pointed out that while we have known about keratoconus for 150 years,15 we have yet to discover where keratoconus comes from, how much inheritance plays into it, and what is actually happening in the cornea to cause the thinning and protrusion. He stated that keratoconus affects the entire cornea—it is a pan-corneal disease—but the epithelial effect of the disease is independent of what is happening in the stromal tissue and in the anterior limiting lamina (Bowman’s layer). He concluded that ectasia happens when you have lamellar splitting and anterior stromal tissue loss.
S. Barry Eiden, OD, discussed technologies for early keratoconus diagnosis and progression detection. He pointed out that early detection is so important because with CXL, practitioners can now intervene early to stop progression and preserve vision.
Dr. Eiden said that central pachymetry is one of the least reliable indicators of keratoconus. Better technology for early diagnosis includes placido topography, Scheimpflug tomography, anterior segment optical coherence tomography (AS-OCT), aberrometry, corneal biomechanics, and others. He then went on to explain the pros and cons of many of these methods and how to use the technologies to diagnose keratoconus or monitor progression.
Christine Sindt, OD, discussed keratoconus management options. She stressed that when managing keratoconus patients, the most important part of the initial visit is to let patients tell their story. You can usually tell when they feel that they’ve been heard when they stop talking. Once they stop, that is the practitioners’ opportunity to tell patients what they know and to present a clear plan.
Dr. Sindt also discusses all options—from spectacles to soft lenses to all types of specialty lenses—as well as costs and resources. The next step is to develop a care map outlining the fitting process, other medical care, potential roadblocks, and follow-up visits.
Dr. Sindt presented considerations for choosing a lens design and reminded attendees to not discount any modalities. For sclerals, she recommended technology that can measure scleral shape, whether profilometry or impression techniques.
Carina Koppen, MD, PhD, discussed surgical options used in managing keratoconus. She began with CXL and its effectiveness in stabilizing keratoconus progression. She noted that epi-on CXL is safer compared to epi-off CXL but is not as effective at stopping progression. Dr. Coppen also discussed surgical visual rehabilitation techniques for keratoconus as well as corneal transplants. She stressed the importance of informing transplant patients that there is a high likelihood that they will need glasses or contact lenses after the procedure to obtain functional vision. In her treatment paradigm for keratoconus, she noted that patients who have good tolerance for contact lenses should stay in contact lenses.

SCIENTIFIC POSTER & PHOTO AWARDS
FOR SCIENTIFIC POSTERS, WE HAD CLOSE TO 120 POSTERS IN three CATEGORIES. THE RECIPIENTS RECEIVE $300, $200, OR $100 GIFT CARDS
RESEARCH POSTERS
1ST PLACE: Pupillary Plus and Spherical Aberration Following Orthokeratology
–Randy Kojima; Patrick Caroline; Matthew Lampa, OD; Beth Kinoshita, OD; Mark André; Mari Fujimoto, OD; Alyssa Invergo, OD
2ND PLACE: Corneal Sagitta as a Predictor of Final Contact Lens Sagitta
–Daniel Fuller, OD; Kevan Smith, OD
3RD PLACE: Antimicrobial Efficacy of Two Hydrogen Peroxide Lens Care Products against Bacteria, Yeast, Mold, and Acanthamoeba with Rigid Gas Permeable Lenses
–Manal M. Gabriel, DDS, PhD; Cindy McAnally; Paul Shannon
CLINICAL CASE POSTERS SUBMITTED BY CORNEA AND CONTACT LENS RESIDENTS
1ST PLACE: Scleral Lens Management of Exposure Keratitis Secondary to Facial Nerve Paralysis
–Stephanie Tran, OD, MS; Chantelle Mundy, OD
2ND PLACE: A Case of Gas Permeable Lenses Dampening Nystagmus and Improving Vision
–Grace Tseng, OD; Michael G. Harris, OD
3RD PLACE: Losing Sleep Over a Scleral Lens
–Liandra Jung, OD
CLINICAL CASE POSTERS SUBMITTED BY NON-CORNEA AND CONTACT LENS RESIDENTS
1ST PLACE: Short-term and Long-term Challenges Associated with Inadequate Limbal Clearance in Scleral Lens Wear
–Michael Wong, MS; Celia Gong, OD
2ND PLACE: Everted Soft Contact Lens Overnight Orthokeratology on a Post-LASIK Patient
–Mari Fujimoto, OD; Patrick Caroline; Matthew Lampa, OD; Randy Kojima; Beth Kinoshita, OD; Mark André; Alyssa Invergo, OD
3RD PLACE: Undiagnosed Limbal Stem Deficiency Contributes to Multiple Contact Lens Failures
–Xiao Jing Xu; Eva Duchnowski OD
SCIENTIFIC POSTER COMPETITION HONORABLE MENTION:
Anisometropic Refractive Amblyopia Managed with Gas Permeable Versus Soft Lenses
–Vakishan Nadarajah, OD; Jenna Williams, OD
2021 GSLS PHOTO CONTEST WINNERS (in alphabetical order)
“Macro of Scleral Lens Fit” –Luciano Bastos
“Interesting Vessel Pattern” –Michael Harmon, OD
“Pond Plants” –Marco Sergio Tovaglia
CE BREAKOUT SESSIONS
This year’s CE Breakout sessions covered a variety of topics including telemedicine, hybrid lenses for pediatric patients, building a specialty lens practice, and a number of fantastic free papers.
