The International Forum for Scleral Lens Research (IFSLR), whose mission is to advance the discipline of scleral lens prescribing through the coordinated efforts of evidence-based research and clinical practice, was pleased to host its fifth annual meeting live in Las Vegas preceding the Global Specialty Lens Symposium (GSLS) in January 2022.
This year, the IFSLR spent the first session reviewing topics discussed earlier, such as intraocular pressure (IOP) and midday fogging (MDF), and then focused on two new topics: scleral lenses in severe ocular surface disease in session II, and advanced optical designs in session III.
Here, we summarize the research and discussions during the fifth annual IFSLR.
SESSION I: REVISITING INTERESTING RESEARCH TOPICS
The first session, a mix of high-interest topics from previous IFSLR sessions, served as an update on the latest research and new thinking in areas of interest concerning potential scleral lens complications. Jan Bergmanson, OD, PhD, DSc, started the meeting off with a discussion about ocular anatomy (Figure 1), focusing on concepts pertaining to IOP. Dr. Bergmanson pointed out that many eyecare practitioners have been trapped into thinking that aqueous can only escape from the eye through the trabeculum into the canal of Schlemm and then through collector channels to conjunctival venous circulation.

He reported that at a recent meeting in Texas, 68% of the eyecare practitioners were unaware of how many ways aqueous may leave the eye. There are, in fact, at least six different pathways that lead aqueous out of the eye.1 From the canal of Schlemm—known as the conventional outflow pathway—aqueous may follow three different routes: the conjunctival, scleral, or ciliary venous plexi.
In addition to these three different options, it’s now known that aqueous escapes the globe via the uveoscleral, uveolymphatic, and transscleral pathways.1 Dr. Bergmanson speculated that this multi-pathway system has built-in plasticity that can compensate for impediments in one or more legs of outflow, perhaps triggered by existing afferent and efferent neural pathways in the region.
This discussion of anatomy may help to explain why the studies have shown variable but overall minimal changes in IOP measurements during scleral lens wear.2-10 Future research will, as always, be welcome and will be able to consider the plasticity of the system, but also to address the need for tonometers designed to measure the IOP in eyes wearing scleral lenses.
The second speaker, Maria Walker, OD, PhD, presented a study that used mass spectrometry to determine the lipid and protein composition of the fluid reservoir in midday fogging (MDF).11 The findings of the study suggest that the wax esters, which are nonpolar fatty acyl lipids secreted by the meibomian glands,12-16 showed the strongest correlations with increased MDF severity. These hydrophobic lipids are believed to contribute to reducing tear evaporation,17,18 and also appear to precipitate into an aqueous-based (i.e., saline) fluid reservoir during scleral lens wear in MDF.
No major proteins were found to be associated with MDF, although Dr. Walker did point out that they did not evaluate for small proteins (i.e., cytokines) or cells in this study. Additionally, there is evidence that immune cell accumulation may also contribute to MDF.19
Lastly, Dr. Walker shared that MDF was not correlated to any fitting parameters (i.e., vault, landing zone, etc.) in these subjects, suggesting that MDF may be more dependent on patient characteristics (i.e., composition of lipids in tear film) rather than the scleral lens fit itself, although this is controversial.19 However, she also pointed out that MDF can present variably in clinic and that this area, much like IOP, needs further investigation to be fully understood.
This session continued with the final speaker, Damien Fisher, BAppSc(Optom), PhD, who presented findings from a recent study on conjunctival prolapse,20 the phenomenon of conjunctival tissue “drawing up” under the peripheral regions of the scleral lens.21,22
Dr. Fisher proposed that the pressure system beneath a sealed scleral lens is likely the cause of prolapse with scleral lenses, noting that it tends to occur in areas of excessive limbal clearance. In the clinical study, the researchers used optical coherence tomography (OCT) to measure conjunctival prolapse in 10 healthy adults wearing 16.5mm diameter scleral lenses. Subjects were fitted with low (150µm), medium (500µm), and high (750µm) vault over the cornea, and wore the lenses for 90 minutes each before the prolapse was measured in the horizontal meridian using OCT.
