In my June 2021 column, I discussed empirical fitting of hybrid lenses on corneas that have above-average sagittal heights. Corneas that have diameters above 12mm limit the performance of off-the-shelf toric contact lenses, resulting in suboptimal quality of vision when they are worn due to inadequate fit. Hybrid contact lenses allow for correction of clinically significant astigmatism in these patients with their stable, GP-generated optics.
Traditionally, hybrid lenses that are commercially available in North America allow for gross modifications of the soft skirt to best fit the underlying cornea. Flat 2, Flat, Medium, Steep, and Steep 2 (rarely used) skirts are familiar choices to hybrid lens fitters. The skirt is covalently bonded to the GP center and is designed to allow tear flow under the lens when worn. The steeper the skirt, the greater the likelihood of lens seal-off on eye, which will result in a stagnation of tears under the lens, lens decentration, and corneal staining or molding.
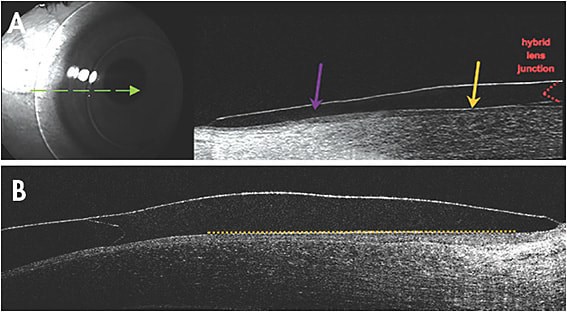
Modern-day hybrid lenses can be empirically designed, and skirt parameters are derived from corneal diameter; larger horizontal visible iris diameters (HVIDs) typically require a tighter-fitting lens to center on eye. Instead of only three main skirt curves (Flat 2 8.7mm, Flat 8.4mm, and Medium 8.1mm), the newest hybrid lenses can now be manufactured to better align with the known linear slope of the scleral profile (van der Worp, 2010) (Figure 1). Instead of radii of curvature defining the fit of the hybrid soft skirt, a linear angle is selected based on corneal size.
Case Example
A 16-year-old female who had –1.50D of corneal cylinder OD and OS was fit with a custom, empirically ordered hybrid lens. Her large HVIDs (12.5mm OD and OS) would traditionally call for a Medium (8.1mm) skirt to minimize the chances of inferior lens decentration. The first dispensed lenses were well-centered, with acceptable movement observed from the edge of the soft skirt. Visual outcomes were far superior to any soft toric lens that she had tried in the past.
At the one-week follow-up, the left lens showed a noticeable decrease in lens movement and inferior decentration after a four-hour-wear-time slit lamp evaluation (Figure 2, video available below). The patient also reported intermittent peripheral blur. Ironically, she was not aware of the left lens on eye at all as compared to the right lens that still had minimal movement on eye and excellent centration. A skirt parameter change of the left lens from 47 to 45 improved centration and increased movement of the lens on eye due to the looser fit. While the patient was initially more aware of this modified lens, the awareness diminished after a week of wear. Vision remained stable throughout the day.

Be mindful of “I don’t feel the lens at all” patient commentary, as these patients may still require modifications to their fit. CLS
For references, please visit www.clspectrum.com/references and click on document #311.




