An orthokeratology (ortho-k) practice begins with the motivation to make a difference in patients’ lives, as their vision directly affects their quality of life. In the past, ortho-k was used primarily to obviate the need to wear myopia-correcting lenses during the day. While that was transformative for many adults, ortho-k promises much more today.
Modern ortho-k can correct other types of refractive errors such as astigmatism and hyperopia, and it is also a tool for addressing the myopia epidemic with its potential to slow the progression of myopia. Reducing the need for corrective lenses is beneficial, but preventing high myopia and its ocular complications is arguably more important. What follows is a discussion of the history of ortho-k and its transformation into modern ortho-k practice.
ORTHO-K DESIGNS THEN AND NOW
During the International Society of Contact Lens Specialists meeting in 1962, contact lens pioneer George Jessen, OD, introduced the concept of “orthofocus,” which was the first deliberate attempt to mold the cornea to reduce myopia. At this meeting, Newton Wesley, OD, MD, ScD, PhD, termed this method orthokeratology. Jessen’s method consisted of fitting a conventional-design polymethyl methacrylate (PMMA) corneal lens flatter than K by the amount of necessary myopia correction, with an additional overcorrection (about 1.00D). This overcorrection, or Jessen factor, compensates for myopia regression toward the end of the day.
As PMMA does not transmit oxygen, the lenses were fit flat to deliver more oxygen to the cornea. Lenses fit in this manner were originally thought to compress the underlying corneal tissue. We now know that this process redistributes the corneal epithelium rather than causing overall corneal flattening. Myopic patients did, however, experience improved uncorrected vision for a period of time after lens wear was discontinued.1 Early attempts at ortho-k, while safe, were plagued by unpredictable refractive outcomes and minimal myopia correction (1.00D, on average), and it would take months to achieve the target treatment goal.2,3
More on the history and evolution of orthokeratology is included in the sidebar to the right.
Modern ortho-k employs reverse-geometry GP lenses. A reverse-geometry lens has a flat central curve and an adjacent reverse curve that is steeper compared to the central radius. This reverse curve is connected to flatter peripheral curves that align with the midperipheral cornea. The modern design centers well and is highly stable, allowing for rapid and predictable correction of higher amounts of myopia and even of other types of refractive errors (Figure 1).4,5
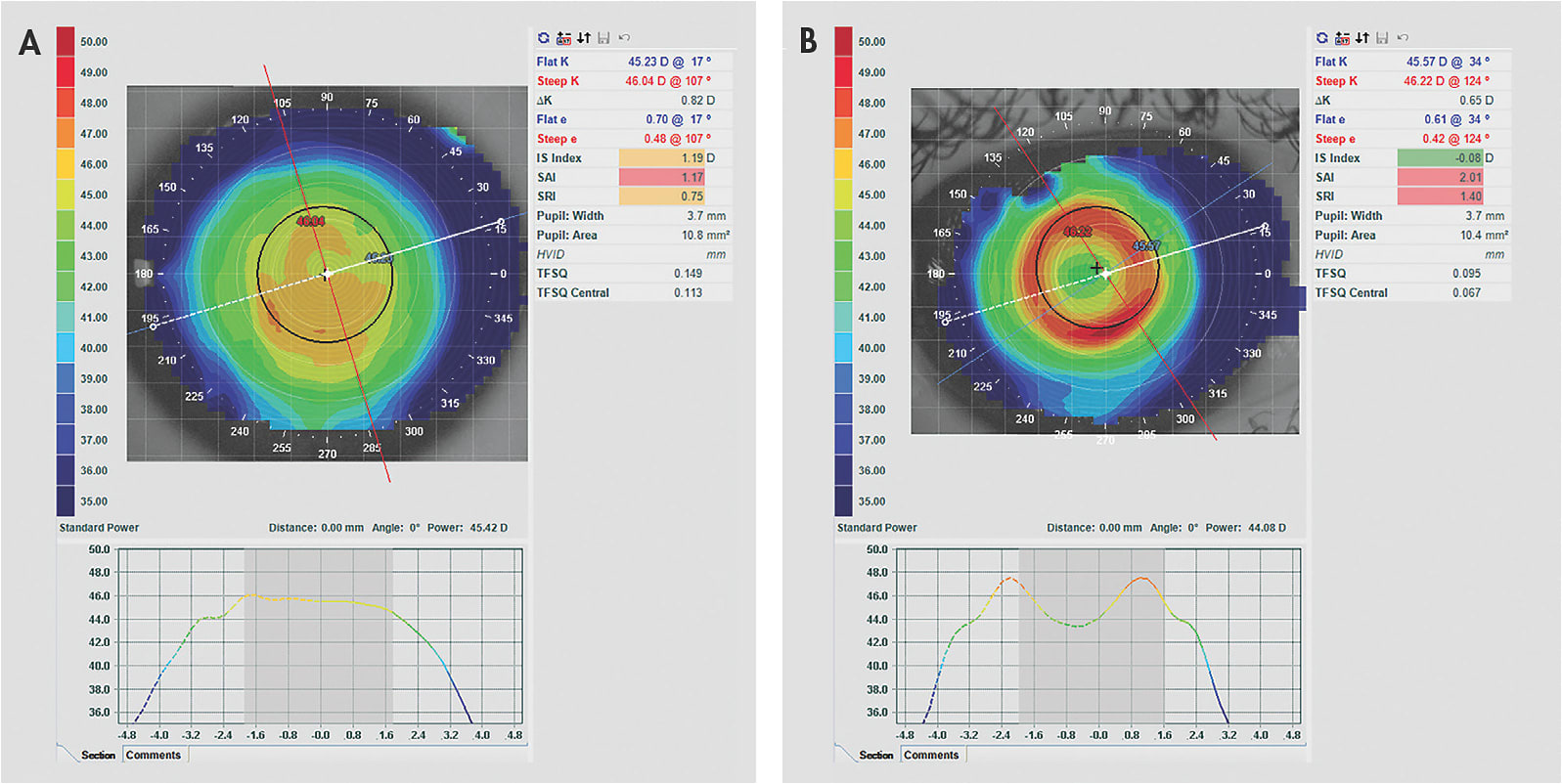