The study found that prolapse was observed in 37% of the measurements, and that 80% of subjects experienced prolapse with at least one fitting design. Prolapse occurred more in the nasal quadrant, although it was not associated with fluid reservoir (FR) thickness asymmetry. Dr. Fisher reported that subjects who had greater amounts of lens settling showed more prolapse, which could be related to a relatively spongy conjunctiva.
Interestingly, he noted that the data from the low-vault group seemed to indicate that “thin film adhesion” factors may make someone who is wearing a lens that has less clearance and greater settling more susceptible to prolapse.20 Dr. Fisher noted that conjunctival prolapse does not appear to adversely affect corneal function or lens performance in the short term,23 but he recommends that future studies evaluate prolapse in the vertical meridian and more extensively in lower vault scenarios.
SESSION II: SCLERAL LENSES AND OCULAR SURFACE DISEASE
The second session of the IFSLR was dedicated to ocular surface disease and scleral lenses. The session opened with the keynote speaker, Jia Yin, MD, PhD, MPH, discussing a publication that assessed the long-term use of scleral lenses as a drug delivery system for bevacizumab in cases of corneal neovascularization.24
Thirteen patients with active corneal neovascularization (Figure 2) that threatened the visual axis received 1% bevacizumab in their scleral lenses between 2006 and 2017. Twelve (92%) patients had neovascular regression and 10 cases demonstrated an improvement in best-corrected vision. One patient had progression after the treatment was discontinued; none of the patients experienced any adverse events.

Dr. Yin also described the benefits of scleral lenses for a complex case that she managed at Massachusetts Eye and Ear. A 51-year-old male who had a history of atopic disease, keratoconus, and limbal stem cell deficiency had been successfully wearing scleral lenses for 10 years prior to presenting with acute hydrops, epithelial defect, descemetocele, and stromal infiltrate.
Dr. Yin performed a penetrating keratoplasty and cataract extraction. The patient resumed scleral lens wear one week post-op to heal the epithelial defect, and vision improved to 20/60; four months later, he developed a fluoroquinolone-resistant suture infiltrate. Fortified antibiotics were delivered to the surface for seven months with a scleral lens and the patient ultimately had 20/50 vision that currently remains stable. Dr. Yin concluded by stating that careful use of scleral lenses can facilitate epithelial defect healing shortly after corneal transplantation while also acting as a drug delivery system.
John Gelles, OD, then presented unique cases of scleral lenses in lipid keratopathy and descemetocele.25,26 To his knowledge, there had only been one previous case report of a descemetocele in the literature, who was followed for one year wearing a scleral lens.27
Dr. Gelles managed a case of a descemetocele that occurred because of a trigeminal nerve (CNV) and cranial nerve (CNVII) palsy.26 The patient wore the lens on an extended wear basis until the epithelial defect re-epithelialized. Due to the extended wear needed for this patient, epithelial bullae eventually formed, at which time the patient was switched to daily wear and remained stable after one year.
Dr. Gelles’ next case demonstrated the success of a scleral lens for lipid keratopathy that resolved after three years of scleral lens wear.25 Collectively, the cases presented by Drs. Yin and Gelles reminded us of the protective capacity of the scleral lens to heal epithelial decompensation and keratopathies.
Tom Arnold, OD, reported on his investigation of corneal edema after scleral lens wear in patients who had a history of radial keratotomy.28 Dr. Arnold and colleagues found that there was 2.19% corneal edema centrally in nine subjects that increased in magnitude in the periphery of the cornea. Specifically, in the superior and inferior nasal areas, at an annulus of approximately 3mm from the central cornea, edema reached its greatest and was between 3% and 4% greater than without lens wear.
