Innovations in contact lens technology enhance the ability of practitioners to improve their patients’ vision and change their lives. Soft lenses are known for their comfort and for ease of fitting a wide variety of eyes. GP lenses, both corneal and scleral, boast improved optics and superior levels of customization. Hybrid contact lenses join the best traits of these two types of contact lenses into a single device.
With so many choices, deciding which lens is best for each patient can be challenging. For the didactic purposes of better understanding each lens design, and for making evidence-based clinical decisions, below are arguments for using one lens design over another.
CUSTOM SOFT CONTACT LENSES
When prescribing contact lenses for patients, each lens should provide adequate vision, comfort, and fitting characteristics to avoid any mechanical disruption or compromise to the ocular surface. Eyecare practitioners often feel that they have achieved contact lens-fitting success when the patient can see 20/20. Patients who have increasing levels of severity of corneal irregularity often need more advanced lens designs to achieve improved functional vision. This may be one of the reasons why custom or specialty soft lenses are overlooked.
However, patients do not always need to—or cannot always—achieve 20/20, even with more customized designs. Patients may also never have a “textbook” fit with a hybrid or GP contact lens design. Many patients can benefit from custom soft lenses, and there are a few important factors to highlight when considering this lens option, based on our experiences.
1. There are many candidates for custom soft contact lenses beyond high ametropia, and they may be less intimidating compared to other lens designs. Patients who have high regular or irregular astigmatism, asymmetric keratoconus, or pellucid marginal degeneration, those who are intolerant of other lens designs, and post-surgical cases all can be successful with custom soft contact lenses. They may be less intimidating than a corneal GP, hybrid, or scleral lens design due to their size, handling, initial comfort, ease of care and handling, and lack of an initial adaptation period.1 For oblate corneal profiles, including post-refractive surgery and post-keratoplasty cases, there are reverse geometry custom soft lenses available.
There are numerous custom soft lens designs available to fit the needs of many patients.1 Custom soft contact lenses are lathe-cut and manufactured by specialty lens laboratories. They not only provide enhanced comfort, centration, and rotational stability, they can also be manufactured with decentered optics. This allows improved alignment of the optics of a multifocal lens with the patient’s line of sight. Modified zone sizes can also be made to enhance distance and near vision for patients with presbyopia.
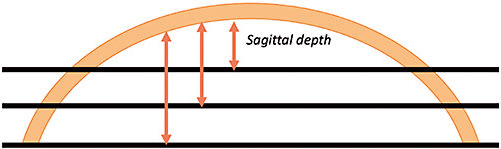
2. The fitting process for custom soft lenses is usually straightforward, and patients generally have an easier time with application and removal training compared to hybrids and sclerals. Custom soft lenses are generally selected based on sagittal height, not on base curve.2 For the same corneal curvature, the sagittal height/depth decreases as the corneal diameter becomes smaller, and then the converse is true; the sagittal height/depth increases as the corneal diameter becomes larger (Figure 1). Custom lenses can solve many fitting challenges for patients who have larger or smaller corneal diameters. To determine the starting overall diameter of the lens, add 2mm to the patient’s horizontal visible iris diameter (HVID).
Most manufacturers recommend fitting custom soft lenses with a diagnostic fitting set; however, they can also be ordered empirically—with fitting calculators or by sending the patient’s data to laboratory consultants. Some custom soft lenses can be designed utilizing software compatible with corneoscleral tomography and profilometry.3 It is recommended to follow the manufacturer’s fitting guide when beginning the fitting process. The initial fitting of a custom soft lens may be like that of other soft lenses and even GP contact lenses; however, the evaluation is slightly different.
It is critical to remember that along with assessing corneal coverage, centration, movement, and rotational stability of the lens, stability of vision with the patient’s blink is imperative for success with custom soft lenses. The base curve of a custom soft lens directly impacts vision, while the skirt or periphery directly impacts the comfort and movement.1 The periphery of the lens can be altered separately from the base curve, to help eliminate the presence of air bubbles or fluting as well as achieve the appropriate amount of lens movement to facilitate tear exchange.
