It has been more than 50 years since soft contact lenses were invented, and let’s be honest, who is going to admit to having been around all that time? To get an idea of how soft lenses have evolved over the last 50 years, we sought out the views of an entity that marks the passage of time in decades rather than in years; that is, a busy contact lens practice. Here is what it had to say.
1971
Meet Peter. He’s heading off to college later this year and wants to be “glasses free” when he arrives. So, he’s been coming to the office to get fit with contact lenses. The first visit didn’t go so well. It’s always the big guys who pass out when the first lens goes on, and he just went out like a light and nearly slid right out of the chair! We had to give him credit though, because once he came around and had a chance to recover, he was keen to try again.
Eventually, we did get him started and ordered a pair of hard lenses. When he came back for aftercare, he had this odd, kind of surprised look about him. You know the sort of thing, a bit wide-eyed and staring, and he didn’t want to blink much. He said that he was constantly aware of the lenses and struggled to get his wearing time up beyond an hour or two before he had to take them out. We persevered for a while, but after a few weeks, he had to admit that hard lenses weren’t for him.
We’d been hearing reports of “soft” contact lenses coming out of Czechoslovakia for about the last 10 years.1 While there seemed to be a few problems with vision and durability,2 they sounded interesting. Examples were becoming available in North America and Europe,3 albeit largely for therapeutic purposes. Additionally, because the U.S. Food and Drug Administration (FDA) approved them for clinical use in the United States just this year, it seemed that they might provide an alternative for Peter. Therefore, we suggested that he give them a try.
His first response said it all: “Oh, wow...these are fantastic! Way better than my old lenses.” In no time at all, he was up to eight hours a day and was much happier. Of course, it wasn’t all smooth sailing. Handling the flexible, wet material was tricky at first, and it took him awhile to get used to their fragility, compared to poly(methyl methacrylate) (PMMA). He stores them in saline, which he makes from salt tablets, and he disinfects them every day in a little heater unit (Figure 1).

Occasionally, he traps a lens in the case when closing it up. Once, he even “fried” a pair when he forgot to put in the saline. All in all, it is working out to be relatively expensive for him, which is probably why he sometimes keeps wearing a lens, even if it’s damaged. No doubt, his hard lens experience stands him in good stead to tolerate the discomfort!
From our point of view, we do think that his eyes look a bit red by the end of the day. We suspect that there may be some corneal edema, although it’s hard to tell for sure without a pachymeter.4 Overall, he’s having a good outcome, and it has made us quite positive about offering soft lenses as an option for other patients. It’s a shame that they don’t work well for astigmats.
1976
We have a good number of soft lens wearers now. However, until recently, we could only fit those who had low levels of astigmatism. Some practitioners claim that soft lenses can “mask” astigmatism, but we generally find that it manifests as poor vision sooner rather than later. It’s good that a few companies are starting to offer soft torics now, and we have patients wearing them.
Julie is one of those patients, and her case demonstrates the challenges. She has 2.50D of corneal cylinder; of course, if she was wearing hard lenses, the post-lens tear film would take care of that. For her to obtain good vision with soft torics, the lenses have to be stopped from rotating so that the axis of their optical correction remains correctly orientated, just as in spectacles.
There are several different ideas among the manufacturers as to the best way to prevent rotation, including truncation, thin-zones, and prism ballasting. The problem is that they don’t all work in all eyes, nor are they equally comfortable. In Julie’s case, we had to go through two or three designs until we found one that remained adequately stable with blinking and eye movement.
The next problem came when she collected the lenses. One was fine, but the other one provided really poor vision. As far as we could tell, our specification was correct, but the lens didn’t behave as expected on the eye. As we now understand, how these lenses are made involves a degree of variability. In one process, the buttons are crimped during lathing, and the toric surface emerges once the compression is released.5 Obviously, some considerable skill is involved in getting this right, and we have come to expect that there will be inconsistencies from lens to lens. Some colleagues refer to them as “snowflake lenses,” because every one is unique, but perhaps that is a bit harsh. Nevertheless, the situation is very frustrating for Julie as well as for us.
1981
Our first appointment this morning was Mary, who was here for an urgent care visit. Normally, she comes every three months—regular as clockwork. So, it was obvious that all was not well. She is aphakic and is about five years post-surgery. The only time her contact lenses leave her eyes is when we take them out. Right after her cataracts were removed, she got a pair of +15D glasses. Although she could see really well, she hated that she looked like (in her words) a cartoon character. For the last two years though, she has been wearing 75%-water-content, extended wear soft contact lenses, and it’s amazing to see the change in her self-esteem. Today, though, she was obviously unhappy and said that she woke up with a sore left eye.