Despite these statistically significant increases in corneal swelling with scleral lenses, no adverse events were reported, and the patients were successful with lens wear. Dr. Arnold reminded the group that vaulting over the cornea is important to avoid mechanical contact of the lens on the cornea, but that the vault should be minimal to reduce the risk of increasing corneal edema.
Muriel Schornack, OD, concluded the session by sharing data from the Scleral Lenses in Current Ophthalmic Practice Evaluation (SCOPE) study group, which queried practitioners about scleral lens indications and usage in ocular surface disease.29,30 The surveys found that practitioners reported managing the following ocular surface disease conditions with scleral lenses: keratoconjunctivitis sicca (43% of practitioners report managing), exposure (42%), Sjögren’s (35%), graft-versus-host disease (33%), Stevens-Johnson syndrome (21%), limbal stem cell deficiency (18%), and cicatrizing disease (15%).29
Dr. Schornack reported that the percentage of scleral lenses utilized for ocular surface disease was 16% in both 2015 (n = 672) and 2020 (n = 717). Lastly, practitioners intervene with scleral lenses after topical lubricants, meibomian gland expression, cyclosporine/lifitegrast, steroids, and punctal plugs.
SESSION III: SCLERAL LENSES AND OPTICS
Geunyoung Yoon, PhD, started the third and final session by discussing individualized presbyopia correction with contact lenses and intraocular lenses (IOL). After briefly describing the refractive and diffractive bifocal/trifocal lenses, he illustrated the limitations of soft and scleral lenses and IOL in terms of discrete foci, eye aberrations, and decentration (i.e., often inferior temporal with scleral lenses). Dr. Yoon proposed solutions to these three limitations by adding 1) refractive extended depth of focus, 2) wavefront-guided higher-order aberration (HOA) correction, and 3) customizing optical zone location, respectively.
Dr. Yoon discussed a current project: his laboratory is designing scleral lenses for presbyopes, in which these three features will be implemented to optimize vision. Dr. Yoon showed the improvement in total root mean square (RMS) when comparing a conventional (no HOA correction) (0.58µm) to a wavefront-guided (HOA- corrected) scleral lens (0.15µm). For presbyopes, particularly those who have high numbers of HOAs, combining wavefront-guided optics with extended depth of focus presents an opportunity to enhance optical performance. He concluded that individualized and highly customized visual correction with scleral lenses can improve quality of life for presbyopes.
Gonzalo Carracedo, PhD, presented outcomes of conventional multifocal scleral lenses in presbyopia. His research evaluated 20 normal, healthy presbyopes and measured high-contrast visual acuity, contrast sensitivity, stereopsis, and binocular defocus. He compared monofocal, multifocal, and decentered multifocal designs, and the data showed better performance with the multifocal designs than with monofocal scleral contact lenses in intermediate and near vision.
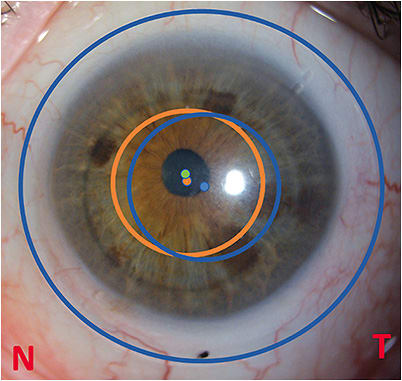
Furthermore, the option to decenter the optical zone of the lens to center it over the visual axis of the patient improved the visual quality at all distances, showing that this type of optical design will likely be employed in many future lenses (Figure 3). Dr. Carracedo’s presentation of patient experience with multifocal scleral lenses shows that these are becoming more successful when introduced into patient care.
Session III concluded with Greg Gemoules, OD, who discussed new technology for correcting HOAs, providing insight from his patient and lens design experience. He added wavefront-guided optics to his scleral lens practice in 2011, and currently uses OCT for imaging the ocular surface. The large width and ability to acquire high-quality off-center images were of special importance, as these could be readily stitched together to produce a larger mosaic for designing large scleral lenses of 20+mm.