Building a Specialty Lens Practice Stephanie Woo, OD, and Elise Kramer, OD, presented the CE Breakout Session “How to Build a Specialty Contact Lens Practice.” Dr. Kramer shared a photo of a contact lens vending machine from Russia. She noted that no two eyes are the same, one size does not fit all, and that contact lenses are medical devices that should be fit and not purchased in this way. She reminded practitioners that it is their job to fit contact lenses, not just dispense them, which is what a vending machine does.
One way to do this, of course, is to build a practice that is focused on specialty lenses. Dr. Woo noted that in a specialty lens practice, a significant difference is that the focus is on contact lenses rather than on the optical, which is the opposite of a primary care practice. In addition, practitioners who specialize in contact lenses have expertise in fitting multiple modalities including soft, GP, hybrid, scleral, post-surgical, myopia management, etc., and they often have a multitude of fitting sets, innovative technology, and custom lens offerings.
Dr. Kramer noted that having no optical is ideal for a specialty lens practice. She has an optical in her clinic, but it is not a focus of the practice. It is there for patient convenience, so that patients don’t have to go elsewhere for their glasses. Dr. Woo does not have an optical. She realized that she wanted to focus only on specialty lenses when she was establishing her new clinic, and once she made that a goal, she brainstormed ways to make that happen. She noted that other practitioners are more likely to refer patients to her because they know that she won’t steal their primary care or spectacle-wearing patients. On the flip side, Dr. Woo’s patients must go elsewhere for glasses and primary care.
If practitioners are interested in building a clinic focused on specialty lenses, Dr. Woo noted that they have to understand that this also includes a focus on diagnosing and treating corneal/anterior segment disease. Conditions that primary care practices would rarely see become almost common in a specialty lens practice. A specialty lens practice typically deals with contact lenses beyond refraction—for treatment, rehabilitation, and protection. Practitioners need great mentors and resources for the more uncommon conditions that they may see. Both Dr. Woo and Dr. Kramer emphasized that having a passion and a drive to fit specialty lenses is vital to success, especially when practitioners are first getting started with building up knowledge and a patient base.
Where could you practice as a contact lens specialist? Dr. Kramer noted that about half of contact lens specialists are in optometry-only private practice, followed by ophthalmology/optometry private practice and university clinics. There are many roads to get there and settings in which to implement this specialty.
Where can practitioners generate referrals? In primary care practice, practitioners can mention specialty lenses as an option to their patients. Other great referral sources include cornea specialists, ophthalmologists, general practitioners, ear/nose/throat specialists, oncologists, and rheumatologists. Dr. Kramer actually visited all of the cornea specialists and other specialists in her area to establish those relationships.
Drs. Woo and Kramer both suggested getting your name out there by becoming a leader within your community—local, state, national, and international associations and organizations, optical and otherwise—in addition to mentoring, research, volunteering, lecturing, publishing, and attending continuing education events.
