As with past annual reports, the information in this article is obtained from a combination of recent research and polling of both the Contact Lens Spectrum readership and experts in the contact lens industry. Recent developments in corneal GPs, scleral lenses, myopia management, and custom soft lenses will be highlighted. Likewise, new advancements in keratoconus and multifocal contact lenses will be presented.
The GP Lens Institute (GPLI) Advisory Board, consisting of prominent experts in specialty contact lenses, were surveyed as to what they believed the most important developments in GP and custom soft lenses were in the past year. Here are the top five responses (n = 49). This year, there was a three-way tie for first between myopia management—multifocal soft applications, new orthokeratology designs, and increasing importance and need; wavefront correction—understanding of optics, higher-order aberrations (HOAs), and wavefront-guided lens designs; and scleral advancements—increasing use of corneoscleral topography, profilometry-driven designs, and advancements in scleral lens optics and designs. Next on the list was advancements in lens materials. Rounding out the top five was multifocal advancements, specifically offset optics and new soft, GP, and hybrid lens designs.
With the much-needed current emphasis on controlling the progression of myopia—to the point where it is rapidly becoming standard of care—this is a very appropriate area to begin this year’s annual report.
MYOPIA MANAGEMENT
Nowhere can custom soft and GP lenses be as closely associated as with the management of myopia. With the current interest in this area—which will only increase in the years ahead—the emphasis in the contact lens industry today is toward technology in this field that has culminated in the introduction of new designs with the potential of exhibiting even greater effect on the progression of myopia in young people. According to Contact Lens Spectrum’s recent market data, when asked about the greatest growth potential in 2022 of several specialty lens options, custom soft and orthokeratology were ranked at the top.1
Soft Multifocal Lenses As in recent years, soft multifocal contact lenses have been the most popular method of myopia management among our responding readership (Figure 1). Clinical research has been very promising in this area. A recent six-year study with young people wearing a U.S. Food and Drug Administration (FDA)-approved soft lens for myopia management resulted in a significant change over a three-year period.2 And, when the control (conventional daily wear soft) was changed to the myopia management lens after three years, they exhibited a 71% slowing of myopia over the next three years. Another six-year study in which a commonly available soft multifocal lens was worn by almost 200 subjects found that myopia progression was slowed by approximately 85% compared to baseline, with 91% showing a decrease in myopia progression and 79% exhibiting a ≥ 70% reduction in myopia progression.3

It has been reported that wearing these lenses is not detrimental to athletes due to peripheral defocus and, in fact, the quality-of-life benefits are evident.4 It was also reported that lifestyle changes can be beneficial; specifically, less time on computers and cell phones and more time outside was recommended. To the latter point, it was recently found that young people spending more than three and four hours of outdoor time per week were associated with the best response in the first year and in the second year of soft myopia management treatment, respectively.5
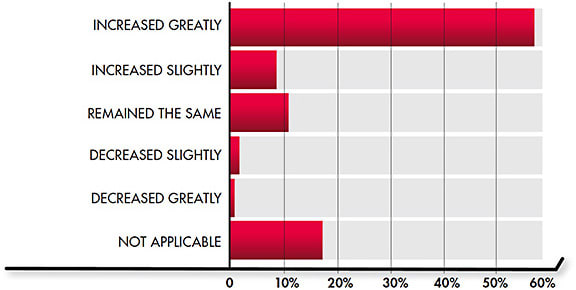
Orthokeratology It is also important to note that orthokeratology use appears to be on the rise, as well. More than 58% of our respondents indicated that it has increased greatly in their practice over the last year (Figure 2). It is also important to note that the “not applicable” (i.e., not fitting orthokeratology lenses) has decreased from slightly greater than 50% in last year’s survey to 17.6% this year.6
Likewise, whereas the Contact Lens Spectrum market research indicated that 3% of GPs fit by practitioners in 2020 were orthokeratology,7 this value increased to 10% in 2021.1 The recently published results of the Fitting of Orthokeratology in the United States (FOKUS) survey were very encouraging.8 It was estimated that the number of eyecare providers (ECPs) actively fitting and managing orthokeratology patients in the United States is approximately 3,000 with high potential for growth within the next two years. Of the 545 ECPs responding to the FOKUS survey, 283 were actively fitting orthokeratology and, of those who are not fitting this modality, 46% plan to initiate it within the next two years.