However, Dr. Gemoules noted that his current OCT is at the end of its product life cycle and shared information about a new design platform, which is one of the more widely used high-end computer-aided-design software suites with advanced surfacing capabilities. An engineering subsidiary created templates based on best practices, as well as programs for importing and exporting various data from other systems. With his HOA-correcting scleral lenses, Dr. Gemoules reported an average improvement in HOAs of 64% compared to conventional optics (excluding eyes with scars) for keratoconus patients, and noted that many post-laser-assisted in situ keratomileusis (LASIK) patients achieve 20/10 visual acuity and are nearly aberration-free.
Collectively, the virtual and live presentations at the fifth annual IFSLR were a resounding success, and the live discussion was welcomed by all. The sixth annual IFSLR is scheduled live for Jan. 18, prior to the commencement of GSLS 2023 in Las Vegas. CLS
Acknowledgment: The authors would like to acknowledge the scleral lens researchers and clinicians who presented at the fifth annual IFSLR and provided content for this article. Support for the fifth IFSLR was provided by CooperVision Blanchard and Bausch Health, and we appreciate the educational support from our media partners, PentaVision (a division of BroadcastMed) and GSLS, as well as our educational partner, The Scleral Lens Education Society.
REFERENCES
- Bergmanson JPG. Limbus, Filtration Angle and Aqueous Outflow Pathways. In: Bergmanson JPG, ed. Clinical Ocular Anatomy and Physiology. 29th ed. Texas Eye Research and Technology Center; 2022:138-150.
- Kramer EG, Vincent SJ. Intraocular pressure changes in neophyte scleral lens wearers: A prospective study. Cont Lens Anterior Eye. 2020 Dec;43:609-612.
- Walker M, Pardon L, Redfern R, Patel N. IOP and Optic Nerve Head Morphology during Scleral Lens Wear. Optom Vis Sci. 2020 Sep;97:661-668.
- Nau CB, Schornack MM, McLaren JW, Sit AJ. Intraocular Pressure After 2 Hours of Small-Diameter Scleral Lens Wear. Eye Contact Lens. 2016 Nov;42:350-353.
- Cheung SY, Collins MJ, Vincent SJ. The impact of short-term fenestrated scleral lens wear on intraocular pressure. Cont Lens Anterior Eye. 2020 Dec;43:585-588.
- Fogt JS, Nau CB, Schornack M, Shorter E, Nau A, Harthan JS. Comparison of Pneumatonometry and Transpalpebral Tonometry Measurements of Intraocular Pressure during Scleral Lens Wear. Optom Vis Sci. 2020 Sep;97:711-719.
- Shahnazi KC, Isozaki VL, Chiu GB. Effect of Scleral Lens Wear on Central Corneal Thickness and Intraocular Pressure in Patients with Ocular Surface Disease. Eye Contact Lens. 2020 Nov;46:341-347.
- Formisano M, Ludovico FF, Santino A, Spadea PL. Effects of Scleral Contact Lenses for Keratoconus Management on Visual Quality and Intraocular Pressure. Ther Clin Risk Manag. 2021 Jan 25;17:79-85.
- Vincent SJ, Alonso-Caneiro D, Collins MJ. Evidence on scleral contact lenses and intraocular pressure. Clin Exp Optom. 2017 Jan;100:87-88.
- Samaha D, Michaud L. Bruch Membrane Opening Minimum Rim Width Changes During Scleral Lens Wear. Eye Contact Lens. 2021 May 1;47:295-300.
- Walker M. The Impact of a Scleral Lens on the Eye. A PhD Dissertation. University of Houston; 2021.
- Chen J, Green-Church KB, Nichols KK. Shotgun lipidomic analysis of human meibomian gland secretions with electrospray ionization tandem mass spectrometry. Invest Ophthalmol Vis Sci. 2010 Dec;51:6220-6231.