Additional topics and pearls discussed in the breakout session included how to choose a location for a specialty lens practice, depending on whether practitioners are free to relocate or are settled in a particular area; incorporating research for contact lens companies into practice; incorporating a specialty lens practice within a larger practice; focusing on the value of the services provided and the patient experience rather than on selling products; and technology needed for a specialty lens practice.
With regard to technology, Dr. Kramer notes that the basic items needed are fitting sets, a slit lamp, and fluorescein. The rest is essentially a bonus. But, she notes that the more technology that practitioners have, the more that they can customize lens fits and the more possibilities that they can offer to their patients with less chair time.
Dr. Woo suggested starting out with refurbished or used equipment and upgrading to new equipment later. Practitioners can also consider referring to other practitioners for certain services, such as for axial length measurements. She stated that you can get creative and partner with other practitioners in the area who have equipment that you don’t want to or can’t purchase.
Once practitioners are more established with a specialty lens practice, corneal topography is important to manage disease and to monitor progression. For scleral lenses, profilometry can dramatically reduce chair time and improve lens fit. Optical coherence tomography is a consideration when a practice fits scleral lenses on a routine basis.
The session ended with a discussion of whether or not to take patients’ insurance. Dr. Woo does not take any insurance plans at all. She tells patients that she doesn’t want insurance dictating the care that she provides. Dr. Kramer takes insurance on a case-by-case basis, with the goal to get patients in the correct lens and seeing well.
Free Papers A highlight of the GSLS every year is the cutting-edge research, and 2021 was no exception. Some key findings from a few of the free paper presentations are provided here.
Nicholas Gidosh, OD, presented the free paper, “Multifocal Off-Center Optics Visual Effectiveness Study (MOOVES): 2nd Year Update.” He provided the results of assessing—in eligible subjects—scleral lenses ordered with 2.5mm near zones decentered to account for position assessed during diagnostic fitting. Subjects trialed the lenses in office at the dispense visit and were asked to provide subjective feedback on the experience. There were 53 subjects enrolled, and results were provided of those who had one-month data.
The average lens decentration was 1.75mm. The average scores (0 to 10 scale, 10 representing the most positive experience) provided by the subjects were distance acuity: 8.7; near acuity: 9.0; comfort: 8.7; overall experience: 9.0. For subjective blur and nighttime glare (0 for absent; 4 for severe), subjects reported an average of 1.1 for blur and 1.3 for glare. Sixty-nine percent were fit with only one attempt; the most common adjustment was to change the near zone size in one or both eyes (i.e., decreasing the zone size in the dominant eye to improve distance vision or increasing the zone size in the nondominant eye to improve near vision). Seventy-seven percent of eyes achieved distance vision within one line of best-correctable acuity. The authors concluded that the previous disadvantage of lens decentration can now be solved with reproducible manufacturing of decentered multifocal optic designs.
Randy Kojima presented the free paper “Profile of the Modern Orthokeratology Patient,” in which he reported on 155 consecutive patients (306 eyes) fit into orthokeratology lenses. The average age was 11.9 years; the average spherical refractive error was –2.94D (range: –0.50D to –7.50D); the average refractive cylinder was –0.45D (range: 0.00D to 2.25D); the average horizontal visible iris diameter was 11.7mm (range: 10.8mm to 13.0mm), and the average eccentricity value was 0.638 (range: 0.36 to 0.88). He concluded that 35% of the patients may require toric lenses, 38% may require custom diameters, and 18% could benefit from height/shape customization.
Boris Severinsky, OD, discussed “Therapeutic Scleral Lenses: From Vision to Ocular Surface Rehabilitation.” He presented a retrospective records review from the Emory University Department of Ophthalmology, Specialty Lens Service in which 183 patients (281 eyes) were fitted with scleral contact lenses. The indications for fitting included visual rehabilitation and therapeutic use for ocular surface disease (OSD).