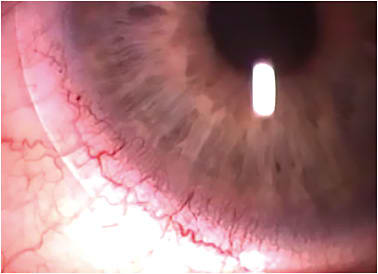
With the biomicroscope, there was a lot to see. Apart from some evident bulbar redness in the left eye, there was a small, round, white lesion in the peripheral cornea at about 7 o’clock that ultimately stained brightly with fluorescein. The lens itself looked pretty hazy, with a protein film on its front surface, and it wasn’t wetting very well. There were also a few raised deposits, which we recognized as lens calculi or jelly bumps, scattered across the surface (Figure 2). On taking the lens out, it looked quite yellow and discolored and was slightly out of shape. A final check of the cornea showed some residual corneal edema, with a couple of vertical striae lingering from last night’s sleep as well as a few new vessel spikes encroaching onto her cornea superiorly (Figure 3).


Ah well, while this was a bit distressing for Mary, it was not that much out of the ordinary. We’ve seen a few of these peripheral ulcers, and they usually self-limit. The discomfort is already improving, but we’ll get her some drops, check in later today, and see her again in the morning. It’s back to spectacles in the meantime though, so she’ll hate us for that.
At least it will give us a chance to clean the lenses up a bit. We can get some of the protein off by heating them in a sodium perborate solution for an hour or so. There is not much that we can do about the jelly bumps without damaging the lens surface, though. Mary did mention that she thinks her lenses have been feeling scratchy of late, so that’s likely because these things are getting bigger and interacting with her eyelids when she blinks. If that persists after cleaning, she will have to seriously consider buying a new pair.
It would be nice to get some more oxygen through to her corneas as well. However, we are about at the limit in terms of water content, so not much that we can do on that score except monitor the situation.
Presbyopia has always been tricky from a contact lens point of view. For many early presbyopes, it’s the first time in their lives that they have needed vision correction, and quite a few ask about whether contact lenses can do the job rather than having to wear glasses. It’s no surprise that soft lenses are highly preferred by this group. Unfortunately, while rigid bifocals can translate reasonably well on-eye—so that their distance or near portions align with the visual axis as required—the inherent stability of a soft lens tends to work against it in this regard. Because of that, we have relied heavily on monovision, which has been quite successful. Not everyone can accept the binocular compromise, though, so we are interested to see that the FDA has approved a few lenses that use simultaneous imagery.6 Although the complexity of the optics is bound to produce some degree of compromise,7 they should at least allow a more balanced correction in both eyes.
1988
Ian was here today. He is a real party animal, so much so that we call him “candle in the wind” because he is always going out! He uses extended-wear lenses, which we thought long and hard about because of his history of noncompliance when he wore regular soft lenses on a daily basis. Frankly, he slept in those so many times, we felt that he might as well have a lens that was specified for extended wear in the first place. He started out in a high-water lens and, not surprisingly, loved the idea that he didn’t need to take them out before falling asleep. He disappeared not that long ago for the better part of a year. When he came back, the lenses were a bit of a mess. One of them actually had a nick at the edge that was giving him some discomfort and is probably the only reason why he thought to come in. On top of that, he obviously hadn’t cleaned them since the day they were dispensed, let alone once every couple of weeks as he was told to do. Fortunately, we’d just started working with weekly disposable lenses at about that time, so we were able to recommend those to him.
The concept had been invented in Denmark a few years previously,8 and commercial lens systems were now more widely available. Although they have a water content that is lower than that of his previous lenses, the fact that he throws them away every week means that he doesn’t need to worry about cleaning, and neither do we. He comes in every three months now to pick up his new lens stock, which is a great opportunity for us to check out his eyes. The overall picture is so much better now. He does have a bit of limbal flush (Figure 4), probably due to lack of sleep, and quite lot of corneal microcysts, which suggest that his corneas could do with more oxygen. In general, though, he’s doing well.
1996
Mike is one of our problem cases. The biggest concern is that he has had episodes of papillary conjunctivitis in the past, and avoiding further flare-ups is a key part of his care. He is a big depositor (Figure 5). And, although he understands that keeping his lenses clean is an essential part of his daily routine, manual cleaning was always a chore for him; it wouldn’t be surprising if his compliance was less than 100% in this. We already knew that regular lens replacement was critical in his case, so now that the technology has advanced to make it possible to dispose of lenses on a daily basis, it was a no-brainer to put him on that schedule. It is a little more expensive, but having a fresh, clean surface on the eye every day has to be a good thing for Mike as well as for some of our other patients.9 How we are going to manage the logistics of having 700+ lenses in the practice for every wearer? We haven’t worked that out yet.

