The information for this annual report is derived from the most recent literature and from Contact Lens Spectrum reader surveys as well as from prominent leaders in the contact lens industry. Recent developments with corneal GPs, sclerals, myopia, and custom soft lenses will be highlighted. In addition, new advancements in multifocals, keratoconus, and hybrid lenses will be presented.
GP LENSES
Overview of Trends According to recent market data from Contact Lens Spectrum, GP lens fits and refits in the United States remain steady relative to recent years,1 comprising about one in nine fits and refits (i.e., 9% GP and 2% hybrid). Data provided by Robert W. Baird & Co. (Jeff Johnson, OD, CFA, managing director, senior research analyst) indicate that—exclusive of scleral lenses and overnight orthokeratology, both of which are exhibiting growth—conventional spherical GPs have exhibited a modest single-digit decline in growth, with a total market of about $140 million.
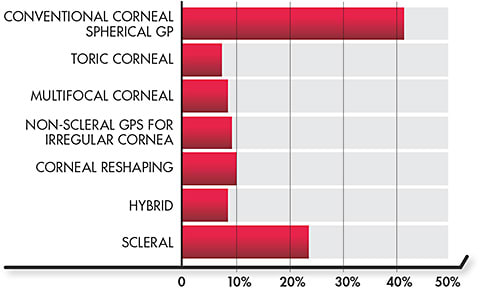
Figure 1 shows results from Contact Lens Spectrum’s recent GP Prescribing Survey. When asked what percentage of each of seven GP lens categories they prescribe, conventional corneal GPs still lead at slightly greater than 40%, with sclerals at 23% and the other categories (toric, multifocal, non-scleral for irregular cornea, corneal reshaping, and hybrid) all at ≤ 10%.
With the knowledge that GP manufacturing quality continues to improve—in addition to competing with soft lenses that are often provided directly from inventory and that provide the benefit of good initial vision—empirical fitting of GPs is becoming more popular. The GP Prescribing Survey asked the readership about the preferred method of fitting—empirical or diagnostic—for seven categories of lenses (Table 1). Not surprisingly, almost four out of five eyecare professionals (ECPs) prefer empirically fitting toric and multifocal GPs, and conventional spherical lenses are not far behind. In fact, there was an increased trend in empirical fitting in every category but one (corneal reshaping) as compared to last year; the biggest increase occurred with hybrid lenses (55% versus 44% in 2020).2 It is predicted that the increasing availability and use of scleral profilometry instrumentation will result in a significant increase in empirical fitting of sclerals in the next few years.
| TYPE OF DESIGN | EMPIRICAL (%) | DIAGNOSTIC (%) |
| Toric | 79 | 21 |
| Multifocal | 78 | 22 |
| Spherical | 73 | 27 |
| Hybrid | 55 | 46 |
| Corneal Reshaping | 50 | 50 |
| Non-Scleral Irregular Cornea GP | 30 | 70 |
| Scleral | 10 | 90 |
Developments in the Last Year Members of the GP Lens Institute (GPLI) Advisory Board were surveyed for their opinions on what were the most important developments in GP lenses in the past 12 months. The top seven responses (in decreasing order) are listed in “Most Important GP Developments in the Past Year” on page 22. It is important to note that advancements in scleral lens technology and applications accounted for most of these developments including the one most cited: the increasing availability of hyper-Dk lens materials. The introduction of a monthly treatment process to restore a polyethylene glycol (PEG)-based coating was also noted, because it helps maintain the surface wettability of a PEG-coated lens. Likewise, there was excitement at the announcement in May that an overnight orthokeratology lens was approved by the U.S. Food and Drug Administration (FDA) for the management of myopia. This was the result of a collaboration between two contact lens companies, and these lenses are expected to be available by the end of 2021. Other notable answers included extended depth of focus (EDOF) designs and increased empirical fitting of hybrid lenses.
Scleral Lenses The use of scleral lenses continues to increase, and they are becoming a mainstream correction device in both irregular cornea and ocular surface disease (OSD) patients. Contact Lens Spectrum market research indicates that—across all designs, soft and GP—scleral lenses represent 4% of all fits and refits, up from 3% last year and equal to corneal GPs.1 The results of the survey also showed that, overall, in the last 12 months, scleral lens use has increased slightly (Figure 2).