The use of GP materials enables overnight wear of ortho-k lenses in a closed-eye state, which adds to the convenience and comfort of this procedure. The use of corneal topography to guide the treatment further differentiates the modern practice of ortho-k (Figure 2). Corneal topographers can map a large area of the cornea, providing an accurate and complete view of the pre- and post-treatment curvatures. These data are crucial for troubleshooting problems with suboptimal designs.
MECHANISMS OF CORNEAL SHAPE CHANGE WITH MODERN ORTHO-K
Early on in ortho-k practice, it was thought that the cornea molded to the back surface of the contact lens because of pressure applied by the eyelid during blinking to the contact lens, which in turn exerted pressure on the corneal apex. This was the basis for Jessen’s orthofocus technique, in which lenses were fitted flatter than the corneal curvature by the dioptric amount of the targeted myopic refractive error. The goal of this fitting technique was to select the lens base curve to match the desired curvature of the reshaped cornea.
Later, Tabb developed the “hydraulic” theory of ortho-k, suggesting that fluid forces in the post-lens tear film were responsible for inducing the corneal shape change.6 This theory also assumed that corneal tissue response to ortho-k involved an overall bending and consequential flattening of the cornea. There remained a disconnect, however, between keratometry readings and refractive error changes after ortho-k, suggesting that this was not the case and that other changes must also be occurring elsewhere in the eye.7
Swarbrick, Wong, and O’Leary were the first to suggest that the changes in ortho-k were not from corneal bending.8 They postulated that central corneal epithelial thinning and midperipheral thickening—possibly of epithelial and stromal origin—were responsible for the daytime-wear ortho-k effect. Since then, central epithelial thinning has been confirmed in clinical studies in overnight ortho-k.8-10
The cause of the epithelial thinning after ortho-k lens wear is not well understood. Histological evidence from Choo et al in cat models indicates that the epithelial response in the central cornea is cellular compression of intracellular fluid toward the midperiphery rather than actual loss or movement of cells (Figure 3).9 Currently, the corneal shape changes in ortho-k are thought to be a combination of central epithelial thinning and midperipheral epithelial and stromal thickening.8,10 While current data indicate that ortho-k is safe, further work is needed to examine long-term effects on the health of the cornea in closed-eye ortho-k lens wear.