Dr. Severinsky found that 94 eyes (33.5%) were fitted for OSD management and that 187 eyes were fitted for irregular cornea (i.e., keratoconus, post-refractive surgery, etc.). The OSD patients had an average wearing time of 10 hours per day, with an average of 1.7 breaks in wear; the irregular cornea group had an average wearing time of 12 hours per day, with 0.6 breaks per day on average. The OSD etiology included the following:
- Severe dry eye/keratoconjunctivitis sicca of autoimmune etiology: 38 eyes
- Graft-versus-host disease (GHVD): 18 eyes
- Neurotrophic keratitis (NK): 15 eyes
- Ocular cicatricial pemphigoid (OCP): 11 eyes
- Stevens-Johnson syndrome (SJS): six eyes
- Exposure keratitis: six eyes
Eighty-eight percent of eyes fitted for ocular surface indications responded well to therapy and continued with scleral lens wear; the highest success rate was recorded in OCP (98%), GVHD (86%), and NK (80%) scleral lens-wearing eyes. The visual acuity among OSD patients improved from 20/80 to 20/30. Dr. Severinsky also reported that 20% of the referrals were from non-ophthalmology providers.
It was concluded that a higher penetration rate of scleral contact lenses for OSD management is present today than in previous years. In addition, patients who have severe inflammatory conditions (GVHD/OCP) are most appreciative of scleral contact lens benefits. Finally, increased awareness of therapeutic benefits of scleral contact lenses among other specialties allows for timely referrals and might save sight in many cases.
“Multifocal Hybrid Lenses for Pediatrics,” presented by Melanie Frogozo, OD, and Stephanie Fromstein, OD, discussed contact lenses in the pediatric population.
Dr. Frogozo noted that there are so many reasons to fit children into contact lenses: aphakia (congenital or due to trauma), corneal irregularity, refractive issues, myopia control, nystagmus, ocular surface disease, photophobia, and amblyopia. If these issues are not addressed, then in addition to not currently seeing well, their vision may not develop normally or they could become blind. She notes that some practitioners are hesitant to fit this population into contact lenses, but if they empower the children and their families, they will be surprised at what these young patients can do. She told of one 7-year-old patient who can apply and remove his scleral lenses completely unassisted.
Soft, GP, and hybrid lenses are all options for children. Dr. Frogozo likes hybrid lenses because of their optics, stability, and handling and care. Kids often will not experience lens awareness because they tend to have a more stable, thicker tear film than adults do.
Dr. Fromstein then reviewed the history of hybrid lenses. Past issues included low oxygen permeability and durability. She noted that current hybrid lenses have higher oxygen permeability, are more durable, have improved designs, and include coatings that make them more wettable. Additionally, hybrids are now available with aspheric GP optics and multifocal designs. In the future, there will be increased options and individualization (e.g., more base curve and skirt options); updated algorithms for online ordering; increased optic zone; and edge redesign.
Dr. Fromstein also discussed several case studies and explained why she chose specific lenses for those cases. For empirically fitting a regular cornea hybrid lens design, practitioners can use a calculator. Simply input Ks, manifest refraction, and horizontal visible iris diameter, and the calculator determines the lens. Often, it will calculate any residual astigmatism as well. During evaluation, there is no need for solutions or sodium fluorescein (NaFl). If there is already NaFl on the eye, she jokingly noted that practitioners don’t have to worry about joining the “Golden Button Club,” because it won’t stain the hybrid lenses. Let the lens settle for 10 minutes and look for coverage, centration, and movement. Follow up with patients one week after dispense to check for acuity and spherical over-refraction. Practitioners should also review wear time, replacement, and care. She noted that troubleshooting is relatively straightforward, because only the skirt curve or the base curve can be altered.
Dr. Frogozo then talked about using multifocal hybrid lenses for myopia control. She explained that multifocal center-distance contact lenses have been shown to decrease the progression of myopia by 43% to 46%.1
Hybrid aspheric multifocal lenses are good for patients who have a higher amount of astigmatism. These lenses come with varying optic zones based on photopic pupil size and with add powers up to +5.00D. In addition, the soft skirt can help with centration. Dr. Frogozo noted that when she first started prescribing these lenses, she was hesitant to prescribe higher adds because she was concerned about blur. However, she found that even with +2.00D adds, her patients were progressing in axial length faster than what she expected. So, she switched to higher adds. She suggested increasing the minus by one-quarter or one-half diopter if patients are experiencing blur.
Next, Dr. Fromstein described hybrid lenses with extended depth of focus (EDOF) designs. She noted that multiple higher-order aberrations create EDOF and are more robust for pupil changes, aberrations, and decentration.