The benefits of scleral lenses are well noted in the literature, with entire issues devoted to covering them. Researchers have examined the impact of sclerals and how they can significantly improve the quality of life of individuals who have keratoconus. Of note, this has included functional improvements, especially for those exhibiting advanced stages of the disease.3 Sclerals can also significantly improve visual acuity and functioning.4 The benefits that they provide to OSD patients can be life-changing as well, and, in many cases, sclerals represent the only contact lens option for these individuals.
In a large retrospective study of 281 eyes fit into scleral lenses, 33.5% were fit for OSD management.5 This included 38 eyes that had severe dry eye/keratoconjunctivitis sicca, 18 eyes that had graft-versus-host disease, 15 eyes that had neurotrophic keratitis, and 11 eyes that had ocular cicatricial pemphigoid. Eighty-six percent of the eyes fit with scleral lenses for OSD responded well to therapy.
Likewise, sclerals have been found to reduce ocular aberrations and to improve visual acuity in patients who had post-laser-assisted in situ keratomileusis (LASIK) ectasia, keratoconus, and pellucid marginal degeneration6 while representing a safe and effective option for reducing higher-order aberrations (HOAs) associated with penetrating keratoplasty.7 One scleral advancement is the application of wavefront-guided optics to reduce aberrations and optimize quality of vision. These designs should have a greater presence on the market in the next few years.
Advancements in hyper-Dk lens materials have made scleral lenses a more attractive option, because they provide increased oxygen transmission. As noted earlier, this was considered one of the greatest advancements in GPs in the last 12 months. Research notes that increasing the Dk of a scleral lens material from 100Dk to 200Dk resulted in a 12% reduction in edema. In general, a minimum Dk of 125 is recommended.8
Overall, scleral lenses exhibit good clinical performance to date. In a retrospective study of 157 keratoconic eyes fit into scleral lenses, 9.6% of eyes experienced physiological adverse events including hydrops (3.2%), corneal infiltrative events (1.3%), corneal abrasion (1.3%), contact lens-induced acute red eye (1.3%), phlyctenulosis (0.6%), and microbial keratitis (0.6%).10 The jury still appears to be out regarding the impact of scleral lenses on intraocular pressure.
In addition, these patients can often benefit from a surface coating that can improve comfort, reduce dry eye symptoms, and reduce ocular surface compromise in scleral lens-wearing patients who have dry eye.9
Improvements in scleral lens design and, in particular, alignment with the sclera, are obtainable today via the increasing use of profilometry-driven design. Even in the absence of this instrumentation, being able to provide photos or video (which are easily captured via a cell phone adaptor to the slit lamp) to the laboratory is beneficial in helping consultants recognize whether a peripheral design modification is indicated.
MOST IMPORTANT GP DEVELOPMENTS IN THE PAST YEAR*
- Increasing availability of hyper-Dk lens materials.
- Advancements in scleral lens technology (i.e., improved applications of asymmetry and/or better control over segments of the lens to improve limbal and landing relationships).
- The introduction of a conditioning solution to resurface polyethylene glycol (PEG)-coated lenses.
- The increased use of profilometry to design scleral lenses to assist in creating highly customized lenses to improve vision, fit, and comfort.
- Advancements in orthokeratology lens design, including more customizable designs and increasing applications of toric designs.
- The U.S. Food and Drug Administration’s approval of an overnight orthokeratology lens for the management of myopia.
- Introduction of smaller scleral lenses that address residual higher-order aberrations.
*Based on responses from the GPLI Advisory Board
The readership was surveyed as to what percentage of their scleral lenses were fit using a spherical (versus toric) periphery, and the results were essentially equal (Table 2). Toric haptics will likely be predominant in the future. Likewise, quadrant-specific designs are increasing in use. One study reported that the use of a data-driven, quadrant-specific design resulted in visual improvement, less need for midday removal, and an average of only two lenses needed for the fitting process.11
| TYPE OF DESIGN | 10% | 20% | 30% | 40% | 50% | 60% | 70% | 80% | 90% | 100% | N/A |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Spherical Peripheral Curves | 14 | 6 | 3 | 3 | 8 | 2 | 5 | 7 | 9 | 6 | 36 |
| Toric Haptics | 11 | 8 | 3 | 3 | 8 | 3 | 3 | 6 | 11 | 6 | 37 |
Keratoconus As mentioned in the previous section, the benefits of scleral lenses for keratoconus patients can be significant. Sclerals have also become a preferred modality in the fitting of those afflicted with this disease. In fact, in recent years, scleral lenses have become the most popular modality, according to respondents.