OVERNIGHT ORTHOKERATOLOGY: A HISTORY OF PROGRESS | Cary M. Herzberg, OD
It has been a momentous last decade for corneal reshaping, with startling growth brought on by new acceptance of the procedure both here in the United States and worldwide, particularly due to the discovery that it has the potential to slow the progression of myopia in children and teens. In the beginning, however, there were many more reasons to believe that the specialty that we call ortho-k was the least likely to lead to an optical defocus model that—when employed in a timely and effective manner—could potentially reduce the frequency of high myopia.25
Setting the Stage for Rapid Growth in the Modern Era
From its discovery in 1960 by Stuart Grant, OD, through decades of stunted growth, the process of reshaping the cornea through ortho-k grew slowly, mainly because it remained outside of the eyecare mainstream. Topography and higher-Dk materials were on the horizon but would have to wait another decade for full implementation. Efforts to increase the awareness of ortho-k were compromised by the lack of academic research and by the smallness of the community that practiced it.
The modern era of ortho-k began with the U.S. Food and Drug Administration approval of the first corneal reshaping device in 2002.26 This approval came with no age limit, which would be incredibly important when all eyes turned to myopia management in the next decade. Academic research during the first decade fol-lowing this approval demonstrated the safety and efficacy of the procedure; more importantly, included in the research was early data demonstrating ortho-k’s effectiveness at managing myopia progression.21,27-29
Advancements in diamond lathes, technology including next-generation topographers, and new higher-Dk fluorosilicone acrylate materials set the stage for the rapid development highlighted in the next decade. Yet the success of ortho-k would ultimately depend on eyecare professional (ECP) acceptance and implementation. The industry that at first rallied around the new device after its approval pulled back, worried that most ECPs would never fully invest in or even attempt corneal reshaping. The answer to this challenge rested on the ability to educate both clinicians and the public that they served. More substantial growth would have to wait for the right circumstances—which unfortunately turned out to be the rapid growth of myopia evolving into a worldwide epidemic.
As myopia has continued to escalate worldwide15 and its long-term ramifications have become better understood,17,18 the need to slow its progression in children and teens has increasingly taken center stage. Ortho-k’s proven ability to do just that19-23 has fueled the modality’s growth and offers practitioners an opportunity to help these children in a way that differentiates them from most standard eyecare practices. Today, there is no shortage of resources available to help practitioners incorporate ortho-k into their practices. Once certified, practitioners can seek advice, information, and assistance from ortho-k lens manufacturers and their consultants as well as from various organizations, forums, and continuing education events and conferences. There’s never been a better time to get started.
MODERN LENS DESIGN IN ORTHO-K FOR MYOPIA
Modern ortho-k lenses have a reverse-geometry design and a larger diameter, often 90% to 95% of the total horizontal visible iris diameter (HVID). The back surface of the lens has a minimum of four curves; however, some designs that correct higher amounts of myopia can have up to six curves. The primary measurements needed to empirically order these lenses include a manifest refraction, HVID, and corneal topography. Some lenses are designed from flat keratometry (flat K) measurements, while custom lenses designed with software incorporate additional measurements such as eccentricity and apical radius of curvature.
The next section describes in detail each of the major curves in a myopia ortho-k lens from the center of the lens toward the periphery.
Base Curve (BC)/Back Optic Zone Radius (BOZR) The BC is the central-most curve. The corresponding anatomical diameter is typically between 5.0mm and 5.8mm, with an average diameter of 5.4mm. For adults who have large pupils, the diameter can be increased. This curve will create the treatment zone on post-fitting topography. The BC/BOZR is chosen based on the amount of corneal flattening desired and is related to the corneal curvature and to the amount of myopia treatment required.