2001
We have a few extended wearers in the practice. They adore the convenience aspect of wearing lenses this way and are really enthusiastic. But, it is a modality that we view with some caution because of the reports of associated microbial keratitis. We have not seen any cases ourselves; so far, we’ve been lucky. Nevertheless, at aftercare, all of these eyes show some evidence of hypoxia, irrespective of what lens type is being worn. We have always felt that a more highly oxygen-transmissible lens would be safer. Up until recently, there were only two ways to do this—make the lenses thin or from a very high-water-content material—and you can only go so far in either of these directions before the lens becomes impossible to handle or damages the cornea.10,11
So, hearing about new materials that incorporate silicone as the oxygen-transmitting element has been very interesting. We did have a couple of people try out silicone elastomer lenses a few years ago, but problems with poor wetting and binding to the ocular surface12 made us cautious. These newer lenses are a silicone hydrogel co-polymer and have an oxygen permeability of 140Dk! We refitted Angela with these lenses six months ago, and she was in today for a check-up.
She said that while the lenses weren’t as comfortable initially as her hydrogels, she soon got used to that and loves being able to wear them for 30 nights at a time before switching to a new pair. Her eyes looked really great. No signs of hypoxia at all,13 and though she previously had one or two new corneal vessels about which we had been concerned, these looked to be much improved. In fact, there seemed to be rather less hyperemia than what we typically expect to see with soft lens wearers, especially around the limbus.14 Looks like that was an oxygen-related phenomenon all along...who knew?
2011
It was a bit of a slow burn to start, but silicone hydrogels have really taken off. Right now, about half of our contact lens wearers are using them, and almost all of them are in daily wear. Unfortunately, it seems that increased oxygen didn’t really reduce the rates of microbial keratitis for extended wearers,15 so we’ve been strongly recommending that our patients don’t sleep in their lenses at all.
We still like to be able to avoid any hypoxia issues whenever possible, so we have been using a lot of silicone hydrogels for daily wear. There were one or two problems in the early days because the first-generation materials had relatively high elastic moduli and were stiffer compared to regular hydrogels.16 That caused discomfort issues for some people as well as the occasional corneal problem (e.g., superior arcuate lesions).17 Fortunately, manufacturers were quick to realize the potential for these materials in daily wear and brought out second-generation products with much lower moduli. Unfortunately, it seems that not all of these newer materials work well with all of the lens care systems available right now.
Mark’s experience is a case in point. He’s using silicone hydrogel, daily wear lenses on a monthly replacement schedule; while he is largely asymptomatic, his corneas were showing a lot of diffuse, punctate, epithelial staining (Figure 6). It seemed to be an interaction with one of the components of the disinfecting solution that he is using,18 so he’ll need to switch to an alternative care system. Fortunately, there are quite a few alternatives available, with a range of different bactericidal agents. So, it shouldn’t be too hard to fix the problem.

2021
Remember Peter? We saw his granddaughter today. She wears daily disposable, silicone hydrogel toric lenses. It’s amazing that even though she has only 0.75DC, we can confidently correct it without worrying about significant lens-to-lens variation, despite her needing hundreds of lenses every year. Manufacturing methods have improved massively, and reproducible mass production of lenses in more or less any design is pretty standard in both hydrogel and silicone hydrogel materials. That means that we can offer the option of daily disposability to the majority of our patients, whether they are simple myopes, hyperopes, astigmats, or presbyopes. We find that this optimizes wearing comfort19 and compliance, because no cleaning or storage solutions are involved, and complications are reduced. That’s especially useful for the growing number of children we are seeing who use lenses to control the progression of their myopia.
Overall clinical performance is generally excellent, and many wearers experience comfort and vision that is comparable with those who have no need for vision correction at all.20 On the downside, we do worry about the environmental impact of so many pieces of plastic going into the trash every day, and we take steps to educate all of our patients about ways to minimize the problem.21 Fortunately, packaging design has also moved forward significantly, otherwise we wouldn’t have enough space to store all of the lenses that we supply.
Of course, the daily disposable route isn’t for everyone. We still have many people who replace lenses less frequently for one reason or another, and they are happy doing so. The range of materials and designs available for this group is equally impressive, so they certainly don’t lose out.
Naturally, we still have problems occasionally.22 End-of-day discomfort continues to be a nuisance for some. And while we no longer recommend overnight wear, contact lenses remain a risk factor for corneal infection.23 A truly great bifocal wouldn’t be a bad thing either. Still, soft lenses have made incredible progress over the last half century, and there aren’t too many people in need of vision correction to whom we can’t offer something these days.
Looking ahead, maybe the next 50 years will be even more spectacular. We already know that soft lenses can be used to continuously monitor intraocular pressure, and we hear that they may be a central component in other biosensing applications as well as in virtual and augmented reality systems.24 Imagine how many new wearers that would create! This should keep us busy for a while. CLS
The Office gratefully acknowledges the many practitioners, supporting staff, and patients who have passed within its walls and provided this unique perspective.