Application and removal of custom soft lenses is usually not difficult, but patients do need to be properly educated. Due to the thickness of custom soft lenses, they may fall off the patient’s finger during lens application. Lenses may need to be applied using two fingers, a tripod method, or even a scleral lens suction remover (Figure 2). To break the suction of the optic zone, lens removal is often performed using the “pop-off” method (Figure 3). Custom soft lenses are typically replaced monthly, quarterly, or annually, and hydrogen peroxide-based disinfection systems are recommended.


3. Custom soft contact lenses are generally more forgiving than corneal GP contact lenses and provide improved centration. Custom soft lenses often provide better initial comfort and centration compared to other lens designs, and they can be manufactured in virtually any parameter. They are fit with reference to the overall corneal shape, rather than the steepest area of the cornea, allowing for improved centration compared to GP contact lenses.2
Patients who have higher levels of corneal irregularity often need increased levels of astigmatic correction, which can be very unstable for the patient. To mask corneal irregularity, custom soft lenses may be designed with an increased center thickness (0.3mm to 0.6mm).3 Increasing the center thickness of the custom soft lens also decreases higher-order aberrations and helps improve overall vision, but it also decreases oxygen transmission.3 Thus, further lens design and fitting modifications should be made.
A custom soft lens can be designed with a lenticular midperiphery and peripheral curve system to thin the lens edge profile thickness and improve oxygen permeability.3 The peripheral curve system can be flattened to increase movement and help facilitate tear exchange. For custom soft lenses, it is acceptable to have as much as 2mm of movement with the blink. Custom soft contact lenses can be manufactured of hydrogel or silicone hydrogel lens materials, the latter of which increases oxygen transmissibility.4
HYBRID CONTACT LENSES
Hybrid contact lenses combine the comfort of soft lenses and the customizable optics of a GP corneal lens. The central GP portion of hybrid contact lenses allows for the correction of difficult refractive and corneal conditions such as high ametropias, astigmatism, presbyopia, corneal ectasias, and irregular astigmatism. In the presence of mild ectasia, hybrid lenses can be ordered empirically, which streamlines the fitting process. For those who have advanced and severe corneal conditions, diagnostically fitting hybrids is preferred.
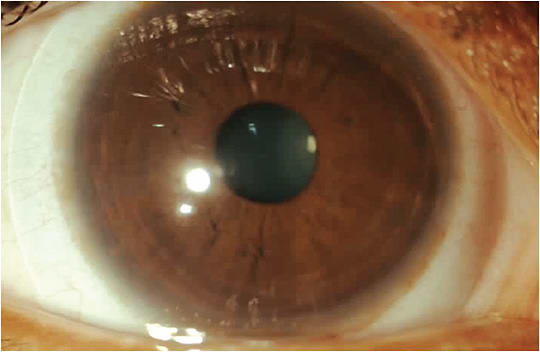
To successfully prescribe hybrid contact lenses, it is important to understand how a proper fit should appear. As the soft skirt centers the GP optic, the best skirt fit is achieved when it is aligned to the conjunctival scleral shape. For patients who have normal corneas, the GP portion should appear as close to an alignment fit as possible (Figure 5). When fitting irregular corneas, such as those in patients who have keratoconus, the GP center will ideally vault the apex of the cone.
The GP lens optics allows for correction of high amounts of regular and irregular astigmatism. Note that hybrid lenses are spherical in the central GP optic. Hybrid lenses are, therefore, limited to correcting corneal astigmatism. Nevertheless, front surface aspheric and extended depth of focus multifocal optics may be added on the anterior surface to correct astigmatic presbyopes. Center-distance multifocal designs are also available for myopia management in myopic children with astigmatism.
Hybrid contact lenses offer many corrective benefits for patients who have complex refractive errors and corneal diseases. In this, hybrid lenses compete with custom soft contact lenses as well as corneal and scleral GP lenses. The benefits of vision and comfort—as compared to other options—are provided below based on our experiences.
1. For astigmatic patients, compared to soft toric lenses, hybrid lenses may offer patients more effective correction. Soft lenses correct astigmatism by adding stabilized toric optics onto the front surface of the lens. This stabilized optic must orient in the correct place to provide optimum vision correction. In high astigmatism, however, fluctuations in vision are more likely to occur due to lens rotation.
In contrast, hybrid contact lens optics can neutralize all corneal astigmatism regardless of the rotational position of the lens, enabling superior quality and stability of vision. This aspect also allows for more predictable correction with multifocal optics.