- Nicolaides N, Kaitaranta JK, Rawdah TN, et al. Meibomian gland studies: comparison of steer and human lipids. Invest Ophthalmol Vis Sci. 1981 Apr;20:522-536.
- Butovich IA, Uchiyama E, di Pascuale MA, McCulley JP. Liquid chromatography-mass spectrometric analysis of lipids present in human meibomian gland secretions. Lipids. 2007 Aug;42:765-776.
- Butovich IA. Tear film lipids. Exp Eye Res. 2013 Dec;117:4-27.
- Butovich IA, Wojtowicz JC, Molai M. Human tear film and meibum. Very long chain wax esters and (O-acyl)-omega-hydroxy fatty acids of meibum. J Lipid Res. 2009 Dec;50:2471-2485.
- Viitaja T, Moilanen J, Svedstrom KJ, Ekholm FS, Paananen RO. Tear film lipid layer structure: self assembly of o-acyl-w-hydroxy fatty acids and wax esters into evaporation-resistant monolayers. Nano Letters. 2021 Sep,21:7676-7683.
- Bron AJ, Tiffany JM, Gouveia SM, Yokoi N, Voon LW. Functional aspects of the tear film lipid layer. Exp Eye Res. 2004 Mar;78:347-360.
- Postnikoff CK, Pucker AD, Laurent J, Huisingh C, McGwin G, Nichols JJ. Identification of Leukocytes Associated With Midday Fogging in the Post-Lens Tear Film of Scleral Contact Lens Wearers. Invest Ophthalmol Vis Sci. 2019 Jan 2;60:226-233.
- Fisher D, Collins MJ, Vincent SJ. Conjunctival prolapse during open eye scleral lens wear. Cont Lens Anterior Eye. 2021 Feb;44:115-119.
- Caroline P AM. Conjunctival prolapse, hooding, chalasis or…. Contact Lens Spectrum. 2012 Apr;27:56.
- Walker MK., Bergmanson J, Miller W, Marsack J, Johnson L. Complications and fitting challenges associated with scleral contact lenses: A review. Cont Lens Anterior Eye. 2016 Apr;39:88-96.
- Severinsky B, Behrman S, Frucht-Pery J, Solomon A. Scleral contact lenses for visual rehabilitation after penetrating keratoplasty: long-term outcomes. Cont Lens Anterior Eye. 2014 Jun;37:196-202.
- Yin J, Jacobs DS. Long-term outcome of using Prosthetic Replacement of Ocular Surface Ecosystem (PROSE) as a drug delivery system for bevacizumab in the treatment of corneal neovascularization. Ocul Surf. 2019 Jan;17:134-141.
- Gelles JD, Hillier KE, Krisa S, Greenstein SA, Hersh PS. Lipid Keratopathy Management With Therapeutic Scleral Lens Wear. Eye Contact Lens. 2022 Feb 1;48:91-94.
- Gelles JD, Bekerman VP, Greenstein SA, Shafiq M, Hersh PS. Descemetocele Management With Therapeutic Scleral Lens Wear. Eye Contact Lens. 2021 May 1;47:314-316.
- Xu M, Randleman JB, Chiu GB. Long-Term Descemetocele Management with Prosthetic Replacement of the Ocular Surface Ecosystem (PROSE) Treatment. Eye Contact Lens. 2020 Mar;46:e7-e10.
- Arnold TP, Vincent SJ. Scleral Lens–Induced Corneal Edema After Radial Keratotomy. Eye Contact Lens. 2021 Oct 1;47:575-577.
- Nau CB, Harthan J, Shorter E, et al. Demographic Characteristics and Prescribing Patterns of Scleral Lens Fitters: The SCOPE Study. Eye Contact Lens. 2017 Sep;44 Suppl 1:S265-S272.
- Harthan J, Shorter J. Therapeutic uses of scleral contact lenses for ocular surface disease: patient selection and special considerations. Clin Optom (Auckl). 2018 Jul;11:65-74.