Making the assumption that the “go-to” lens is the one they fit to, at minimum, 50% of their keratoconus patients, scleral lenses are fit approximately 2.5 times more compared to the next highest modality (i.e., corneal GP lenses).
That said, it is a blessing to have all of these tools available when managing these often-challenging patients. One tool that is now available throughout the United States is a genetic eye test that helps practitioners determine a patient’s risk of keratoconus as well as the presence of other corneal dystrophies.
Recent research has confirmed that multiple tools are beneficial in the management of keratoconus. When comparing corneal and scleral GP lens wear in patients who have corneal ectasia, significantly better comfort was achieved with scleral lenses.12 However, both modalities were successful, and there was no visual advantage to refitting successful corneal lens wearers into sclerals and vice versa. A retrospective review of patients who have keratoconus and who had been fit into hybrids in one or both eyes indicated that the new-generation hybrid lenses are a safe and appropriate option that provide very good visual outcomes.13 However, a dropout rate of 37.8%—primarily in sagging, more peripheral, cones—can limit success with this modality.
Multifocals As in previous years, survey responses indicate a strong preference for aspheric GP multifocals as the “go-to” lenses (i.e., ≥ 50% of GP multifocal fits); they account for as much as the next four categories combined (i.e., segmented translating GP, scleral, concentric, and hybrid).
Much recent interest pertains to decentering the optics to allow the optical center of the lens to align with the pupil center. This was also noted by many of the survey respondents as an important innovation, especially with scleral lenses that tend to decenter inferior-temporally. A recent study examined scleral lenses ordered with a 2.5mm center-near zone that was decentered consistent with the position of the lens assessed during a diagnostic fitting.14 The researchers found that the average decentration was 1.75mm and that 77% of eyes achieved distance vision within one line of their best-corrected acuity.
Hybrids Empirical fitting of hybrid lenses is both recommended by the manufacturer and increasing as a preferred method of fitting by ECPs. At the 2021 virtual Global Specialty Lens Symposium, one company introduced a lens that specifically promotes an empirical fitting approach. The linear silicone hydrogel (SiHy) soft skirt of the lens follows the linear shape of the sclera, and the landing is based on the sagittal depth depending on the horizontal visible iris diameter. Its multifocal lens is powered by a proprietary EDOF design that combines HOAs to elongate patients’ depth of focus for potentially clearer vision at near, intermediate, and distance.
Lens Care As noted earlier, the introduction of a conditioning solution to restore the PEG layer on the front surface of treated lenses was a major advancement in 2021. This is a five-step monthly process to be performed by patients. It is a prescription-only product that can be sold directly by ECPs or via participating contact lens laboratories.
The evolution toward scleral lens filling solutions that mimic the ionic composition of the tears continues to occur. One such solution recently introduced to the market improved subjective ratings of scleral lens wearers and may reduce the incidence of midday fogging.15
The issue of tap water use with GP lenses continues to be addressed. Although the FDA, the Centers for Disease Control and Prevention (CDC), and the American Optometric Association (AOA) all indicate that tap water should not be used for rinsing or storing GP lenses, a recent survey completed by 272 clinicians, vision scientists, and industry personnel indicated that more than one-half (57.4%) reported rinsing lenses with tap water.16 Noncompliance with recommended care was also evident in the results from our readership poll, as no less than 15% of those ECPs answering with regard to their “go-to” filling solution for scleral lenses responded with “preserved wetting/conditioning solution” (Figure 3). Therefore, our educational efforts on care and compliance need to increase.

CUSTOM SOFT LENSES NOW AND IN THE FUTURE
WHAT HAS BEEN THE MOST IMPORTANT RECENT DEVELOPMENT IN CUSTOM SOFT LENSES? WHERE DO YOU SEE CUSTOM SOFT LENSES HAVING THE MOST IMPACT IN THE NEXT TWO-TO-THREE YEARS?