2. Hybrid lenses are more comfortable than corneal GP lenses. Many patients report initial discomfort with, and awareness of, corneal GP lenses. This awareness is created by lens movement during blink, causing an irritating interaction with the eyelids and the corneal surface. Compared to corneal GP lenses, the soft skirt of hybrid lenses decreases movement of the entire lens, allowing for better initial comfort.
With any contact lens, visual discomfort and degradation of acuity can occur when the optic zone is not centered over the visual axis. Corneal GP lenses can possibly decenter, especially in complex prescriptions such as high-plus and -minus powers. These higher powers are thicker and heavier, which leads to decentered optics and consequential decreased vision. In hybrid lenses, the soft skirt centers the GP optic over the pupil, allowing for optimized acuity and visual comfort. Compared to corneal GP lenses, therefore, hybrid lenses offer better vision in patients with high refractive errors.
3. Prescribing hybrid lenses is more straightforward versus scleral GP lenses. The natural contour of the sclera is asymmetric, making scleral lenses difficult to fit without customized toric peripheral curvatures. Consistently matching the toric peripheral curves of a particular scleral lens to a patient’s unique eye requires specialized knowledge and experience.
In certain situations, instrumentation such as anterior segment ocular coherence tomography and/or scleral topography may be required to obtain a good outcome. Although the barriers to success can be steep it is essential to design a scleral lens that fits well. Poorly fitting scleral lenses can cause degraded vision and impaired comfort from problems such as debris within the lens vault and mechanical irritation of the scleral surface. As the soft skirt of hybrid contact lenses easily conforms to the toric shape of the sclera, the process of fitting these lenses is simpler and more straightforward versus scleral GP lenses.
GP LENSES
GP lenses have gone through an interesting life cycle. At first, all contact lenses on the market were rigid lenses. This led to a meteoric rise in the awareness of contact lenses among those who needed visual correction. When soft lenses arrived on the scene in the 1970s, some declared that the GP lens was “dead.”5
But that did not happen. In fact, in recent years, there has been a resurgence in the GP modality, including one of the fastest-growing segments of the contact lens market, scleral lenses. The benefits of vision and comfort of corneal and scleral GP lenses—as compared to other options—are provided below.
1. GP lenses can be more customized in comparison to soft and hybrid lenses. GP contact lenses certainly offer the most customization of any contact lens modality. This is because each lens is lathed according to the specifications of either an empirical fit or a diagnostic trial. Depending on the skill of the prescriber, GP lenses can be designed with nearly unlimited parameters of base curve, thickness, diameter, peripheral curve width, peripheral curve radius of curvature, material, color, and surface treatment—or simply designed by an expert consultant from one of the GP laboratories.
2. Fitting scleral GP lenses will help build your contact lens practice. A 2006 survey of the American Academy of Optometry’s Diplomates in Cornea, Contact Lenses and Refractive Technologies found that 27.8% of all contact lenses they fit are GP lenses.6 In this same survey, interestingly, when using the Mandell-Moore fitting guide, only 10.4% of the Diplomates considered toric or bitoric lenses difficult to fit.6
GP lens use in the United States reportedly remained steady at 1 in 9 fits and refits.7 The corneal GP market in the U.S. declined slightly in 2021 and was $140 million.8 Scleral lens use, however, has increased since last year, accounting for 4% of all contact lens fits in the United States (including soft).7
Patients in need of something special will seek those practitioners who have developed expertise in something they need. For those willing to specialize and develop expertise in this exciting modality, the future is bright.
3. GP lenses provide better visual outcomes compared to soft contact lenses. The success rate with GP lenses prescribed for both refractive and therapeutic reasons is very high. In a 2017 study, researchers analyzed 232 new GP fits and found a 70% success rate with refractive patients and a 90% success rate with therapeutic patients.9 Although soft contact lenses are generally regarded to be more comfortable, GP lenses can be comfortable in the most discriminating patients: kids. In a 2010 study of 116 kids aged 8 to 11, 70% of GP wearers and 93% of soft lens wearers ended up wearing their lenses to every visit.10 The researchers concluded that children are able to wear both GPs and soft lenses successfully.