Certainly, an exciting development in the past 12 months has been the FDA approval in November 2021 of a one-day soft lens for myopia management. While currently only available in limited markets in the U.S., plans to expand the launch are forthcoming.
The results of recent studies have been beneficial in our understanding of both how to optimize lens design as well as success. It has been found that the use of a smaller-than-average (i.e., 5mm) optical zone/treatment diameter can yield a faster reduction in myopia and a smaller aspheric treatment zone.9 Long-term results have also found orthokeratology to be both safe and effective.10
That said, compliance with proper lens wear and care can be substandard; therefore, in clinical practice this should be emphasized and regularly reinforced.11 With attention to the fitting process, careful follow-up, and compliance, orthokeratology can be a safe and effective method of slowing axial elongation in young people.12
Combination Therapy Studies that have looked at low-dose atropine in combination with orthokeratology have been encouraging as the combined treatment appears to result in a greater effect than one method used alone.13,14 The long-anticipated results of the Bifocal & Atropine in Myopia (BAM) Study have recently been published.15 This three-year study found a similar change in axial length change and myopia progression between soft multifocal lenses used alone and in combination with 0.01% atropine. The total refractive change was –0.52D for the bifocal-atropine group, –0.55D for the bifocal-alone group, and –1.09D for the single-vision-lenses group.
GP LENSES
GP lenses appear to be holding their own according to recent Contact Lens Spectrum market data, which shows 10% of contact lens fits and refits are into GP lenses as compared to 11% one year ago.1,7 In response to our readership poll, it was encouraging that 96.5% of the respondents indicated they fit GP lenses. Figure 3 shows the distribution of our readership respondents’ GP fitting preferences.

Once again, it is apparent that scleral contact lenses most certainly have positively impacted GP fitting trends. Empirical fitting continues to an increasingly popular method of fitting corneal GPs (Table 1). In all categories, empirical fitting increased versus this same survey 12 months ago.6 The most significant increase occurred in orthokeratology/corneal reshaping increasing from 50% empirical fitting one year ago to 71% this year. It is also important to note that more than 1 in 3 of scleral fits from the survey respondents was empirical. This could reflect, in part, the increasing use of profilometry-driven designs.
| TYPE OF DESIGN | EMPIRICAL (%) | DIAGNOSTIC (%) |
| Toric | 83 | 17 |
| Multifocal | 86 | 14 |
| Spherical | 79 | 21 |
| Hybrid | 67 | 33 |
| Corneal Reshaping | 71 | 29 |
| Non-Scleral Irregular Cornea GP | 48 | 52 |
| Scleral | 35 | 65 |
Scleral Lenses Scleral lens use appears to remain stable holding at 14% of GP lens fits in 2021, according to the recent Contact Lens Spectrum readership poll.1 However, when asked about scleral contact lens use in the last 12 months, the most common response (56.8%) is that it has “increased greatly” (Figure 4). A very good overview of how to position scleral lenses versus corneal lenses was recently published and is summarized in Table 2.16

| SCLERAL | CORNEAL |
| 1. Moderate to Severe Irregular Cornea | 1. Mild-to-Moderate Irregular Cornea |
| 2. Ocular Surface Disease/Severe Dry Eye Disease | 2. Presbyopia |
| 3. “Wow” Effect with Initial Comfort | 3. Orthokeratology |
| 4. Cannot Dislodge or Eject | 4. Tear Exchange |
| 5. Ease of Handling |
It is important to note that two of the three most important advancements (i.e., wavefront correct and scleral advancements) pertain to scleral contact lenses. Several contact lens laboratories have been developing wavefront-guided designs to reduce HOAs, which is especially important with diseased eyes, notably keratoconus. In fact, a two-line improvement in visual acuity was recently reported with a patient who was fitted with wavefront-guided optics on custom ocular impression-based scleral lenses versus impression-based optics with traditional optics.17 With scleral profilometry, the ability to align the contact lens back surface to the eye shape will help this technology gain greater success.
The increase in empirical fitting of scleral lenses is an indication that scleral topography-guided lenses are increasing in use. Laboratories have developed software to utilize this technology to manufacture truly custom lenses to align with the sclera in all meridians and provide a viable option for patients who have failed with traditional scleral lenses.
