Recent advances in scleral lens (SL) technologies such as profilometry and impression-based SL design are impressive and have improved the lives of countless patients globally. Phorometry, which dates back to the early 1900s, continues to be the main method of measuring the refractive error of individual eyes (Campbell, 2008).
Unsurprisingly, “20/20 unhappy” patients with seemingly impeccable SLs continue to report glare, haloes, starbursts, and double vision in our clinics. Rotationally asymmetric anterior and posterior corneal profile misalignment is the most common cause of optical aberrations in patients who have corneal ectasia (Tomidokoro et al, 2000; Chen and Yoon, 2008).
GP lenses and SLs partially mask anterior surface irregularities and correct lower-order aberrations and higher-order aberrations (HOAs) such as sphere and astigmatism by creating a new tear layer between the lens and cornea (Choi et al, 2007; Gumus et al, 2011). This optical system, however, is not perfect and residual HOAs within the ocular system can remain (Hastings et al, 2019). The next big wave in the SL world aims to wipe out residual HOA-related vision degradation: wavefront-guided scleral lenses (WFG-SL).
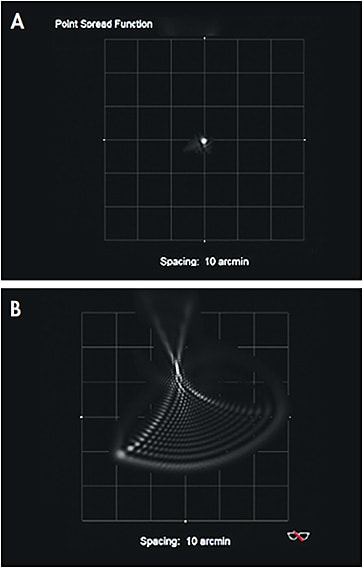
Aberrometers quantify the difference in ideal and measured wavefront; that difference is wavefront error (higher order aberrations). Imagine numerous light rays emitted from a single-point source entering the pupil. The course of these rays can be slowed and result in higher oscillations if an area of higher refractive index such as a corneal irregularity or cataract is encountered (Sepulveda and Krueger, 2003).
Commercially available wavefront aberrometers use a Hartmann-Shack sensor, dynamic sciascopy, or ray tracing technology to analyze the trajectory of individual light rays as it travels through the eye and reflects off the retina; otherwise known as a light ray’s optical path length (OPL) (Sepulveda and Krueger, 2003). Differences in OPLs among the infinite light rays result in optical aberrations and may cause the point light source to appear smeared or even doubled.
This smearing of vision was especially true for a 31-year-old male who had keratoconus and who presented to our clinic for a first-time eye exam (Figure 1). After achieving 20/20 distance visual acuities with conventional SLs, he continually reported debilitating diplopia, especially at night. Wavefront error mapping over his SLs revealed residual HOAs as the source of vision loss.
WFG-SLs target the residual optical aberrations that highly irregular eyes continue to experience despite conventional SL wear. The process of identifying patients who would benefit most from WFG-SLs begins with a conventional SL fitting. If poor visual quality persists despite optimizing SL power and fit, utilize an aberrometer and perform wavefront imaging after sufficient SL settling on a dilated eye to uncover residual HOAs present during SL wear.
Certain manufacturers may utilize the wavefront image to create a custom WFG-SL that targets these residual aberrations. Literature reports significant vision improvement with WFG-SLs (Hastings et al, 2019; Sabesan et al, 2013). A 71% reduction in higher-order root mean square wavefront error has been shown when comparing WFG-SLs to habitual correction whereas conventional SLs exhibit only a 48% reduction (Hastings et al, 2019).
Hopefully, as the future of optometry advances, wavefront imaging will become more accessible and wavefront-guided technology will become standard of care. CLS
References
- Campbell GL. Phoroptors, Early American Instruments of Refraction, and Those Who Used Them. Wheaton, IL: Gary L. Campbell, 2008.
- Tomidokoro A, Oshika T, Amano S, Higaki S, Maeda N, Miyata K. Changes in anterior and posterior corneal curvatures in keratoconus. Ophthalmology. 2000 Jul;107:1328-1332.
- Chen M, Yoon G. Posterior corneal aberrations and their compensation effects on anterior corneal aberrations in keratoconic eyes. Invest Ophthalmol Vis Sci. 2008 Dec;49:5645-5652.
- Choi J, Wee W, Lee J, Kim M. Changes of ocular higher order aberration in on-and off-eye of rigid gas permeable contact lenses. Optom Vis Sci. 2007 Jan;84:42-51.
- Gumus K, Gire A, Pflugfelder S. The impact of the Boston ocular surface prosthesis on wavefront higher-order aberrations. Am J Ophthalmol. 2011 Apr;151:682-690.
- Hastings GD, Applegate RA, Nguyen LC, Kauffman MJ, Hemmati RT, Marsack JD. Comparison of Wavefront-guided and Best Conventional Scleral Lenses after Habituation in Eyes with Corneal Ectasia. Optom Vis Sci. 2019 Apr;96:238-247.
- Sepulveda RN, Krueger R. Optical Aberrations and Wavefront Sensing. In Adler’s Physiology of the Eye: Clinical Application, Kaufman PL, Alm A, Adler FH, eds. St. Louis: Mosby. 2003:28-39.
- Sabesan R, Johns L, Tomashevskaya O, Jacobs DS, Rosenthal P, Yoon G. Wavefront-guided scleral lens prosthetic device for keratoconus. Optom Vis Sci. 2013 Apr;90:314-323.