Hybrids can also be used for irregular corneas, most commonly for patients who have keratoconus. The first step when fitting this design is to optimize the vault, with the ultimate goal of being between 100 and 150 microns. Next, optimize the skirt; Dr. Fromstein says there should be an even division of labor between the GP center and the peripheral skirt. Next, perform an over-refraction. The follow up will be very similar to one performed for a regular cornea lens. With this lens, however, examine the staining (i.e., the fluorescein pattern with the lens on) to determine whether there are any fit issues. The session ended with Dr. Frogozo talking about using hybrids in specialty cases such as for high hypermetropia, cosmetic use, or for those who have irregular scleral toricity.
References
- Bullimore MA, Richdale K. Myopia Control 2020: Where are we and where are we heading. Ophthalmic Physiol Opt. 2020 May;40:254-270.
Telemedicine Clarke Newman, OD; Marcus Noyes, OD; and John D. Gelles, OD, presented the CE Breakout session “Telemedicine and Scleral Lenses: The Genesis of a New Way to Deliver Care.” Dr. Gelles noted that virtual care for scleral lenses is a largely unexplored area as far as published literature. But, the COVID-19 pandemic acted as an impetus to provide telehealth, especially during the lockdown period, when there was a need to provide care for patients at a distance.
One article, published in June 2020, reported that telehealth was helpful for gross analysis, enhancing compliance during the pandemic, subjective refraction, and visual acuity; for imaging, the article concluded that adjunctive devices were needed that patients might not have at home.1
Dr. Gelles discussed challenges to using telehealth for a patient exam, explaining that it depends on where the patient is located — in office or out of office—because that dictates what technology is used. For instance, if the patient is in the office but the practitioner is out, technicians perform the tests and upload the data to the electronic medical record (EMR); so as long as a practice has qualified technicians in the office who can perform all of the scans and flip lids, the practitioner doesn't need to be physically present. Video calls can be used for patient interaction during testing. The practitioner can come into the exam room to perform a quick check of a patient, then leave the room and have a discussion with the patient from another room using a video conference. It’s the same elements of the exam as before, just with applying different pieces of technology in new ways, Dr. Gelles noted.
As another example, videos can be taken with a tablet while a patient is at the slit lamp for a peer-to-peer video conference to discuss the fit with a consultant. Drone slit lamps offer real-time control from another location with a virtual reality headset for a stereoscopic view. Dr. Gelles noted that the technology has advanced such that we have the ability to transfer data back and forth; we have the ability to obtain noncontact scans with profilometry, which provides the full geometry of the eye from which the resulting lenses can be empirically designed; and we have the ability to non-contact evaluate the patient—this allows the possibility of multiple satellite clinics, with cost being the main initial barrier.
What do you do when a patient is at home with only a cell phone? Dr. Gelles pointed out that the newest smart device camera lenses are more advanced, and better imaging processors and algorithms result in much higher quality images. When patients are provided with specific instructions for how to take pictures and video with their smartphones, they can achieve good quality images and videos that can allow practitioners to remotely assess an eye. Dr. Gelles said that telehealth has been most useful to him with regard to evaluating scleral lenses by allowing him to see what an eye looks like at the end of the wearing day, which he’d never be able to see in office.
Dr. Noyes stated that patient-supplied photos taken with their phones can serve as a great screening tool in determining whether they need to come to the office right away or whether they can wait a week. Both Dr. Noyes and Dr. Newman said that with good-quality images, even subepithelial infiltrates could be detected with imaging and videos that patients took at home.
Telemedicine can also be used to initiate treatment for a severe condition (e.g., graft rejection) if a patient is unable to immediately come to the office, but then the patient must come for an in-person examination as soon as they are available to do so. Telemedicine and patient-guided exams will miss things that practitioners wouldn’t miss during an in-person exam, so it needs to be emphasized to patients that telemedicine is adjunctive and can’t replace in-person care. In addition, Dr. Newman pointed out that if practitioners fail the standard of in-person care, regardless of the technology that they have with them, they’re going to have legal exposure.
Dr. Gelles discussed the limitations of telemedicine evaluations. Some of these can be alleviated with smartphone diagnostics and filters as well as by sending items to patients for use at home such as fluorescein strips and blue LED lights to improve remote evaluations when necessary.
