The argument of diagnostic fitting versus empirical design of corneal GP lenses has raged for many years, but with ongoing advancements in diagnostic technology, empirical design is now undeniably easy and effective. With careful patient selection and data collection and a reputable GP lens laboratory, nearly any GP lens can be designed to fit accurately and to provide excellent vision with the first lens ordered, particularly on regular corneas.
We All Love to Save Time
Patients appreciate efficiencies that limit their time in the office. Multiple diagnostic lens attempts are not only time consuming, they can also be messy and confusing, and they require extensive staff time for lens cleaning and storage. With many eyecare practices scheduling patients at 15- or 20-minute intervals, the cost of taking up valuable chair time with diagnostic fittings can be difficult to justify. Additionally, even with careful efforts to minimize pathogen contamination and spread, trialing numerous contact lenses in-office can lead to unnecessary exposures.
New wearers can be provided with application, removal, and care education prior to their first lens dispense appointment to reduce in-office training time. An excellent resource for this is available at www.contactlenses.org/care-and-handling.htm . When patients are prepared and can confidently apply and remove a lens that provides better vision immediately, success with GPs is limited only by their ability to tolerate the adaptation period.
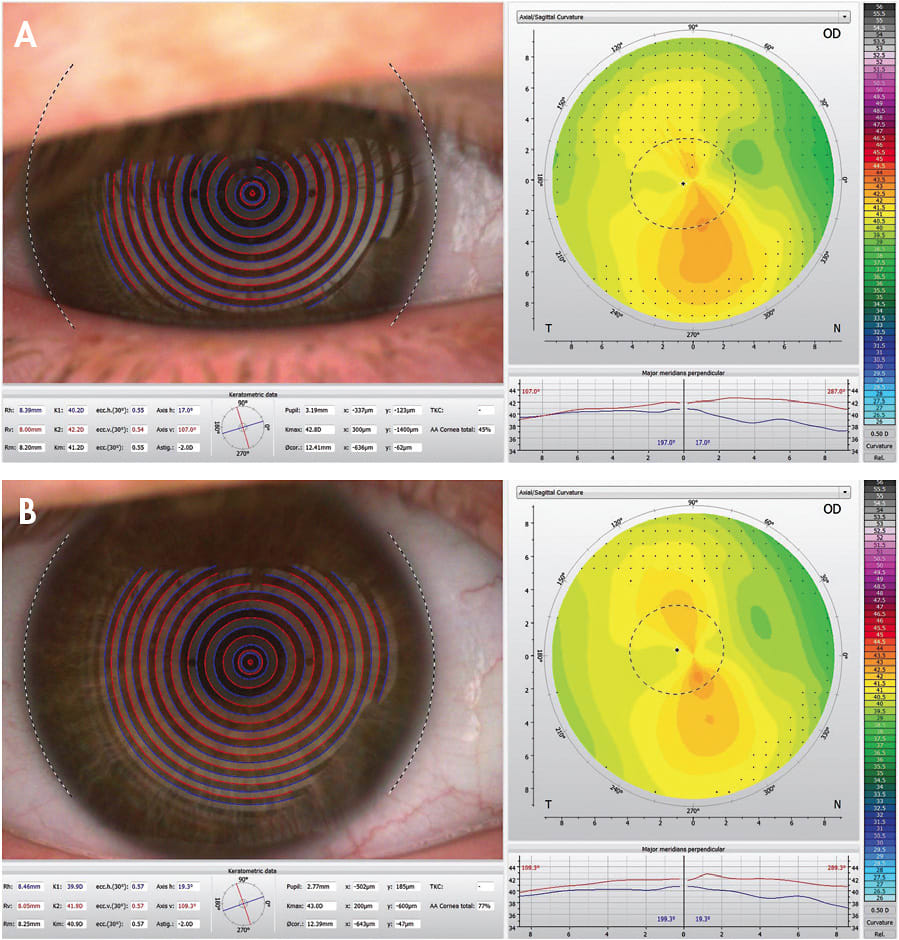
A careful manifest refraction will allow for accurate power calculations; minimizing power adjustments with over-refraction will provide better vision on the initial lens dispense. Getting high-quality, reliable keratometry or topography with clear mires, good centration, and minimal lid interference (Figure 1) helps in base curve selection. Instilling artificial tears prior to obtaining these measurements can assist in getting the best data possible, and handheld devices may help improve corneal view and image capture by assisting in holding eyelids out of the way. Inexpensive mascara “guards” or “shields” for this purpose are easily obtained online.
For GP multifocals, determine eye dominance, pupil size, and lower lid position (for translating designs) to make empirical design even easier. Though not always necessary, notes on upper lid positioning and any excessive laxity may help predict centration issues.
Sending topography images electronically to laboratory consultants provides an appreciated abundance of information for design purposes, but first determine which method of electronic communication is the most secure. Additionally, many topographers now include GP lens fitting software that can assist with design and can show simulated/predicted fluorescein patterns prior to lens ordering.
Success with the first corneal GP ordered is not uncommon. Obtaining good initial data is critical, but the time and frustration saved makes the effort worthwhile. CLS