Each laboratory varies in their method of data collection, design concepts, and consultation but, ultimately, the patient typically benefits from this technology. Some designs are data-driven to such an extreme that they match the exact shape of the sclera and the cornea; other designs are created with the limbus and the sclera as a primary profile design. It is significant to mention a recent exclusive distribution agreement that allows access to a software that gives practitioners the ability to make custom lens designs using free-form manufacturing technology and 3D imaging.
The use of toric haptics is becoming more the rule than the exception, again to achieve better alignment with a sclera that is typically toric in curvature. Whereas in 2021, there was parity in the readership in terms of what percent of respondents fit, at minimum, 50% in each modality—in 2022, toric haptics are more often preferred (Table 3).
| LENS TYPE | ≥ 20% OF PATIENTS | ≥ 50% OF PATIENTS | NOT APPLICABLE (I.E., DOES NOT FIT) |
| Scleral Lenses | 70% | 47% | 17% |
| Intralimbal | 23% | 11% | 45% |
| Small-Diameter GPs | 43% | 9% | 15% |
| Hybrid | 36% | 4% | 23% |
| Custom Soft | 19% | 4% | 34% |
| Piggyback | 9% | 2% | 40% |
Scleral contact lenses have been a popular topic for recent clinical research. In a study involving 41 eyes of 24 keratoconus patients fit into scleral lenses, the functional improvement and quality of life improved significantly, especially in patients who have more advanced stages of the disease.18
Scleral contact lenses have also been found to be an effective means of visual rehabilitation in aphakic children after lensectomy. In one study, the authors concluded that scleral lenses may be used long term with good lens wear compliance, excellent visual results, and acceptable adverse events.19 It has also been found that, as the vault behind a scleral lens increases, significant changes were detected in the spherical equivalent and HOAs, especially coma and spherical aberration.20 It was recommended to consider the impact on vision—notably HOAs—when increasing the scleral lens vault.
Finally, one of the top five advancements in GP lenses in the past year (as reported earlier) pertains to GP contact lens materials. In particular, the GPLI respondents often noted the increasing popularity of newly introduced hyper-Dk lens materials for scleral lens designs. This, in combination with polyethylene glycol (PEG), an encapsulated coating that can be complimented by monthly restoration treatment solution, can maintain long-term wettability of these highly permeable lens materials.
Keratoconus Every year, the readership are asked their breakdown as it pertains to contact lens correction of the irregular cornea. The results are given in Table 4. What is notable is how scleral lenses have become the overwhelming “go-to” lens (i.e., ≥ 50% of fits) for our readership, being fit more than 4.5 times more than the next popular design (intralimbal). It is also notable that the “Not Applicable/Does Not Fit Scleral Lenses” was reported by only 17% of the respondents.
| LENS TYPE | ≥ 20% (OF RESPONDENTS) | ≥ 50% (OF RESPONDENTS) | NOT APPLICABLE (I.E., DOES NOT FIT) |
| Aspheric | 58% | 33% | 18% |
| Scleral | 24% | 18% | 42% |
| Concentric | 35% | 13% | 36% |
| Segmented, translating | 26% | 9% | 42% |
| Hybrid | 24% | 9% | 51% |
Overall, however, corneal GP lenses still prevail and that was the result found in a study of 217 keratoconus patients in which 60% were wearing corneal GPs, 22% scleral lenses, 12% soft torics, 5% hybrid, and 1% soft sphere.21 A very good overview of the fitting, evaluation, and management of keratoconus was recently published by Itoi and Itoi22; likewise a comprehensive overview of the epidemiology, etiology, clinical features, detection, and management and treatment strategies was recently reported by Santodomingo-Rubido and colleagues.23
Of course, corneal cross-linking continues to be a significant treatment option for slowing or halting keratoconus, notably in the early stages. It has also been found to improve contact lens tolerance by providing a more regular-shaped cornea.24 Specifically, the topographic changes in the last postoperative period may have a positive effect on contact lens fitting.24
Likewise, as this entire article emphasizes, the impact of HOAs in keratoconus and the benefits of incorporating aberrometry into clinical practice have been significant.25 This allows for early diagnosis of keratoconus, which could then result in earlier intervention and preservation of vision in these patients.
