In optometry school, a mentor of mine said: “As a rule of thumb, if a contact lens-wearing patient has a red eye, nine times out of 10, the contact lenses are to blame.” There is some truth to this, as patients are not always compliant with their lens care. An older study showed that 99% of the surveyed lens wearers reported engaging in at least one risky contact lens hygiene-related behavior (Joslin et al, 2007). Luckily, there are some corneal conditions that have classic pathognomonic characteristics.
One of these conditions is Thygeson’s superficial punctate keratitis (TSPK) due to its unique arrangement of central or paracentral bread-crumb-like intra-epithelial opacities that usually spare the peripheral cornea. This chronic and often recurrent condition usually presents with photophobia, foreign body sensation, reflex epiphora, and mildly reduced visual acuity, with minimal conjunctival injection or discharge. Although TSPK is considered idiopathic, some report an associated mechanism linked to viral as well as immunologic etiologies including HLA-DR3 antigen markers (Priyadarshini et al, 2021).
A TSPK Example
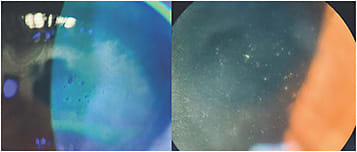
A 36-year-old female presented with worsening symptoms of bilateral photophobia, burning, and foreign body sensation over the last three-to-four months. She reported a prior diagnosis of dry eye and wondered whether this was a “flare-up.” Artificial tears, over-the-counter topical decongestants, and daily disposable contact lenses provided mild relief, and biomicroscopy revealed multiple small, grey-white, granular, intra-epithelial opacities in the central and paracentral corneas with overlying positive and negative punctate staining (Figure 1). Aside from mild obstructive meibomian gland dysfunction and trace conjunctival injection, no discharge, anterior chamber reaction, or other signs of infectious etiologies were observed. Best-corrected visual acuity was 20/25 in each eye, and all other exam findings were unremarkable.
The patient was diagnosed with TSPK. She was instructed to discontinue lens wear and to start preservative-free artificial tears four-to-six times per day along with loteprednol etabonate 0.38% gel q.i.d. in both eyes for two weeks, then taper to b.i.d. in both eyes for two weeks.
At her one-month follow up, she showed significant improvement, with only a few intra-epithelial lesions remaining (Figure 2). She was cleared to return to lens wear, and we discussed the use of off-label steroid-sparing calcineurin inhibitors, such as tacrolimus 0.02%, for chronic management, if needed, to manage future flare-ups.

More Advice
Contact lenses also play a role in influencing anterior segment disease, even if they aren’t the underlying cause. Remember to apply the “3 Ms”: contact lenses either mimic, mask, or multiply corneal pathology. CLS
For references, please visit www.clspectrum.com/references and click on document #312.




