Corneal topography is, without a doubt, a critical piece of diagnostic data that specialty contact lens fitters use to guide decision-making. There are times when the practitioner is unable to obtain this information; yet, it is still possible to proceed with a specialty lens fit.
Situations that can make obtaining topography difficult may include when patients are unable to hold fixation (as in nystagmus) or maintain upright or stable positioning in the instrument itself, advanced corneal disease that creates difficulty in image capture and analysis, severe ocular surface disease, very narrow palpebral apertures, equipment malfunction, or simply a lack of this technology in a new and/or growing practice.
Despite these numerous potential situations, measuring corneal topography should be achievable on most specialty lens candidates and every attempt should be made to do so when possible. If the patient does not have underlying issues preventing it, but the fitting practitioner’s equipment does not suffice, a local colleague could be asked to provide this measurement, with or without billing, for interpretation. Requesting records from any prior lens fits and practitioners can be invaluable in providing a better starting point for lens design.
Understanding the underlying corneal condition is critical if actual shape cannot be mapped. It is very helpful to measure corneal diameter, and this can often be done with a handheld ruler with reasonable accuracy. External photography or videography can be useful when working with consultants to provide the most accurate visual descriptions during the fitting process. Options to make some of these fits easier include piggybacking and scleral lenses, both of which can reduce the complexity required for corneal GP lenses in fitting the corneal surface.
Figure 1 is an example of a patient for whom corneal topography could not be acquired. This patient has congenital aniridia, macular hypoplasia, and nystagmus, and is aphakic. She has an epikeratophakic graft OS that is more than 30 years old. She is monocular and has a prosthetic eye OD. Scleral lenses were previously worn but were deemed uncomfortable and carry a greater risk of hypoxia and worsening corneal neovascularization.
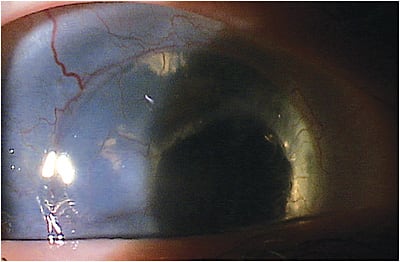
External videography was done and a still photo was extracted for consultation. Corneal GP lenses were fit very steeply, as would be expected with this type of graft, and the diameter was designed to avoid issues at the junction of the graft and the host cornea.
A fit of this nature can be particularly challenging, requiring multiple lens remakes and exchanges, and it is important to understand the chosen laboratory’s lens warranties and exchange policies. It needs to be well documented when a fit begins (and specifically when the first lens is ordered), how many exchanges are allowed, how long the warranty period will last, and what shipping costs will be.
Costs can add up quickly when lens remakes are required beyond the allowable exchange period, and decisions regarding who is responsible for covering these costs are difficult. However, fitting without topography is not an insurmountable task, and can be very rewarding for both patients and practitioners. CLS