Many designs incorporate a Jessen factor, ranging from 0.50D up to greater than 3.00D flatter than K. This additional correction to the targeted amount of myopia ensures that the desired treatment amount is achieved and that patients maintain satisfactory uncorrected vision throughout the entire day.11,12
In empirical designs, the central BC is typically spherical; however, an aspheric radius can be incorporated instead to increase the amount of midperipheral clearance. An aspheric BC not only allows for higher amounts of myopia to be treated, it also creates greater peripheral myopic defocus to slow the progression of myopia when needed. Because designs that aim to treat lower degrees of myopia have wider treatment zones, inducing an adequate amount of peripheral defocus within a patient’s visual axis to slow myopia progression is a concern. In designs that target lower degrees of myopia, an aspheric BC can be used to increase the amount of midperipheral clearance, thereby creating more peripheral myopic defocus for effective myopia management.11,12
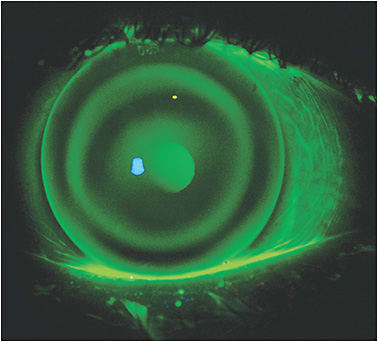
The desired amount of apical clearance under this curve is commonly 5µm to 10µm.11,12 This is worth noting, as it is less than the 20µm needed to perceive fluorescein behind a contact lens. When observing the BOZR, therefore, it can falsely appear as an apical-bearing fluorescein pattern.13
Reverse Curve The reverse curve joins the BC to the relief/alignment curve and is steeper compared to its neighboring curves. This curve is typically 0.3mm to 1.0mm wide, and the amount of clearance over the cornea depends on the amount of myopia being corrected. Lower amounts of myopia correction will result in a shallower reservoir in comparison to higher amounts of myopia correction. The clearance under this curve is commonly referred to as the tear film reservoir and is important for creating optimum forces to properly mold the cornea and exert the myopia-control effect.
One of the primary functions of the reverse curve is to raise or lower the BC to create appropriate central clearance. Increasing or decreasing the sagittal depth of the lens through steepening or flattening the reverse curve may be necessary to achieve proper treatment.11,12
Relief Curve An additional relief curve may be incorporated to encourage epithelial changes from the alignment zone toward the tear film reservoir. This may allow for more effective treatment of higher degrees of myopia. When present, the relief zone is 0.2mm to 0.4mm wide, with a clearance of 1µm to 6µm.11,12
Alignment Zone The alignment zone is critical for properly centering the ortho-k lens on the eye. This is the zone in which the lens lands on the eye, and alignment beneath this area is desired. The width of this zone comprises 30% of the total lens diameter, and its shape is determined by the amount of eccentricity present along the flat meridian of the midperipheral cornea. Individuals who have lower corneal eccentricity will have steeper alignment curves, and those who have higher corneal eccentricity will have flatter alignment curves.11,12
Peripheral Zone(s) In the periphery of ortho-k lenses, up to two curves can be incorporated next to the alignment curve to create edge lift at the peripheral cornea. The secondary zone has a width of 0.2mm to 0.5mm and a depth of about 20µm. This curve is not included in all lens designs. The function of the secondary zone is simply to link the alignment and peripheral curves. The peripheral curve also has a width of 0.2mm to 0.5mm, and its depth is usually between 80µm and 100µm.11,12
MODERN ORTHO-K DESIGNS FOR OTHER REFRACTIVE ERRORS
Although correction of myopia is the primary indication for ortho-k, correction of other refractive errors is achievable with alternate lens designs and fitting philosophies. Ortho-k for hyperopia creates central steepening by gently reshaping the midperipheral cornea (Figure 4). Regular astigmatism is correctable through designs that offer back-toric curves. Additionally, newer ortho-k designs also allow for manipulation of various back-surface curves and zones, allowing correction of refractive error for patients who have undergone laser-assisted in situ keratomileusis (LASIK) (Figure 5).

SOFTWARE-DRIVEN DESIGNS
Ortho-k design software linked to corneal topography is also available when a high degree of customizability is desired. This enables practitioners to customize curves to optimize additional factors such as tear layer thickness for improved refractive error treatment and myopia control (Figure 6).

CORNEOSCLERAL ORTHO-K
In the past decade, scleral lenses have increased in popularity for fitting both normal and diseased eyes. The larger-diameter design offers patients improved comfort, lens stability, and vision. Interestingly, both scleral lenses and modern ortho-k lenses feature a landing/alignment zone that is functional for centering and stabilizing these lenses. Because of these unique fitting characteristics, improved fit using corneoscleral lens designs in ortho-k has been utilized.14
Because of their increased size, corneoscleral ortho-k designs may offer better centration and stability compared to corneal lenses, particularly when treating challenging refractive errors such as high corneal astigmatism (> 1.75D), against-the-rule and oblique astigmatism, high myopia in cases of smaller corneal diameter, irregular astigmatism, and cases in which the cylinder component is higher compared to the spherical component (Figure 7).