REFERENCES
- Wichterle O, Lim D. Hydrophilic gels for biological use. Nature. 1960;185:177.
- Pearson RM. A review of the limitations of the first hydrogel contact lenses. Clin Exp Optom. 2010 Jan;93:15-25.
- Inn HD. The Griffin lens. Am J Optom Arch Am Acad Optom. 1973 Dec;50:977-983.
- Josephson JE. A report on the refitting of successful Griffin Naturalens wearers with Bausch & Lomb Soflens™ contact lenses (polymacon). Am J Optom Arch Am Acad Optom. 1973 May;50:416-422.
- Epstein AB, Remba MJ. Hydrogel toric contact lens correction. In Bennett ES, Weissman BA, eds. Clinical Contact Lens Practice, 2nd ed. Philadelphia: Lippincott Williams & Wilkins. 2005:515-530.
- Barr J. History and development of contact lenses. In Bennett ES, Weissman BA, eds. Contact Lens Clinical Practice, 2nd ed. Philadelphia: Lippincott Williams & Wilkins. 2005:9.
- Charman WN, Walsh G. Retinal image quality with different designs of bifocal contact lens. Cont Lens Anterior Eye. 1986 Jan;9:13-19.
- Lamb J, Bowden T. Contact lens history and material development. In Phillips AJ, Speedwell L, eds. Contact Lenses, 6th ed. Edinburgh: Elsevier. 2019:2-17.
- Nilsson SEG, Söderqvist M. Clinical performance of a daily disposable contact lens: a 3-month prospective study. J British Contact Lens Assoc. 1995;18(3):81-86.
- Holden BA, Sweeney DF, Seger RG. Epithelial erosions caused by thin high water content lenses. Clin Exp Optom. 1986 May;69:103-107.
- Orsborn GN, Zantos SG. Corneal desiccation staining with thin high water content contact lenses. CLAO J. 1988 Apr-Jun;14:81-85.
- Refojo MF, Leong FL. Water pervaporation through silicone rubber contact lenses: A possible cause of complications. Contact Intraocul Lens Med J. 1981 Jul-Sep;7:226-233.
- Covey M, Sweeney DF, Terry R, Sankaridurg PR, Holden BA. Hypoxic effects on the anterior eye of high-Dk soft contact lens wearers are negligible. Optom Vis Sci. 2001 Feb;78:95-99.
- Papas EB, Vajdic CM, Austen R, Holden BA. High-oxygen-transmissibility soft contact lenses do not induce limbal hyperaemia. Curr Eye Res. 1997 Sep;16:942-948.
- Stapleton F, Keay L, Edwards K, Holden B. The epidemiology of microbial keratitis with silicone hydrogel contact lenses. Eye Contact Lens. 2013 Jan;39:79-85.
- Tighe BJ. A decade of silicone hydrogel development: Surface properties, mechanical properties, and ocular compatibility. Eye Contact Lens. 2013 Jan;39:4-12.
- Holden BA, Stephenson A, Stretton S, et al. Superior epithelial arcuate lesions with soft contact lens wear. Optom Vis Sci. 2001 Jan;78:9-12.
- Khan TF, Price BL, Morgan PB, Maldonado-Codina C, Dobson CB. Cellular fluorescein hyperfluorescence is dynamin-dependent and increased by Tetronic 1107 treatment. Int J Biochem Cell Biol. 2018 Aug;101:54-63.
- Lazon de la Jara P, Papas E, Diec J, Naduvilath T, Willcox MD, Holden BA. Effect of lens care systems on the clinical performance of a contact lens. Optom Vis Sci. 2013 Apr;90:344-350.
- Lazon de la Jara P, Diec J, Naduvilath T, Papas EB. Measuring daily disposable contact lenses against non-wearer benchmarks. Optom Vis Sci. 2018 Dec;95:1088-1095.
- Smith SL, Orsborn GN, Sulley A, Chatterjee NB, Morgan PB. An investigation into disposal and recycling options for daily disposable and monthly replacement soft contact lens modalities. Cont Lens Anterior Eye. 2021 Mar 12;101435.
- Stapleton F, Bakkar M, Carnt N, et al. CLEAR - Contact lens complications. Cont Lens Anterior Eye. 2021 Apr;44:330-367.
- Szczotka-Flynn LB, Shovlin JP, Schnider CM, et al. American Academy of Optometry Microbial Keratitis Think Tank. Optom Vis Sci. 2021 Mar 1;98:182-198.
- Papas EB. Contact lens technology to 2020 and beyond: a review of recent patent literature. Clin Exp Optom. 2017 Sep;100:529-536.