4. Scleral lenses help manage advanced corneal disease better than soft and hybrid contact lenses. GP lenses dominate in one specific category of patients: those with corneal and systemic pathologies. In keratoconus, the gold standard treatment has always been corneal GP lenses. Scleral GP lenses are now taking center stage with advanced disease. A 2019 study found that soft toric lenses are used mostly in mild keratoconus, while scleral lenses are used most for advanced disease.11
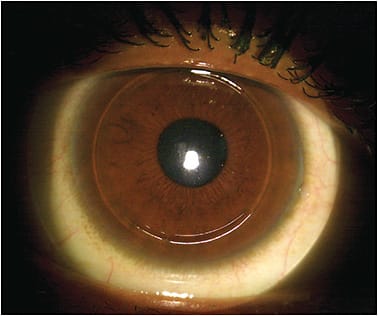
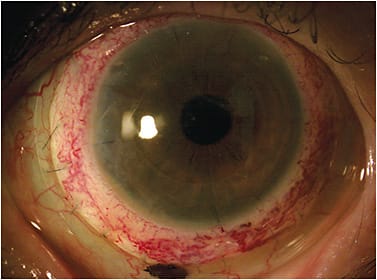
It is also well established that dry eye syndrome, even advanced forms of systemic disease, can be effectively treated with scleral lenses (Figure 6).12-14 What is often not quantified by the peer-reviewed literature is just how transformative scleral lenses are to those who suffer from dry eye disease.
SUMMARY
Patient satisfaction with the quality of their contact lens experience is impacted by the optical results and the physical comfort of the lens, which are not mutally exclusive. GP lenses offer excellent optics even for patients who have highly irregular ocular surfaces. Soft lenses are comfortable, fit a wide variety of eye shapes, and require less knowledge and experience to fit successfully. Hybrid lenses largely combine the positive attributes of each modality.
Each of these lens designs have their unique positive attributes, and there is a place for each lens, depending on what the patient needs. Incorporating all these lens designs into your practice enhances your ability to best care for patients in need of specialty contact lenses. CLS
REFERENCES
- Andrzejewski T. Managing irregular corneas with soft lenses. Rev Cornea Contact Lens. 2020 Feb 15.
- Young G. Ocular sagittal height and soft contact lens fit. J British Contact Lens Assoc. 1992;15(1):45-49.
- Chang C, DeNaeyer GW. Specialty Contact Lenses: Treat Your Keratoconus Patients Right. Rev Cornea Contact Lens. 2017 Mar 15.
- Situ P, Simpson TL, Jones LW, Fonn D. Effects of silicone hydrogel contact lens wear on ocular surface sensitivity to tactile, pneumatic mechanical, and chemical stimulation. Invest Ophthalmol Vis Sci. 2010 Dec;51:6111-6117.
- Efron N. Obituary--rigid contact lenses. Cont Lens Anterior Eye. 2010 Oct;33:245-252.
- Blackmore K, Bachand N, Bennett ES, Henry VA. Gas permeable toric use and applications: survey of Section on Cornea and Contact Lens Diplomates of the American Academy of Optometry. Optometry. 2006 Jan;77:17-22.
- Nichols JJ, Fisher D. Contact Lenses 2020. Contact Lens Spectrum. 2021 Jan;36:24-29,51.
- Bennett E. GP and Custom Soft Annual Report 2021. Contact Lens Spectrum. 2021 Oct;36:20-27.
- Ortiz-Toquero S, Martin M, Rodriguez G, de Juan V, Martin R. Success of Rigid Gas Permeable Contact Lens Fitting. Eye Contact Lens. 2017 May;43:168-173.
- Jones-Jordan L.A, Walline J, Mutti DO, et al. Gas permeable and soft contact lens wear in children. Optom Vis Sci. 2010 Jun;87:414-420.
- Saraç O, Kars ME, Temel B, Çağıl N. Clinical evaluation of different types of contact lenses in keratoconus management. Cont Lens Anterior Eye. 2019 Oct;42:482-486.
- Bavinger JC, DeLoss K, Mian SI. Scleral lens use in dry eye syndrome. Curr Opin Ophthalmol. 2015 Jul;26:319-324.
- Jacobs DS, Rosenthal P. Boston scleral lens prosthetic device for treatment of severe dry eye in chronic graft-versus-host disease. Cornea. 2007 Dec;26:1195-1199.
- Kok JH, Visser R. Treatment of ocular surface disorders and dry eyes with high gas-permeable scleral lenses. Cornea. 1992 Nov;11:518-522.