MYOPIA CONTROL
Researchers have estimated that one-half of the global population will be myopic by 205015 if management strategies are not effectively employed. Myopia is being diagnosed in many countries at increasingly younger ages,16 and when children develop myopia at a younger age, it progresses more quickly and to higher amounts. Those who have high myopia (more than 6.00D) are at heightened risk of developing vision-threatening pathology. For example, people who have 6.00D of myopia have a 14.4 times greater likelihood of developing glaucoma and a 3.3 times greater likelihood of developing posterior subcapsular cataracts.17 Those who have 8.00D or more of myopia have a 7.8 times greater risk of retinal detachment. For patients who have pathologic myopia, approximately 26% older than 70 years of age had best-corrected vision worse than 20/200.18 Myopia has serious vision implications and is not merely a minor inconvenience requiring eyeglasses or contact lenses. Myopia is a disease process that carries significant risk of vision-threatening disease.17
Because children are at greater risk for developing high myopia, it is important to prevent myopia progression as early as possible. Preventing high myopia by slowing the progression of myopia offers a solution. Ortho-k and other contact lens-based interventions aim to create a peripheral defocus retinal cue that slows myopia progression. Ortho-k slows the growth of the eye and provides effective myopia control.19 In myopia ortho-k correction, the central refractive error is corrected while leaving peripheral myopic blur. This blur is thought to act as the stimulus that slows the progression of myopia.20
In May 2021, the U.S. Food and Drug Administration approved the first ortho-k lens for the management of myopia. Myopia management with ortho-k can reduce myopia progression by approximately 50% compared to spectacle correction alone.19,21-23.
The Ethical Case for Ortho-k and Myopia Management Myopia of any degree is a condition worthy of medical intervention, as it is not a consequence-free deviation of normal physiology. While simply correcting refractive error carries risks and costs, myopia’s effects are more insidious than just optically correctable blurred vision. Myopia is a pathological disease process with consequences that can make it impossible to achieve adequate best-corrected visual acuity and may lead to permanent visual impairment.
Treatments to limit the progression of myopia are available, and their existence in the presence of a myopia epidemic makes it imperative for eyecare professionals to prescribe them to all appropriate children. Current myopia management treatment options include soft multifocal lenses, ortho-k, and low-dose topical atropine. Providing myopia management to myopic children is the current standard of care.24 Myopia management naturally fits into the practice of providers who offer primary eye care, and it should be offered to as many children as possible.
THE BUSINESS CASE FOR ORTHO-K
To provide ortho-k and myopia management effectively, practitioners must build their expertise. Exceptional professional skills enable profitability. Ortho-k also requires substantial investments in materials, technology, training, people (staff), infrastructure, and operations. With ortho-k, your skill is the product, and it must be spectacular.
One benefit of ortho-k is its flexibility to incorporate into and to grow your practice; that is, ortho-k is considered an unspecified ophthalmological service, and as such, it is not covered by medical insurance and should be paid by the patients. Likewise, no vision care plans cover ortho-k. Primary eyecare providers are ideally positioned to provide myopia management and ortho-k treatments, and they should seize the opportunity while it exists to differentiate themselves and to grow their practices.
SUMMARY
The introduction of ortho-k techniques in the early 1960s was bold and prescient. Today, ortho-k offers visual solutions for many patient types, ranging from adults looking to eschew daytime spectacles and contact lenses to children needing myopia control. Advances in lens design, supported by underlying research into the mechanisms of the ortho-k effect, have enabled eyecare practitioners to safely address many more of our patients’ needs. Concomitant with the expanding research findings and potential applications is an enlarged body of knowledge that must be mastered to successfully implement ortho-k in our practices. The rewards are more than worth the effort, particularly as ortho-k remains firmly in the domain of primary eyecare practitioners. CLS
REFERENCES
- Jessen G. Orthofocus techniques. Contacto. 1962;6:5.
- Polse KA, Brand RJ, Keener RJ, Schwalbe JS, Vastine DW. The Berkeley Orthokeratology Study, part III: safety. Am J Optom Physiol Opt. 1983 Apr;60:321-328.
- Polse KA, Brand RJ, Schwalbe JS, Vastine DW, Keener RJ. The Berkeley Orthokeratology Study, Part II: Efficacy and duration. Am J Optom Physiol Opt. 1983 Mar;60:187-198.
- Mountford J. An analysis of the changes in corneal shape and refractive error induced by accelerated orthokeratology. Int Contact Lens Clin. 1997 Jul;24:128-144.
- Nichols JJ, Marsich MM, Nguyen M, Barr JT, Bullimore MA. Overnight orthokeratology. Optom Vis Sci. 2000 May;77:252-259.