Presbyopia The Contact Lens Spectrum readership was surveyed as to how much they fit of five popular GP presbyopic designs including aspheric, scleral, concentric, segmented/translating, and hybrid. The results are shown in Table 5. As in previous years, aspheric multifocals predominate, although for the first-time scleral wearers, multifocals were the second most popular option as the “go-to” lens.
| TYPE OF DESIGN | 10% | 20% | 30% | 40% | 50% | 60% | 70% | 80% | 90% | 100% | N/A |
| Spherical Soft Multifocal | 31 | 13 | 7 | 4 | 7 | 2 | 9 | 4 | 7 | 7 | 4 |
| Custom Soft Multifocal | 18 | 13 | 7 | 9 | 11 | 0 | 4 | 0 | 4 | 0 | 29 |
| GP Aspheric Multifocal | 38 | 20 | 0 | 7 | 4 | 0 | 0 | 2 | 0 | 2 | 16 |
| Hybrid Multifocal | 20 | 11 | 0 | 2 | 2 | 2 | 0 | 0 | 0 | 0 | 47 |
| Translating, Segmented GP Multifocal | 31 | 11 | 2 | 2 | 2 | 0 | 0 | 0 | 0 | 0 | 38 |
Much current interest pertains to decentered optics with scleral designs to optimize alignment as they customarily decenter slightly inferior (due to mass) and temporal (due to an elevated nasal sclera). Rodriguez provided the results of a study comparing a single-vision optics scleral lens, a scleral multifocal lens without decentered optics, and a scleral multifocal with decentered optics.26 The authors determined that the intermediate, near, and subjective vision were all significantly better with the decentered optics design and the distance vision was slightly better. One recently introduced scleral incorporates aberration control to help address lens-induced aberrations.
CUSTOM SOFT
Much of the emphasis today with custom soft contact lenses pertains to the aforementioned myopia management modality. Whether it pertains to this application or correction of astigmatism, presbyopia, or both, technology is driving this modality to be a viable alternative to an increasing number of patients. Davis and Schwartz surveyed a large group of specialty lens fitters and found that 78% prescribed custom soft lenses to manage astigmatism, presbyopia, ametropia, anisometropia, myopia management, and to retain contact lens prescriptions.27 There are some exciting lenses under development.
The increasing use of corneoscleral topographers does not simply benefit scleral lens fitting. Research has shown that here is a large variability in ocular sagittal height beyond the cornea in healthy eyes.28 This brings into question the traditional method of selecting the parameters for custom soft lenses only via corneal measurements.
Current lathing technology coupled with the availability of silicone-hydrogel lens materials allows for the manufacture of soft toric lenses in practically any sphere power, cylinder power, and axis. That said, the readership survey showed that standard soft toric lenses were overwhelmingly the modality of choice for patients who have ≥ 2D of refractive cylinder (Table 6).
| TYPE OF DESIGN | 10% | 20% | 30% | 40% | 50% | 60% | 70% | 80% | 90% | 100% | N/A |
| Standard Soft Toric | 0 | 7 | 9 | 4 | 16 | 13 | 13 | 16 | 16 | 2 | 2 |
| Custom Soft Toric | 24 | 22 | 9 | 9 | 4 | 2 | 0 | 2 | 0 | 2 | 24 |
| Spherical GP | 39 | 13 | 11 | 2 | 11 | 0 | 0 | 0 | 0 | 0 | 16 |
| Toric GP | 38 | 18 | 9 | 4 | 4 | 0 | 2 | 0 | 0 | 0 | 16 |
Patients who have not been successful in other soft lens designs are often good candidates for custom soft multifocals. This is because these custom lenses can potentially provide a better fit and/or meet the needs of a nonstandard prescription.29
Multifocal toric soft options are becoming increasingly available and popular. The ability to provide made-to-order designs and provide them relatively quickly to practices is beneficial.30 As with scleral lenses, decentered optics are being introduced into custom soft multifocal designs, which may provide success if other designs fail.
Finally, we are all awaiting the introduction of a lens for presbyopia that features a novel design and that has great potential to provide good vision at all distances.
WHAT TO EXPECT IN THE NEAR FUTURE
When the GPLI Advisory Board was surveyed as to what they believe the most important advancements will be in GP and custom soft lenses in the next 12 months, the following four responses were most common, beginning with the most popular option:
- HOA-correcting lens designs
- Custom lens designs for myopia management
- Lenses for drug delivery
- Increased use of profilometry-designed scleral contact lenses
As it pertains to drug delivery, it is important to recognize the recent FDA approval of the first drug-eluting lenses.31 They are daily disposable lenses indicated for the prevention of ocular itch due to allergic conjunctivitis. Other drug-eluting lenses with varying applications should follow in the years ahead.
