Eyecare professionals (ECPs) have been encouraging patients to blink fully and frequently for quite some time now. Current technology allows ECPs to analyze blink rates, blink quality, and, more specifically, the mechanism of the blink.
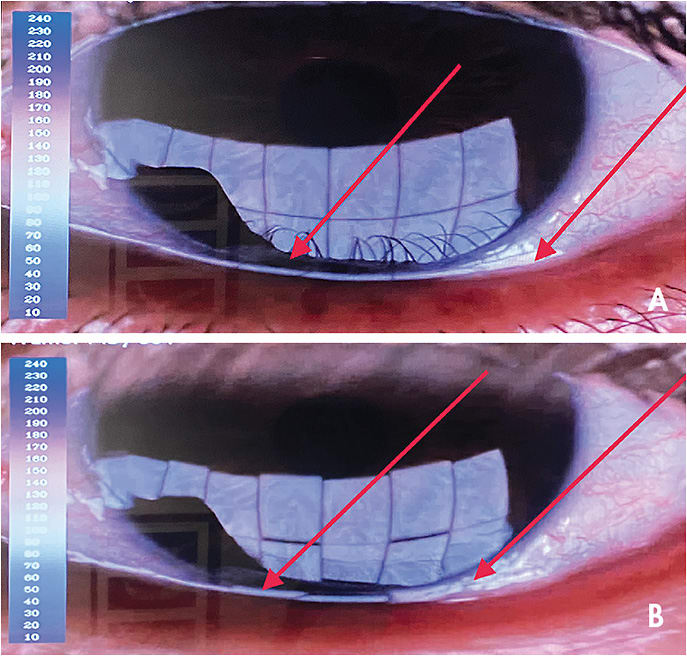
I (Dr. Gee) discovered an interesting phenomenon with one of my patients during a recent visit. She had mild meibomian gland truncation, so I brought her back for computerized blink analysis. The instrument that I used can quantify a patient’s lipid layer thickness and analyze how many blinks are produced over a 20-second interval. Even more revealing is whether those blinks are partial or complete. The video capture can be further broken down into a frame-by-frame analysis and shown to patients for educational purposes. While I have traditionally blamed incomplete blinks on “lazy” blinking, I have discovered that this sometimes also occurs as a result of a mild ectropion of the lower lid during the blink itself (Figure 1). If the technology described previously is unavailable in a practice, this phenomenon also can be visualized via sodium fluorescein pooling in the tear meniscus upon blinking and can be enhanced with slit lamp video capture.
A Novel Treatment Option
This particular type of “blink ectropion” may be caused by the development of lower lid laxity due to age or to mechanisms related to years of GP lens removal and makeup use, etc. (Bergstrom and Czyz, 2021). My intrigue in this area led me to investigate radiofrequency thermal treatment (RFTT) (off-label). The basic premise is that RFTT helps strengthen collagen bonds of the periorbital skin, which brings the lower lid into better apposition to create a more full and forceful blink (Oh et al, 2016). An added benefit is that patients also enjoy a non-invasive approach to reducing under-eye bags as well as fine lines and wrinkles (Carruthers and Carruthers, 2007).
The treatment is simple, non-invasive, and takes about 10-to-15 minutes per eye. It can be conducted by practitioners or by a well-trained technician. Ultrasound gel is applied generously around the periorbital area, and a stylus-like probe is massaged in a circular fashion around the orbital rim while the temperature is slowly increased to 105º F. Boney prominences and the globe itself are avoided. There are no restrictions following the procedure.
A Technology to Consider
RFTT has played a significant role in my practice and in our Ocular Surface Disease and Restoration Center. If ECPs are looking to expand further into dry eye care, this may be a viable option. Paying close attention to the blink mechanism is key to success in general, but especially if you choose to adopt this type of technology. CLS
For references, please visit www.clspectrum.com/references and click on document #306.




