Interest in specialty contact lens fitting, particularly with scleral and orthokeratology lenses, continues to grow significantly among eyecare practitioners. Whether it is the joy of providing life-changing lenses to patients or the slowing of myopia progression in a child, today’s specialty lenses are improving the quality of life of patients and prescribers.
Providing the best possible fit to achieve the best comfort and vision correction requires an understanding of both the ocular surface shape and the design of the lenses that are utilized. Over the last several years, instrumentation has been developed and has evolved to give us more information about the shape of the ocular surface. Modern instruments can measure more surface area, and in better detail, than previous imaging devices could. This new information about the shape of the eye in general, and each individual patient specifically, allows us to not have to settle for fits that are “acceptable,” but instead to target “optimal” fits.
INSTRUMENTATION
There are two types of instruments that are used to capture ocular surface shape data: those that are reflection-based and those that are Scheimpflug-based. There are also differences in the number of captures used and how they obtain their maximum data. Finally, there are also differences in how each instrument integrates with lens design applications, impacting their utilization to the specialty lens fitter. These differences will lead some practitioners to favor one instrument over another, but they all provide meaningful data and the opportunity to create great contact lens fits.
Reflection-based systems require the use of fluorescein to capture data. This is due to the poor reflectivity of the sclera. Based upon the author’s experience, a reflection-based system is most effective with a slight amount of lubricant added first, then a generous amount of fluorescein. It is vital to cover as much of the ocular surface with dye as possible, as the unit will only capture data where there is adequate fluorescein to reflect. The unit then reflects a cobalt blue grid over the ocular surface to obtain the shape data for processing (Figure 1).

Scheimpflug-based imaging systems do not require fluorescein to be added to the eye because they are not reflection based. A Scheimpflug-based system takes cross-sectional measurements along a chord of the eye, typically rotating around a central point. A scan of 25 to 50 chords takes about three to four seconds, providing cross-sectional data along each axis of the scans. These data are then used to create a data map, either for the cornea (one scan) or for the entire ocular surface (multiple scans).
Regardless of the imaging method used when obtaining scans, it is vital to look at results with a critical eye for quality, accuracy, and repeatability. Any inaccurate information obtained from maps to help with lens fitting will lead to poor initial outcomes. Artifacts in a reflection-based scan can arise from drying of the surface, excessively heavy lubrication, mucus, debris in the tear layer, or inadequate fluorescence (Figure 2).
With a Scheimpflug-based system, inaccuracies can occur when scans are improperly aligned, there is eyelid obstruction, or there is movement of the eye during the three- to four-second scan time. After image capture, assessing scans for smooth transitions in shape, for shape changes consistent with what is visible with a slit lamp, and for lack of “gaps” or extrapolation is important. It is advisable, when scanning an eye for shape prior to orthokeratology or scleral lens fitting, to obtain the best images possible, as you may not have the ability to obtain them in the future without the patient “washing out of” contact lens wear, a significant inconvenience.
Contact lens washout refers to a discontinuation of contact lens wear. If the patient has been wearing contact lenses of any kind (scleral, soft, or corneal GP), there may be an impact on the ocular shape that will affect the data obtained and possibly alter the results of contact lens fitting (Figure 3). When at all possible, patients should be out of soft or corneal GP lenses at least 12 hours, and at least 36 hours for scleral lenses. If the conjunctiva appears inflamed, as can often be the case when attempting a refit, using a steroid eye drop when appropriate for a few days prior to scanning can also improve the quality and reliability of the scans.

INTERPRETING MAPS
Corneoscleral profile maps can provide a level of understanding that makes contact lens fitting more efficient and successful. Becoming adept at reading maps is the first step in this process. The first point to be clear on is the type of map at which you are looking. Usually, the default display is an elevation map. This is different than most corneal topographers, who usually default to a curvature map. This means that, in general, hotter colors on the elevation map indicate a higher elevation, and therefore a flatter rate of curvature change. Cooler colors indicate a lower elevation or—another way of stating it—a deeper depression, which indicates that the slope to get there is steeper (Figure 4). It is also useful to look for obstacles that can impact the ability to fit a contact lens to predict the on-eye fit, which may require a more sophisticated contact lens design (Figure 5).


It is easy to get so focused on the scleral shape that we neglect to consider the corneal shape. The shape of the cornea is obviously critical to orthokeratology lens fitting but can be vital to a proper scleral fit as well. Some profilometers break the corneal and scleral shape maps into two separate displays, which others superimpose them. However, keep in mind that they are presented on different reference scales (Figure 6).