Smart contact lens technology has been under investigation by many companies for several years with presbyopia as a a prime target. In addition, one company is using its smart lens technology—combining augmented reality, wearable technology, and personal performance data—to develop partnerships with leading sports and fitness brands in an effort to enhance athletic performance.
GP and custom soft contact lenses are moving in a very positive direction, notably in improving the quality of life of young myopes, irregular cornea patients, presbyopes, and those who are manifesting high astigmatism. The future looks especially exciting for applications such as drug delivery, accommodating lenses, and continued options for correction of HOAs. Stay tuned! CLS
Acknowledgements: Roxanne Achong-Coan, OD; Tom Arnold, OD; Adeline Bauer, OD (Valley Contax); Cindy Belliveau (Visionary); Edward Boshnick, OD; Marc Botticella (Bausch + Lomb); Mile Brujic, OD; Karen Carrasquillo, OD, PhD; Gloria Chiu, OD; Brian Chou, OD; Robert Davis, OD; Karen DeLoss, OD; Greg DeNaeyer, OD; S. Barry Eiden, OD; Rob Ensley, OD; Daddi Fadel, DipOptom; Melanie Frogozo, OD; Dan Fuller, OD; John Gelles, OD; Alan Glazier, OD; Bob Grohe, OD; Susan Gromacki, OD; Jennifer Harthan, OD; Jason Jedlicka, OD; Matt Kauffman, OD; Elise Kramer, OD; Jamie Kuhn, OD; Matt Lampa, OD; Michael Lipson, OD; Eric Marshall (Visionary Optics); Robert Maynard, OD; Brooke Messer, OD; Langis Michaud, OD, MSc; Chandra Mickles, OD (Johnson & Johnson); Heidi Miller, OD; Troy Miller (AccuLens); Clarke Newman, OD; Roxanna Potter, OD; Tom Quinn, OD; Renee Reeder, OD; Susan Resnick, OD; Pam Satjawatcharaphong, OD; Jack Schaeffer, OD; Cristina Schnider, OD; Moshe Schwartz, OD; Joe Shovlin, OD; Brian Silverman, OD; Jeffrey Sonsino, OD; Long Tran, OD; Eef van der Worp, BOptom, PhD; Ashley Wallace-Tucker, OD; Jeff Walline, OD; PhD, Maria Walker, OD; Bruce Williams, OD; Stephanie Woo, OD
REFERENCES
- Nichols JJ, Starcher L. Contact Lenses 2021. Contact Lens Spectrum. 2022 Jan;37:22-24,26,28,29.
- Chamberlain P, Bradley A, Arumugam B, et al. Long-term effect of dual-focus contact lenses on myopia progression in children: A 6-year multicenter clinical trial. Optom Vis Sci. 2022 Mar 1;99:204-212.
- Cooper J, O’Connor B, Aller T, Dillehay SM, Wiebel K, Benoit D. Reduction in myopic progression using a multifocal soft contact lens: A retrospective cohort study. Clin Ophthalmol. 2022 Jul 4:16:2145-2155.
- Bennett ES, Fisher D, Morgan E. Highlights from the 2022 GSLS. Contact Lens Spectrum. 2022 Apr;37:20-22,24-26.
- Prieto-Garrido FL, Hernández Verdejo JL, Villa-Collar C, Ruiz-Pomeda A. Predicting factors for progression of the myopia in the MiSight assessment study Spain (MASS). J Optom. 2022 Jan-Mar;15:78-87.
- Bennett ES. GP and Custom Soft Annual Report. Contact Lens Spectrum. 2021 Oct;36:20-27.
- Nichols JJ, Fisher D. Contact Lenses 2020. Contact Lens Spectrum. 2021 Jan;36:24-29,51.
- Lipson MJ, Curcio LR. Fitting of orthokeratology in the United States: A survey of the current state of orthokeratology. Optom Vis Sci. 2022 Jul 1;99:568-579.
- Zhang Z, Chen Z, Zhou J, et al. The effect of lens design on corneal power distribution in orthokeratology. Optom Vis Sci. 2022 Apr 1;99:363-371.