“Better vision through [higher-order aberration (HOA)] application in custom soft lenses. Custom soft designs for myopia management. In fact, all lenses potentially should be custom designed, as each eye is so different in terms of peripheral vision and HOA, etc. And more use of soft specialty lenses for challenging eyes.” –Eef van der Worp, PhD, BSc
“Ability to correct higher and more exact astigmatic prescriptions, including irregular astigmatism and HOAs.” –Gloria Chiu, OD
“Decentered multifocal optics are the most important recent development. Custom soft lenses will reign supreme until standard lenses can accurately be decentered.” –John Gelles, OD
“The ability to create soft lenses with a more robust range of sagittal values. This includes ‘normal’ eyes that just do not fit into the available parameters of stock lens offerings; a greater range of ametropia can be addressed, small and large corneas can be better fit, etc.” –Ken Maller, OD
“Drug delivery and health monitoring.” –Louise Sclafani, OD
“The availability of custom high-toric powers for monthly replacement and improvements in computer-generated prosthetics.” –Greg DeNaeyer, OD
“Toric multifocal lenses are becoming important in light of myopia management. Custom design will help to calibrate add power and treatment zone diameter.” –Langis Michaud, OD, MSc
“Radical new soft lens designs for lens rotational stability and lens translation.” –Steve Byrnes, OD
“Several things top the the list. High-quality custom multifocal torics and a stock multifocal toric are game changers. This allows private practitioners to add specialty contact lenses with no additional startup cost to their practices.” –Dan Fuller, OD
“The future introduction of high-Dk materials in custom soft [contact lenses] and continued development of designs to address irregular corneas in these materials potentially can have a significant impact.” –Barry Eiden, OD
MYOPIA
Based on our readership survey, the survey of the GPLI Advisory Board, and the introduction of programs such as the Global Myopia Symposium (GMS), it is evident that myopia management is the hottest topic of 2021. Greater awareness of the long-term complications of myopia, notably high myopia, has resulted in extensive research pertaining to (primarily) contact lens, pharmaceutical, and combination treatments headed by the most prolific researchers in myopia management.
It has been reported that the benefits of a myopia control program far exceed the risks, as a reduction of just 1.00D in myopic refractive error can have a significant effect on future impairment, and the risk of loss of vision is quite remote.17 As for preferred modality of myopia control, when asked which method(s) they use in practice, the readership showed a preference toward soft multifocals (57%) versus corneal reshaping/orthokeratology (43%), atropine (35%), and bifocal spectacles (26%) (Figure 4).

Orthokeratology The current interest in myopia management has resulted in an increased interest in incorporating orthokeratology into clinical practice as well as resulted in the introduction—or forthcoming introduction—of several lens designs. When asked about the use of corneal reshaping/overnight orthokeratology lens designs (if applicable) in the past 12 months, the greatest response was “Increased Slightly,” with only two respondents indicating that this had decreased in their clinical practice (Figure 5). In addition, a number of lens designs have been or will soon be introduced in the United States and/or in Europe.

Benefits One study looked at Chinese children undergoing orthokeratology. As compared to single-vision spectacles, the study reported that orthokeratology may induce some ocular discomfort with lens wear during the night, but overall this was surpassed by the benefit of better vision-related quality of life.18 Researchers also noted that orthokeratology was a viable alternative for adult symptomatic soft lens wearers, with a success rate of 72.5%.19 Although most subjects were unfamiliar with orthokeratology prior to the study, they were able to quickly adapt to the treatment and were likely to recommend orthokeratology to others.19
Safety Several recent studies have resulted in the conclusion that orthokeratology is a safe modality for myopia management.20-22 The rate of microbial keratitis is similar to that associated with the use of daily wear soft contact lenses.21 The results of a comprehensive one-year study concluded that orthokeratology is a safe option for children who have myopia; younger age, higher myopia, and a history of allergic conjunctivitis were risk factors for adverse events.22
Orthokeratology and Atropine Several studies have evaluated the use of low-dose atropine, either in combination with orthokeratology or in comparison to it. In one study that compared orthokeratology to 0.02% atropine, orthokeratology appeared to be a better method for slowing axial length elongation.23 In another study, combining 0.01% atropine with orthokeratology was not significant in changing the three-year axial elongation outcome as compared to orthokeratology monotherapy.24 However, a meta-analysis, including a total of five combination studies of orthokeratology with low-dose atropine, concluded that the combined effect may be superior to that of orthokeratology alone.25
Soft Multifocals The FDA approval of a daily disposable lens to slow the progression of myopia in young people in November 2019 has had a large ripple effect in looking at this and other soft multifocal lens designs to evaluate their effectiveness—alone or in combination with low-dose atropine—as well as what would be the optimum add power for these lenses to significantly slow myopia progression without a significant effect on a young person’s quality of vision.