Dr. Noyes then spoke about artificial intelligence (AI) on the horizon. One example is an FDA-approved retinal fundus camera that is used for rural screenings of diabetic retinopathy. If the AI detects signs that a patient has diabetic retinopathy, that patient is then sent to an office for in-person evaluation. The AI is not replacing care; it is a screening tool to identify who needs to come in for care. AI is also on the horizon for certain types of anterior segment evaluation. It could - in the future - serve as a screening tool for identifying adverse events from contact lens wear in addition to many other potential applications related to contact lenses.
Dr. Newman discussed telehealth billing and coding during the pandemic. He reviewed changes and additions that were made to telehealth-related codes to allow practitioners to receive reimbursement during the pandemic, including what they need to do to obtain reimbursement under each code. He emphasized that patients must provide consent for their insurance plan to be billed for these telemedicine services; if this is not documented, then a practitioner cannot bill for them, and if the patient does not provide consent, care must still be provided because the patient cannot be abandoned. It is likely that not all of the changes/additions to the codes will remain in effect once the pandemic is over.
Reference
- Nagra M, Vianya-Estopa M, Wolffsohn J. Could telehealth help eye care practitioners adapt contact lens services during the COVID-19 pandemic? Cont Lens Anterior Eye. 2020 Jun;43:204-207.
GP Lens Update Dr. Bennett presented the CE Breakout session “GP Lens Update,” which was sponsored by the GP Lens Institute (GPLI). He discussed updates on current trends as well as on lens materials and coatings, ortho-k, and scleral, multifocal, toric, and spherical lens designs. The following are some of the highlights.
- Eleven percent of contact lens fits and refits in the United States are with GPs.1
- The biggest advancements in GP lenses in 2020 (per a survey of the GPLI Advisory Board)2
- Introduction of stable, wettable, 200-Dk materials
- Profilometry/topography-driven scleral designs
- Custom-back-surface scleral designs (toric haptics, quadrant-specific)
- New GP disinfection guidelines,3 also available for download from www.gpli.info (under “Resources” and then “Order Printed Materials”)
- New ortho-k lens designs
- Overnight ortho-k
- Empirical fitting has demonstrated very good (80%)4 first-fit success
- Due to the larger diameter, limited movement, low edge clearance, and overnight wear schedule, adaptation can occur within a few nights
- The incidence of microbial keratitis is no greater than with conventional extended wear5
- An excellent overview article was recently published by Drs. Mark Bullimore and Leah Johnson6
- Lens materials, coatings, design, and fitting
- Improvements in oxygen permeability, surface wettability, greater flexural resistance, better memory/less warpage, and scratch resistance are characteristic of current materials versus their predecessors
- The most recent material approved by the FDA has a Dk of 200
- A new solution for patients to use at home to help restore the polyethylene glycol-based coating launched in January
- Scleral lenses
- The Scleral Lenses in Current Ophthalmic Practice: an Evaluation (SCOPE) study reported that 74.2% of scleral fits are to irregular cornea patients, 16.1% to ocular surface disease patients, and 9.7% to healthy eyes (i.e., astigmatism, presbyopia)7
- When the Contact Lens Spectrum readership was recently surveyed as to which contact lens option they fit to irregular cornea patients, the “go to” lens was sclerals.2 Fifty-two percent of respondents fit ≥ 50% of their patients into sclerals, followed by 18% in small-diameter GPs, 10% in intralimbals, 5% in hybrids, and 4% in custom soft
- A recent study reported on the safety of scleral lenses.8 In a sample size of 157, there was a total of 9.6% adverse events, with only a few being significant complications. It was concluded that overall, scleral lens wear is quite safe
References
- Nichols JJ, Fisher D. Contact Lenses 2020. Contact Lens Spectrum. 2021 Jan;36:24-29, 51.
- Bennett ES. GP Annual Report 2020. Contact Lens Spectrum. 2020 October;35:28-30,32,34,36,37,59.
- Sindt C, Bennett E, Szczotka-Flynn L, Sclafani L, Barnett M, American Academy of Optometry (AAO) Section on Cornea, Contact Lenses & Refractive Technologies, The American Optometric Association (AOA) Contact Lens and Cornea Section. Technical Report: Guidelines for Handling of Multipatient Contact lenses in the Clinical Setting. Optom Vis Sci. 2020 Aug;97:544-548.
