
History
A 54-year-old Hispanic female presented for a contact lens fitting. She had worn GPs all her life but was fit in soft contact lenses by an outside provider. The patient had a history of moderate astigmatism; due to limited soft toric multifocal options at the time, she was fit into monovision with soft torics. She did not mind the comfort of the soft contact lenses but was dissatisfied with the vision.
Exam Findings
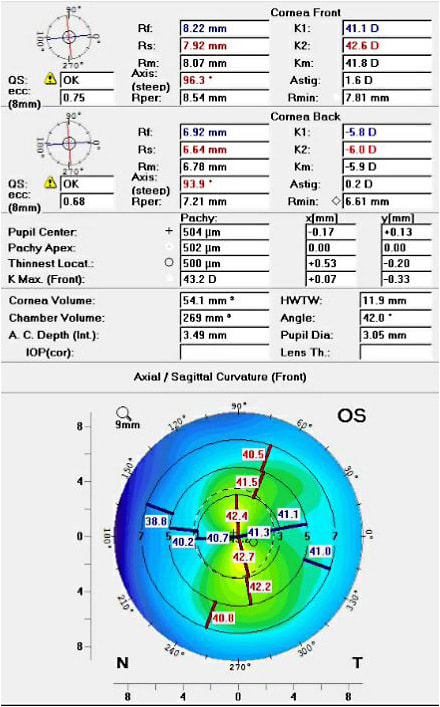
All entrance testing, vision, and slit lamp exams were unremarkable. Refraction was OD –2.00 –1.75 x 010 and OS –2.25 –1.50 x 179 (20/20 OD and OS). Topographies were taken for OD and OS (Figures 1 and 2). Initial GP multifocal (translating trifocal) lenses were ordered empirically based on the patient’s topography and refraction. Vision with the GP multifocals was 20/20 at distance, but slightly reduced to 20/30 at near. The patient noted that the blurry vision at near was more pronounced in the left eye. Figures 3 and 4 shows the initial trial lenses on each eye for OD and OS, respectively. Assessment of the OD lens revealed optimal fit with no rotation. The contact lens for the left eye was decentered inferiorly with minimal translation consistent with the patient’s complaints.


Discussion
Correcting patients for presbyopia can often be done with glasses, but visual performance may be superior with multifocal contact lenses.1 While soft contact lenses have grown in popularity due to comfort, disposability, and extended parameters, GPs can still offer patients superior vision. GPs are particularly beneficial for patients who have astigmatism and/or presbyopia.2 Providers fit soft contact lenses regularly due to their initial comfort and their ease of fitting. When discussing corrective options with patients, it is important to obtain a history of their contact lens wear, so that the provider knows which modalities have worked well and which ones to avoid.
The adaption period of GPs is one of the biggest hurdles for patients and providers, but typically occurs in the first 10 days of wear.3 As a general rule, if patients have happily worn GP lenses in the past, it is best to keep them in that modality. They are used to a certain quality of vision that may not be repeatable in soft contacts. Furthermore, if a patient is adapted to GPs, then comfort really isn’t something they will benefit from by switching to soft contact lenses.
When correcting for presbyopia, soft lenses offer spherical multifocals, monovision, and/or toric multifocals. Patients who have no or limited astigmatism do quite well with spherical multifocals. However, presbyopic patients with moderate or high astigmatism have limited options in soft contact lenses. There are more soft toric multifocals on the market today than ever before, but still very few commercial lenses exist. Monovision is a great modality for these patients, but many have complaints of adapting, reduced stereo vision, or glare at night while driving. GP multifocals maintain stereopsis and may offer superior vision for the presbyopic astigmatic patient. Table 1 shows a general comparison between soft and hard contact lenses, which can be beneficial to discuss with patients when deciding a modality.
| Advantages | Disadvantages | |
|---|---|---|
| Soft | Initial comfort Ease of fitting Easy to remove Not likely to dislodge |
Costly Limited parameters (reduced vision) Higher risk of infections Can be difficult to apply |
| GP | Affordable Custom parameters (crisp vision) Lowest risk of infections Easy to apply |
Adaption period More skill needed to fit Can be difficult to remove More movement/may dislodge |
For GPs, multifocal designs can be divided into aspheric and translating. Aspheric designs generally start with a distance power in the center of the lens and gradually transition to the near power at the edge of the lens.4 Translating designs consist of segmented powers of distance, intermediate, and/or near. They depend on the lower eyelid to push the lens superiorly to allow the patient to see through the different segmented powers.4 These lenses must be stabilized to avoid rotation such as using a prism ballasted or truncation design.
For our patient here in the translating multifocal, the upper edge of the intermediate segment should intersect the lower one-quarter of the pupil, while the lower edge of the intermediate segment should be at the lower edge of the pupil. We can see this optimal fit for OD, while OS shows inferior decentration. Changes were made to the OS lens to fit more superiorly, and acceptable vision was achieved. Not all GP multifocals may be fit in the same fashion and it is best to consult the fitting guide or manufacturer to ensure higher success rate/lower chair time.
Conclusion
Soft multifocals are a great option for most patients, however, those with astigmatism may not find their designs to be visually adequate. Patient motivation is one of the best predictors for success when converting a soft contact lens wearer to an GP. If someone is already happy in GPs, it is best to keep them in that modality and incorporate a multifocal rather than change to a soft lens modality. These patients are great candidates for the novice GP multifocal fitter and help the provider to become more familiar with lens options and troubleshooting.
References
- Fogt JS, Weisenberger K, Fogt N. Visual performance with multifocal contact lenses and progressive addition spectacles. Cont Lens Anterior Eye. 2021 May 25:101472.
- Fonn D, Gauthier CA, Pritchard N. Patient preferences and comparative ocular responses to rigid and soft contact lenses. Optom Vis Sci. 1995 Dec;72:857-863.
- Carracedo G, Martin-Gil A, Peixoto-de-Matos SC, Abejón-Gil P, Macedo-de-Araújo R, González-Méijome JM. Symptoms and Signs in Rigid Gas Permeable Lens Wearers During Adaptation Period. Eye Contact Lens. 2016 Mar;42:108-114.
- Bennett ES. Contact lens correction of presbyopia. Clin Exp Optom. 2008 May;91:265-278.