A two-year study reported on the impact on myopia of a bifocal defocus-inducing soft lens.26 After two years, signs of myopia progression stabilization in 72% to 73.5% of subjects and a statistically significant reduction of 87% to 88% in axial elongation were also observed.
Additionally, the long-awaited and highly anticipated results of the Bifocal Lenses in Nearsighted Kids (BLINK) study were recently published.27 In this multi-center three-year study, 294 children, aged 7-to-11 years, who had –0.75D to –5.00D of myopia, were randomly assigned to wear single-vision soft, medium-add (+1.50D)soft multifocals, or high-add (+2.50D) soft multifocals. The study demonstrated that treatment with the high-add multifocals was more effective in reducing the rate of myopia progression compared to with a low-add lens. Therefore, as the single-vision wearers experienced fewer than two letters of better low-contrast visual acuity compared to those in both multifocal groups, a high add power is recommended for optimal control of myopia.
Comparison Studies In a 12-month study comparing orthokeratology to multifocal contact lenses, orthokeratology-induced elongation and associated relative corneal refractive power shift were significantly smaller than that for multifocal contact lenses.28 Likewise, another review analyzed the literature and found that orthokeratology is the modality with the longest track record of high (defined as approximately 50%) effectiveness, and it also has a more robust amount of supporting evidence.29
Coding and Billing With the rapid onset of interest in fitting these modalities for myopia control, it becomes imperative to appropriately code to get properly reimbursed. An entire webinar on this topic is available at https://www.gpli.info/webinar-2020-09-b .
As children often have degenerative myopia in both eyes, the diagnostic code to use in controlling myopia would be “Degenerative myopia, bilateral” (H42.23).30,31 Another recommendation is to use the “unlisted ophthalmological service or procedure” code (92499) for the services associated with myopia management.31
Myopia Resources There are a growing number of organizations and symposia that focus exclusively on myopia management. GMS, which was recently held from Sept. 16 to 19, included an education content partnership with the Asia Optometric Congress. These sessions can be viewed on-demand at www.gmsymposium.com . The American Academy of Orthokeratology and Myopia Control has an annual meeting (Vision By Design) and a Fellowship program. The Myopia Profile resources for ECPs and patients (www.myopiaprofile.com ) are also very useful. Finally, comprehensive contemporary myopia management articles17,32 are definitely worth reading.
CUSTOM SOFT LENSES
While there have not been many new developments in custom soft lenses in the past year, the future of custom soft lenses is exciting. Each year, the manufacturing of these lenses becomes more sophisticated, and that bodes well going forward. Traditionally, custom soft lenses have been important for patients who either did not have an optimal fit with a standard lens or whose required power and/or axis was outside of the standard range.33 The fact that these lenses can be manufactured in essentially any spherical power, any cylinder power, and cylinder axes in 1º increments is a testament to how precisely these lenses can be lathe-cut. The ability to do so in a SiHy lens material is very beneficial as well.
More recently, advances have been made in the area of multifocal corrections. Initially, the ability to custom manufacture—and to continually expand parameters including add powers—and to refine lenses for astigmatic presbyopes has been very beneficial. Some manufacturers are now able to customize the sizes of the near and distance zones to factor in pupil size as well as vision demands. Likewise, some manufacturers can now decenter the optics so that the geometric center of the lens aligns optimally with a patient’s line of sight.
Custom soft lenses are expanding as a viable option for irregular cornea patients. Steeper base curve radii to better align with keratoconic corneas as well as the greater thickness needed for astigmatic correction and stability have been important breakthroughs. Again, these designs can be manufactured in a SiHy material—important with the center thicknesses often employed—and represent a viable option in mild cases of keratoconus as well as in some post-surgical cases. Aberration control is another potential benefit of these designs, and one recent report pertained to a keratoconus design with decentered optics (i.e., the optical zone was decentered superiorly by 0.7mm) that resulted in an improvement in correction of coma aberrations and on-eye optical centration.34 In addition, custom soft lenses should be considered in some cases in which scleral lenses are not successful due to factors such as a poor fitting relationship, patient dissatisfaction with handling, or lens-induced hypoxia.