- Davis RL, Eiden SB, Bennett ES, Koffler B, Wohl L, Lipson M. Stabilizing myopia by accelerating reshaping technique (SMART)-study three year outcomes and overview. AOVS. 2015 Apr 21;2:92-98.
- Bullimore MA, Sinnott LT, Jordan LA. The risk of microbial keratitis with overnight corneal reshaping lenses. Optom Vis Sci. 2013 Sep;90:937-944.
- Bullimore MA, Johnson LA. Overnight orthokeratology. Cont Lens Anterior Eye. 2020 Aug;43:322-332.
- Schornack M. The SCOPE Study: An Overview. Contact Lens Spectrum. 2017 Dec;32 25-28,30,32.
- Fuller DG, Wang Y. Safety and Efficacy of Scleral Lenses for Keratoconus. Optom Vis Sci. 2020 Sep;97:741-748.
Ortho-k Basics On the final day of the conference, Jason Compton, OD, and Shalu Pal, OD, presented “Ortho-k Basic Fitting, Clinical Tips and Practice Growth Strategies.” The session began with a definition of ortho-k and a look back at its history. Simply put, the reverse geometry design of the lens, with the assistance of the tear film, creates a pressure gradient across the lens. There are some limitations with these lenses. For example, they are ideal for those who have myopia between –1.00D and –6.00D and astigmatism up to –2.00D.
Dr. Compton mentioned that the best ortho-k candidates have regular corneas, are nearsighted, have low-to-moderate astigmatism, and are highly motivated. Pay special attention to candidates who have dry eye disease or ocular allergies. It’s important to tell parents that the FDA did not put any age restrictions on the use of ortho-k and that, as myopia tends to advance more when children are younger, it would be wise to start as early as possible.
Dr. Pal noted that communication with patients is very important. Practitioners should think about the specific words that they use to explain the benefits (e.g., “peace of mind,” “non-surgical,” “safe,” etc.). Involving the kids in the process can help make it more successful. Barriers to moving forward include lack of understanding, fear of contact lenses, and parental concerns about having to do the work as well as about the time and/or the cost. Practitioners need to show parents what the value is.
Dr. Compton believes that involving the entire team in the office is critical. The staff at the front desk can start with messaging, scheduling appointments, and distributing marketing materials. Technicians can start the conversation about ortho-k. They can also perform any additional testing and handle education and training. In-office coordinators can help reduce chair time by handling conversations before the practitioner even walks in the door. Other coordinator duties may include pretesting, obtaining consents (including financing), and communicating with the laboratory about lens orders. Training staff takes time on the front end, but different staff members need different levels of understanding; someone working the front desk only needs a low-level elevator pitch, while the coordinator needs to know all of the nuts and bolts of ortho-k.
Dr. Pal reviewed the various fitting philosophies: empirical ordering, trial lenses, or custom designed. Regardless of which design you choose, an ortho-k lens should be well-centered, with little movement. Toric lenses should be used when there is more than 0.50D difference in Ks, when you see edge-to-edge astigmatism on topography, or if you see a fuzzy oval pattern in the treatment zone (where it should be round). Dr. Compton noted that many manufacturers have calculators that can help practitioners determine whether a toric design is indicated.
If patients return with uncorrected power in their over-refractions, make sure that they have worn the lens for at least eight hours. Then doublecheck your calculations. Sometimes the fit is correct, but it just needs more time to work. If the fit is indeed poor, check the centration and alignment curve. Other vision complaints may include glare and ghosting, inconsistent vision, or discomfort. When you have a patient who is having trouble with vision but already has lenses, Dr. Pal suggests starting from scratch after a complete washout period.
If patients decide they are done with ortho-k, it may take several months to get back to their natural visual state. Dr. Pal provides patients with contact lenses during that regression time and includes the cost of the lenses in a regression fee.