This is important, as the corneal and scleral shape maps cannot be compared directly. Observe the corneal shape on its own and the scleral shape on its own, but don’t overanalyze what is happening at the junction of the two maps.
USING PROFILOMETRY TO GUIDE OUR SPECIALTY LENS FITTING
There are various ways to use the output from profilometry to guide specialty lens fitting. From simply looking at a few key values prior to beginning a diagnostic fitting to letting an application use the data directly to do the complete design, the data obtained can be used differently for each situation. An advantage of diagnostic fitting is that it is less expensive for the patient, and a large percentage of patients are quite successful with diagnostically fitted contact lenses. For those patients who have a unique eye shape or unusual needs or time constraints, an entirely empirical map-based design can be beneficial.
When it has been determined that a scleral lens should be fitted to one eye or both, scans can be performed on both eyes, assuming that the patient has been out of contact lenses for an adequate period and that the eye does not show any acute concerns that might be affecting the shape. After obtaining maps, the various aspects of the data should be looked at to help decide on a design to fit. The data can be used to help select a diameter; geometry; initial sag; the need for toric, spherical, or quadrant specific curves; and any areas that will need local accommodations.
SELECTING LENS DIAMETER AND GEOMETRY
The first step in a diagnostic scleral lens fitting is to decide on lens diameter and geometry. These decisions should be based primarily on the corneal scan. Knowing the patient’s corneal diameter, a lens can be selected that is large enough to allow the starting point of significant lens bearing to occur beyond the limbal zone by a reasonable amount (I prefer 0.5mm at the closest point) (Figure 7).

Knowing the shape of the patient’s cornea will guide the choice of a lens that has standard geometry or one that has reverse geometry. Standard geometry scleral lenses are more appropriate for normal corneas or keratoconus when the apex is near the center of the cornea. Reverse geometry lenses can be more appropriate for post refractive surgery, eyes that have peripheral elevations (such as Salzmann’s), or pellucid marginal degeneration. Once diameter and general geometry are selected, the next step is to decide specifics about the diagnostic lens, and this is where the profilometer can start to save time and effort.
DETERMINING SAG AND PERIPHERAL CURVES
With a given lens diameter, a profilometer can help determine a starting point for lens sag (Figure 8). The sag will be a factor of the lens diameter and the desired clearance, and this will be a starting point for choosing a diagnostic lens. The other aspect of the lens gained from profilometry maps is the need for spherical, toric, or quadrant-specific peripheries (Figure 9). Select a diagnostic lens that is closest to the suggested lens from the profilometry instrument, place it on the eye, check the lens for minor adjustments to sag and edges, and over-refract. This should be the initial lens order, ready to go from just a single diagnostic lens.


A second approach when there is little time and/or there is a known lens base curve and power is to simply order the lens empirically using the recommended lens parameters or export the recommended parameters to the manufacturer directly (Figures 10 and 11). This can also be helpful when the lens needed is uncommon, and the diagnostic set does not include reasonable options. Quadrant-specific eye shapes and extremely deep or shallow sag values are just two examples of eyes that have uncommon needs, and diagnostic lens sets will not likely have lenses close to the appropriate fit.


USING PROFILOMETRY FOR MORE COMPLEX FITTING
In some instances, a more complex lens design is needed to achieve a good fit. These are instances in which the sclera has local areas of elevation, or the cornea has significant toricity. Using profilometry can assist in localizing the area of elevation as well as measuring its height. In the example in Figure 5, knowing the area of the local elevation allows us to measure the length of the area radially at 2.6mm, as well as the height of that spot at 275 microns.
When the local vault area is built, accommodations for width and height are made without guessing. If using a diagnostic lens on the eye, lens rotation should be noted and accounted for in placing the vault where needed. If designing the lens empirically, it can be noted that the area of localized vault is near the center of the steepest meridian. Thus, the profilometry map of the eye allows for highly specific design of local vaults.
Some eyes have high degrees of toricity that can create problems with obtaining good alignment of the scleral zone to the eye. Using profilometry, it is possible to measure the differences in elevation in a highly toric eye and build that toricity into the contact lens in the appropriate fashion. This provides better lens centration and less risk of debris accumulation under the lens.
To determine whether the amount of toricity in the cornea will impact fit, use the chord diameter of the landing point of the particular scleral lens being fitted (obtained from the manufacturer) and measure the difference in elevation at this point. This is illustrated in the following case.
A 32-year-old female presented for contact lens fitting. She reported having trouble with soft toric lenses in the past, mainly due to stability of vision and dryness. Her refraction revealed mixed astigmatism of approximately 2DC OD and OS. After discussing contact lens options including soft toric lenses, corneal GP lenses, and scleral lenses, she opted to try scleral lenses. Based on her corneal shape and diameter, it was decided to fit a standard geometry, 17mm overall diameter lens. Realizing she had significant scleral toricity, she was fitted in a toric periphery lens OD and OS, with 570 microns of toricity in the left lens (Figure 12).