THE FUTURE OF MYOPIA MANAGEMENT
WHEN ASKED ABOUT THE FUTURE OF MYOPIA MANAGEMENT, JEFF WALLINE, OD, PHD, HAD THE FOLLOWING THOUGHTS:
“Myopia management for a child may begin even before the future onset of myopia in that child. We can pretty accurately predict which children will become myopic simply by measuring their cycloplegic refractive error. That may enable us to apply treatment prior to the onset of myopia. Because the period of greatest eye growth is prior to the onset of myopia, we may be able to better affect the amount of myopia experienced in adulthood by providing myopia control prior to the onset of myopia. For example, we may be able to prescribe eye drops to delay the onset of myopia and eventually to make a patient less myopic in adulthood.”
Of course, custom soft tinted lenses can be invaluable in providing cosmesis for disfigured or blind eyes, and they help functionally for those who have color blindness, diplopia, or photophobia. One large retrospective study of 109 patients who had either unilateral blindness or any one of the three aforementioned eye function problems reported that 94.5% of patients were satisfied following the application of tinted soft lenses.35
THE FUTURE
The future of GP and custom soft lenses is exciting, especially in the areas of scleral design and myopia. Several soft lens designs—typically multifocals—are currently commonly used as an off-label application for myopia management; this will significantly increase in the next few years as information about progressive myopia becomes more mainstream to consumers and ECPs alike and as it grows as a public health concern (see “The Future of Myopia Management”). Likewise, new orthokeratology designs will continue to be introduced and, like soft multifocals, will continue to have a greater effect on axial length and myopia progression.
Custom soft lens innovations to expect soon would include more designs incorporating decentered optics for greater optical alignment in multifocal lenses, the introduction of an innovative translating soft multifocal design, increased application of aberration-control optics, introduction of horizontal prism to correct horizontal binocular problems, and innovations in manufacturing of custom lenses, notably for the correction of irregular corneas. In the long-term, look for lenses that provide drug delivery, including for management of allergies, dry eye, and glaucoma (see “Custom Soft Lenses Now and in the Future” on page 23).
Advancements in sclerals will include continuing introductions of wavefront optics to decrease HOAs, decentered multifocal optics for better optical alignment resulting in improved vision, and increased profilometry-driven designs that enable empirical fitting, improved scleral alignment, and first-fit success. Scleral lenses will increase in use as a mainstream corrective option for those suffering from dry eye disease. Long-term applications should include the incorporation of artificial intelligence and biometric data. Certainly, augmented reality lenses are on the horizon, and smart presbyopia lenses may not be far behind (see “Future Advancements in GP Lenses,” for additional comments about this from leaders in specialty lenses). CLS
FUTURE ADVANCEMENTS IN GP LENSES
WHAT DO YOU THINK WILL BE THE MOST IMPORTANT DEVELOPMENT IN THE NEXT 12-TO-38 MONTHS IN GP LENSES?
“The continued development of myopia management designs will slowly drive up the number of GP contact lens fittings.” –David Seibel, OD
“The addition of more comfortable materials, lenses with better optics (e.g., wavefront optics); and more customization options for scleral lenses.” –Matt Kauffman, OD
“[In the short term:] Labs adopting scanning technologies in the manufacture of corneal lenses for irregular corneas. [In the long term:] Incorporation of artificial intelligence and biometric data.” –Tom Arnold, OD
“Better understanding of the environment created under a scleral lens (e.g., oxygen transfer, corneal impact, causes and resolution to midday fogging, etc.).” –Ken Maller, OD
“More customized options in scleral and multifocal contact lens designs and new lens materials to enhance their surface for improved comfort and vision quality.” –Brian Silverman, OD
“Wave error-correcting scleral lenses, decentration of optical centers over the visual axis and oval lens diameters/optical zones to match cornea shapes.” –Dan Fuller, OD