- Coon LJ. Orthokeratology. Part II: Evaluating the Tabb method. J Am Optom Assoc. 1984 Jun;55:409-418.
- Swarbrick HA. Orthokeratology review and update. Clin Exp Optom. 2006 May;89:124-143.
- Swarbrick HA, Wong G, O’Leary DJ. Corneal response to orthokeratology. Optom Vis Sci. 1998 Nov;75:791-799.
- Choo JD, Caroline PJ, Harlin DD, Papas EB, Holden BA. Morphologic changes in cat epithelium following continuous wear of orthokeratology lenses: a pilot study. Cont Lens Anterior Eye. 2008 Feb;31:29-37.
- Alharbi A, Swarbrick HA. The effects of overnight orthokeratology lens wear on corneal thickness. Invest Ophthalmol Vis Sci. 2003 Jun;44:2518-2523.
- Mountford J, Ruston D, Dave T. Orthokeratology: Principles and Practice. Butterworth-Heinemann; 2004.
- Korszen E, Caroline PJ. The Anatomy of a Modern Orthokeratology Lens. Contact Lens Spectrum. 2017 Mar;32:30-32,34,35,40.
- Young G. The effect of rigid lens design on fluorescein fit. Cont Lens Anterior Eye. 1998;21(2):41-46.
- Fadel D, Herzberg C. Is Ortho-K Possible With Corneo-Scleral lenses? Contact Lens Spectrum. 2016 Dec;31:48-50.
- Holden BA, Fricke TR, Wilson DA, et al. Global Prevalence of Myopia and High Myopia and Temporal Trends from 2000 through 2050. Ophthalmology. 2016 May;123:1036-1042.
- Holden BA, Jong M, Davis S, Wilson D, Fricke T, Resnikoff S. Nearly 1 billion myopes at risk of myopia-related sight-threatening conditions by 2050 – time to act now. Clin Exp Optom. 2015 Nov;98:491-493.
- Flitcroft DI. The complex interactions of retinal, optical and environmental factors in myopia aetiology. Prog Retin Eye Res. 2012 Nov;31:622-660.
- Cho BJ, Shin JY, Yu HG. Complications of Pathologic Myopia. Eye Contact Lens. 2016 Jan;42:9-15.
- Walline JJ. Myopia Control: A Review. Eye Contact Lens. 2016 Jan;42:3-8.
- Smith EL, Hung LF, Huang J, Arumugam B. Effects of local myopic defocus on refractive development in monkeys. Optom Vis Sci. 2013 Nov;90:1176-1186.
- Cho P, Cheung SW, Edwards M. The longitudinal orthokeratology research in children (LORIC) in Hong Kong: a pilot study on refractive changes and myopic control. Curr Eye Res. 2005 Jan;30:71-80.
- Cho P, Cheung SW. Retardation of myopia in Orthokeratology (ROMIO) study: a 2-year randomized clinical trial. Invest Ophthalmol Vis Sci. 2012 Oct;53:7077-7085.
- Santodomingo-Rubido J, Villa-Collar C, Gilmartin B, Gutiérrez-Ortega R. Myopia control with orthokeratology contact lenses in Spain: refractive and biometric changes. Invest Ophthalmol Vis Sci. 2012 Jul;53:5060-5065.
- World Council of Optometry. Resolution: The Standard of Care for Myopia Management by Optometrists. 2021. Available at https://worldcouncilofoptometry.info/resolution-the-standard-of-care-for-myopia-management-by-optometrists . Accessed Aug. 30, 2021.
- Herzberg C. An Update on Orthokeratology. Contact Lens Spectrum. 2010 Mar;25:22-24,26-31.
- U.S. Food & Drug Administration. Premarket Approval, Paragon CRT. 2002 Jun. Available at http://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfpma/pma.cfm?id=P870024S043 . Accessed Sept. 8, 2021.
- Reim TR, Lund M, Wu R. Orthokeratology and Adolescent Myopia Control. Contact Lens Spectrum. 2003 Mar;18:40-42.
- Walline JJ, Jones LA, Sinnott LT. Corneal reshaping and myopia progression. Br J Ophthalmol. 2009 Sep;93:1181-1185.
- Eiden SB, Davis RL, Bennett ES, DeKinder JO. The Smart Study: Background, Rationale, and Baseline Results. Contact Lens Spectrum. 2009 Oct;24:24-28,30,31.