- Chen XH, Xiong Y, Wang JL, Yang B, Liu LQ. Prospective Study on Corneal Safety Evaluation of Children/Adolescents with Low and Moderate Myopia after Long-Term Orthokeratology]. Sichuan Da Xue Bao Yi Xue Ban. 2021 Nov;52:1006-1010.
- Bian Z, Xu X, Chen D, Ni H. Assessment of patient compliance in orthokeratology and analysis of influencing factors: a cross-sectional study. BMC Ophthalmol. 2021 Nov 16;21:396.
- Lipson MJ. The role of orthokeratology in myopia management. Eye Contact Lens. 2022 May 1;48:189-193.
- Rhee MK. Update on myopia control: The US perspective. Eye Contact Lens. 2022 Mar 1;48:105-109.
- Ji N, Niu Y, Qin J, Fu A-C, Cui C. Orthokeratology Lenses Versus Administration of 0.01% Atropine Eye Drops for Axial Length Elongation in Children With Myopic Anisometropia. Eye Contact Len. 2022 Jan 1;48:45-50.
- Jones JH, Mutti DO, Jones-Jordan LA, Walline JJ. Effect of combining 0.01% Atropine with soft multifocal contact lenses on myopia progression in children. Optom Vis Sci. 2022 May 1;99:434-442.
- Michaud L, Resnick S. Scleral lenses versus corneal GP lenses. Contact Lens Spectrum. 2022 Aug;37:32-38.
- Gelles JD, Cheung B, Akilov S, et al. Ocular impression-based scleral lens with wavefront-guided optics for visual improvement in keratoconus. Eye Contact Lens. 2022 Jul 29. [Online ahead of print]
- Baudin F, Chemaly A, Arnould L, et al. Quality-of-life improvement after scleral lens fitting in patients with keratoconus. Eye Contact Lens. 2021 Sep 1;47:520-525.
- Yehezkeli V, Hare I, Moisseiev E, Assia EI, Chacham I, Ela-Dalman N. Assessment of long-term visual outcomes in aphakic children wearing scleral contact lenses. Eye (Lond). 2022 Jan 31. [Online ahead of print]
- Villa M, Cavas F, Piñero DP. Optical impact of corneal clearance in healthy eyes fitted with scleral contact lenses: A pilot study. J Clin Med. 2022 Jun 14;11:3424.
- Scanzera A, Deeley M, Joslin C, et al. Contact lens prescribing trends for keratoconus at an academic medical center: Increased utilization of scleral lenses for severe disease. Eye Contact Lens. 2022 Feb;48:58-62.
- Itoi M, Itoi M. Management of Keratoconus With Corneal Rigid Gas-Permeable Contact Lenses. Eye Contact Lens. 2022 Mar 1;48:110-114.
- Santodomingo-Rubido J, Carracedo G, Suzaki A, Villa-Collar C, Vincent SJ, Wolffsohn JS. Keratoconus: An updated review. Cont Lens Anterior Eye. 2022 Jun;45:101559.
- Isik P, Harbiyeli II, Erdem E, Yagmur M. Improved contact lens fitting after corneal cross-linking in eyes with progressive keratoconus. Cont Lens Anterior Eye. 2022 Jun;45:101488.
- Koh S, Inoue R, Maeno S, et al. Characteristics of Higher-Order Aberrations in Different Stages of Keratoconus. Eye Contact Lens. 2022 Jun 1;10:256-260.
- Rodriguez GC. Visual Quality of Decentered-Optic Multifocal Scleral Lens Design. Presented at the Global Specialty Lens Symposium, Las Vegas, January 2022.
- Davis RL, Schwartz M. Custom soft lenses: Expand Your Fitting Options. Contact Lens Spectrum 2021 Oct;36:38-42.
- Rojas-Viñuela J, Frogozo MJ, Piñero DP. What we know about the scleral profile and its impact on contact lens fitting. Clin Exp Optom. 2022 Jul 11:1-14. [Online ahead of print]
- Fuller DG. Specialty Scleral Lens Designs and Applications. Contact Lens Spectrum. 202 Feb2;37:28-33.
- Kauffman M. 21st Century Correction of Presbyopia. Contact Lens Spectrum. 2022 Jun;37:20-24.
- Johnson & Johnson Vision Care. Johnson & Johnson Vision Care Receives FDA Approval for ACUVUE® Theravision™ with Ketotifen – World’s First and Only Drug-Eluting Contact Lens. News Release. 2022 Mar 2.