“Increasing attention toward profilometry and data-driven contact lens fitting. This applies not only to more custom freeform scleral lens designs, but to new corneal reshaping designs and other GP designs as well. I believe this trend will make it apparent that technology will increasingly perform contact lens fitting.” –Brian Chou, OD
“A multifocal GP lens that works for all stages of presbyopia that is easy to fit. An orthokeratology lens that centers well on oblique astigmatic eyes. A corneal scleral profiler that is consistent and as good as diagnostic fitting.” –Melanie Frogozo, OD
“The use of simplified topography/tomography-guided lens design programs will make GP lenses more ubiquitous.” –John Gelles, OD
“GP lenses that slowly release medication or artificial tears in the eyes. GP lenses that monitor blood sugar and IOP throughout the day.” –Roxanne Achong-Coan, OD
“I believe that OSD could surpass keratoconus as the primary indication for scleral lenses. Increased awareness and experience with scleral lenses will be the drivers to fill the unmet needs for patients with moderate to severe OSD who have failed with traditional medical management and are underserved.” –Greg DeNaeyer, OD
“I see it growing in the area of myopia control, orthokeratology, new materials have made it to the market and wouldn’t be surprised if there’s continued innovation here, as well as more customization capabilities with scleral lenses.” –Karen Carrasquillo, OD, PhD
“I think corneo-scleral topography will become more readily available in many offices and designing corneal GPs and scleral lenses will become even easier.” –Stephanie Woo, OD
Acknowledgements: Roxanne Achong-Coan, OD; Tiffany Andrzejewski, OD; Mile Brujic, OD; Steve Byrnes, OD; Karen Carrasquillo, OD, PhD; Gloria Chiu, OD; Brian Chou, OD; Robert L. Davis, OD; Greg DeNaeyer, OD; Barry Eiden, OD; Melanie Frogozo, OD; Dan Fuller, OD; John Gelles, OD; Jennifer Harthan, OD; Jeff Johnson, OD (Robert W. Baird); Matt Kauffman, OD; Elise Kramer, OD; Derek Louie, OD; Ken Maller, OD; Langis Michaud, OD; Clarke Newman, OD; Louise Sclafani, OD; David Seibel, OD; Brian Silverman, OD; Jeff Sonsino, OD; Eef van der Worp, PhD, BSc; Cheri Vincent-Reimer, OD; and Stephanie Woo, OD.
REFERENCES
- Nichols JJ, Fisher D. Contact Lenses 2020. Contact Lens Spectrum. 2021 Jan;36:24-29,51.
- Bennett ES. GP Annual Report 2020. Contact Lens Spectrum. 2020 Oct;35:28-30,32,34,36,37,59.
- Baudin F, Chemaly A, Arnould L, et al. Quality-of-Life Improvement After Scleral Lens Fitting in Patients With Keratoconus. Eye Contact Lens. 2021 Sep 1;47:520-525.
- Kreps EO, Pesudovs K, Claerhout I, Koppen C. Mini-Scleral Lenses Improve Vision-Related Quality of Life in Keratoconus. Cornea. 2021 Jul 1;40:859-864.
- Severinsky B. Therapeutic scleral lenses: From vision to ocular surface rehabilitation. Presented at the (virtual) Global Specialty Lens Symposium, January 2021.
- Kumar M, Shetty R, Lalgudi VG, Khamar P, Vincent SJ, Atchison DA. The effect of scleral lenses on vision, refraction and aberrations in post-LASIK ectasia, keratoconus and pellucid marginal degeneration. Ophthalmic Physiol Opt. 2021 Jul;41:664-672.
- Penbe A, Kanar HS, Simsek S. Efficiency and Safety of Scleral Lenses in Rehabilitation of Refractive Errors and High Order Aberrations After Penetrating Keratoplasty. Eye Contact Lens. 2021 May 1;47:301-307.
- Dhallu SK, Huarte ST, Bilkhu PS, Boychev N, Wolffsohn JS. Effect of Scleral Lens Oxygen Permeability on Corneal Physiology. Optom Vis Sci. 2020 Sep;97:669-675.
- Mickles CV, Harthan JS, Barnett M. Assessment of a novel surface treatment for scleral lens wearers with dry eye. Eye Contact Lens. 2021 May 1;47:308-313.
- Fuller D, Wang Y. Safety and efficacy of scleral lenses for keratoconus. Optom Vis Sci. 2020 Sep;97:741-748.
- Barnett M, Carrasquillo KG, Schornack MM. Clinical Outcomes of Scleral Lens Fitting with a Data-driven, Quadrant-specific Design: Multicenter Review. Optom Vis Sci. 2020 Sep;97:761-765.
- Levit A, Benwell M, Evans BJW. Randomised controlled trial of corneal vs. scleral rigid gas permeable contact lenses for keratoconus and other ectatic corneal disorders. Cont Lens Anterior Eye. 2020 Dec;43:543-552.
- Kloeck D, Koppen C, Kreps EO. Clinical Outcome of Hybrid Contact Lenses in Keratoconus. Eye Contact Lens. 2021 May 1;47:283-287.
- Gidosh N. Multifocal off-center optics visual effectiveness study (MOOVES): 2nd year update. Presented at the (virtual) Global Specialty Lens Symposium, January 2021.