The lenses as ordered demonstrated significant decentration along the steep axis of the eye OD and OS. They also had edge lift and minimal limbal clearance superiorly. Looking back at the profilometry maps and looking further into the toricity of the eye, it was clear that much of the toricity came from the corneolimbal zone, and the lenses did not account for that (Figure 13). The lenses were redesigned to add 250 microns of toricity to the internal lens curves where the lens was vaulting the cornea and limbus, and 300 microns of toricity in the scleral zone, much more in line with the true shape of the left eye. This lens provided a much more acceptable fit with better centration and scleral alignment, as well as comfort for the patient (Figure 14).


FULLY CUSTOMIZED, MAP-DRIVEN LENSES
Another approach to scleral lens fitting using profilometry is to export the map and have an application do the entire lens design in a completely custom manner. This requires a very high-quality map with the best possible data. When eyes are more complex in shape, time is at a premium, or diagnostic fitting is not producing the desired outcome, an application-based custom design can provide a better outcome for some patients. The cost of the lens is a downside in some cases. To create an application-driven lens design, ensure that the patient is out of all contact lenses for an appropriate period of time, because any data artifacts will result in an inaccurate lens.
Once an optimal map is obtained, upload or export the map and the software will create an initial lens design. Order the initial lens without making any adjustments, simply by providing the lens power data (power adjusted for base curve changes versus prior lenses). These apps then allow you, with or without help from consultation, to go back and make adjustments at the follow-up visit if needed. An example of an application-based fit follows below.
A 57-year-old female presented for a scleral lens follow-up visit. She had been wearing scleral lenses for three years for keratoconus and was happy with her right eye but reported ongoing issues with fogging of the left lens.
Despite efforts to refit with adjustments to the edge profile, debris continued to accumulate at 1 o’clock and couldn’t be resolved to the patient’s satisfaction.
A custom lens design was offered and the patient consented to being refit in this modality after discontinuing her previous contact lens for three days prior to repeating her profilometry.
The scleral map demonstrated an obviously elevated temporal sector and a quadrant-specific scleral shape (Figure 15). A custom, free-form lens was created by exporting the map into proprietary software, using the base curve and power from her prior scleral lens. The lens was dispensed two weeks later with excellent results. The patient’s comfort and vision surpassed that of her prior lens, and the debris issue was resolved (Figure 16).


LENS DESIGN AND PROFILOMETRY: BEYOND SCLERAL LENSES
While scleral lens design is the biggest area of profilometry utilization, there are more applications being introduced for orthokeratology lens designs as well. Because the profilometer measures corneal and scleral shapes and is able to define the borders of the cornea so as to capture full corneal data, profilometer-based software can be used to empirically fit orthokeratology lenses.
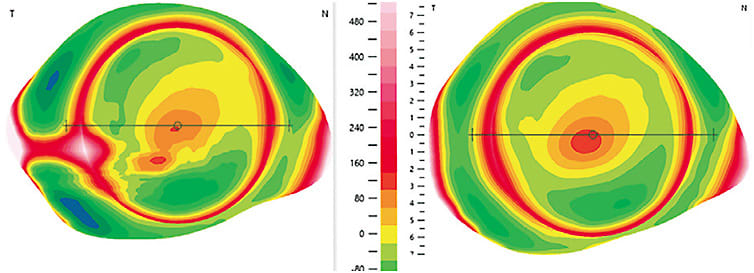
This capability of profilometers allows for highly specific orthokeratology lens fitting, helping to define the ideal lens diameter for the patient’s corneal size and determine the need for toricity in the zones of an orthokeratology lens (Figure 17). Adding the patient’s Rx also allows for calculation of the lens base curve, giving the practitioner a complete set of lens parameters optimized from the profilometry.

Profilometry provides a better understanding of the shape of the eyes of our specialty lens patients. These data improve efficiency in fitting specialty lenses and provide better outcomes, no matter which strategy is employed. They allow eyecare practitioners to prescribe more advanced designs, with less chair time, for the more complex patient. Profilometry truly is a win for everyone involved in the process of fitting specialty contact lenses. CLS