Next, Dr. Compton provided details about what should be accomplished during exams—from the initial consultation to the lens fitting to the various follow-up visits (first day, one week, and one month). He then tackled issues surrounding billing strategies. He noted that, while ortho-k is not covered by insurance (because it is considered elective), many of his patients use their flexible spending accounts to pay for the procedure. Dr. Compton uses global fees so that patients are aware of all costs upfront. When determining what the fee should be, practitioners (especially those new to doing ortho-k) should take everything into consideration such as chair time, lost or damaged lenses, and changes in treatment. There also should be transparency throughout the process. Specifically, the informed consent documents should be very clear, should outline patient responsibilities, and should include details about prices, warranties, materials, and refunds.
Dr. Compton then completed the session by detailing various marketing options for growing an ortho-k practice. He says that this includes internal marketing (playing videos in your reception room, supplying materials throughout the office, recall systems, emails) and external marketing (gaining new customers). He then walked attendees through the setup of a myopia management ad on a Facebook business page.
HOPE TO SEE YOU ALL NEXT YEAR
The 2022 GSLS meeting is scheduled to take place from Jan. 19 to 22 at Bally’s Hotel and Casino in Las Vegas. CLS
Dr. van der Worp is acknowledged for his contribution to the myopia session information in this article.
REFERENCES
- Michaud L, Lipson M, Kramer E, Walker M. The official guide to scleral lens terminology. Cont Lens Anterior Eye. 2020 Dec;43:529-534.
- Bennett ES. GP Annual Report 2020. Contact Lens Spectrum. 2020 Mar;35:28-30,32,34,36,37,59.
- Nichols J, Fisher D. Contact Lenses 2020. Contact Lens Spectrum. 2021 Jan;36:24-29,51.
- van der Worp E, Lampa M, Kinoshita B, Fujimoto MJ, Coldrick BJ, Caroline P. Variation in sag values in daily disposable, reusable and toric soft contact lenses. Cont Lens Anterior Eye. 2021 Jan 7;S1367-0484(20)30200-9. [Online ahead of print]
- Wang J, Li Y, Musch DC, et al. Progression of Myopia in School-Aged Children After COVID-19 Home Confinement. JAMA Ophthalmol. 2021 Jan 14:e206239.
- Brennan NA, Toubouti YM, Cheng X, Bullimore MA. Efficacy in myopia control. Prog Retin Eye Res. 2020 Nov 27:100923.
- Pauné J, Fonts S, Rodríguez L, Queirós A. The Role of Back Optic Zone Diameter in Myopia Control with Orthokeratology Lenses. J Clin Med. 2021 Jan 18;10:336.
- Lau JK, Vincent SJ, Cheung SW, Cho P. Higher-Order Aberrations and Axial Elongation in Myopic Children Treated With Orthokeratology. Invest Ophthalmol Vis Sci. 2020 Feb 7;61:22.
- Walline JJ, Walker MK, Mutti DO, et al. Effect of High Add Power, Medium Add Power, or Single-Vision Contact Lenses on Myopia Progression in Children: The BLINK Randomized Clinical Trial. JAMA. 2020 Aug;324:571-580.
- Jones LA, Sinnott LT, Mutti DO, Mitchell GL, Moeschberger ML, Zadnik K. Parental history of myopia, sports and outdoor activities, and future myopia. Invest Ophthalmol Vis Sci. 2007 Aug;48:3524-3532.
- Read SA, Collins MJ, Vincent SJ. Light Exposure and Eye Growth in Childhood. Invest Ophthalmol Vis Sci. 2015 Oct;56:6779-6787.
- Cao K, Wan Y, Yusufu M, Wang N. Significance of Outdoor Time for Myopia Prevention: A Systematic Review and Meta-Analysis Based on Randomized Controlled Trials. Ophthalmic Res. 2020;63(2):97-105.
- Read SA, Vincent SJ, Tan CS, Ngo C, Collins MJ, Saw SM. Patterns of Daily Outdoor Light Exposure in Australian and Singaporean Children. Transl Vis Sci Technol. 2018 May 29;7:8.
- McCrann S, Loughman J, Butler JS, Paudel N, Flitcroft DI. Smartphone use as a possible risk factor for myopia. Clin Exp Optom. 2020 May 25. [Online ahead of print]
- Nottingham J. Practical observations on conical cornea: and on the short sight, and other defects of vision connected with it. London: J. Churchill, 1854.