- Fogt JS, Karres M, Barr JT. Changes in the symptoms of midday fogging with a novel scleral contact lens filling solution. Optom Vis Sci. 2020 Sep;97:690-696.
- Steele KR, Wagner H, Lai N, Zimmerman A. Gas-permeable contact lenses and water exposure: Practices and perceptions. Optom Vis Sci. 2021 Mar 1;98:258-265.
- Bullimore MA, Ritchey ER, Shah S, Leveziel N, Bourne RRA, Flitcroft DI. The Risks and Benefits of Myopia Control. Ophthalmology. 2021 May 4;S0161-6420(21)00326-2.
- Yang B, Ma X, Liu L, Cho P. Vision-related quality of life of Chinese children undergoing orthokeratology treatment compared to single vision spectacles. Cont Lens Anterior Eye. 2021 Aug;44:101350.
- Duong K, Pucker AD, McGwin G Jr., Franklin QX, Cox J. Established soft contact lens wearers’ awareness of and initial experiences with orthokeratology. Ophthalmic Physiol Opt. 2021 Jul;41:673-682.
- Goto T, Shiraishi A, Ohashi Y, et al. A multicenter clinical trial of orthokeratology in school-aged children and adolescents in Japan. Jpn J Ophthalmol. 2021 Sep;65:624-631.
- Bullimore MA, Mirsayafov DS, Khurai AR, et al. Pediatric microbial keratitis with overnight orthokeratology in Russia. Eye Contact Lens. 2021 Jul 1;47:420-425.
- Hu P, Zhao Y, Chen, D, Ni H. The safety of orthokeratology in myopic children and analysis of related factors. Cont Lens Anterior Eye. 2021 Feb;44:89-93.
- Lyu Y, Ji N, Fu A-C, et al. Comparison of administration of 0.02% Atropine and Orthokeratology for myopia control. Eye Contact Lens. 2021 Feb 1;47:81-85.
- Chen Z, Zhou J, Xue F, Qu X, Zhou X. Two-year add-on effect of using low concentration atropine in poor responders of orthokeratology in myopic children. Br J Ophthalmol. 2021 Mar 11;bjophthalmol-2020-317980. [Online ahead of print]
- Gao C, Wan S, Zhang Y, Han J. The efficacy of Atropine combined with orthokeratology in slowing axial elongation of myopic children: A meta-analysis. Eye Contact Lens. 2021 Feb 1;47:98-103.
- Avetisov SE, Myagkov AV, Egorova AV, Poskrebysheva ZN, Zhabina AO. [Results of a two-year clinical study of myopia control with bifocal defocus-inducing soft contact lenses] [Article in Russian] Vestn Oftalmol. 2021;137(3):5-12.
- Walline JJ, Walker MK, Mutti DO, et al. Effect of High Add Power, Medium Add Power, or Single-Vision Contact Lenses on Myopia Progression in Children: The BLINK Randomized Clinical Trial. JAMA. 2020 Aug 11;324:571-580.
- Jiang F, Huang X, Xia H, et al. The Spatial Distribution of Relative Corneal Refractive Power Shift and Axial Growth in Myopic Children: Orthokeratology Versus Multifocal Contact Lens. Front Neurosci. 2021 Jun 9;15:686932.
- van der Worp E, Gifford K, Polling JR, Read S. Customizing the treatment of the myopic child. Presented at the (virtual) Global Specialty Lens Symposium, January 2021.
- Flitcroft DI, He M, Jonas JB, et al. IMI – Defining and Classifying Myopia: A Proposed Set of Standards for Clinical and Epidemiologic Studies. Invest Ophthalmol Vis Sci. 2019 Feb 28;60:M20-M30.
- Newman CD. Coding and Billing for Myopia Management. Contact Lens Spectrum. 2020 Dec;35:48.
- Walline JJ. Myopia Control in 2021. Contact Lens Spectrum. 2021 Mar;36: 24-26,28.
- Messer B. Customizing with Confidence. Contact Lens Spectrum. 2021 June;36:26-28,30,31.
- Suzaki A, Koh S, Maeda N, et al. Optimizing correction of coma aberration in keratoconus with a novel soft contact. Cont Lens Anterior Eye. 2021 Aug;44:101405.
- de Paula Yoneda P, Schellini SA, Padovani CR, Silva VF. Use of soft contact lens for esthetic and functional rehabilitation. Eye Contact Lens. 2021 Jul 1;47:383-387.




