THE ROLE OF the iris is to regulate the amount of light that enters the eye, while its muscles are responsible for controlling the size of the pupil. It reduces aberrations from the lens and cornea by decreasing the amount of light entering the pupil, preventing excessive glare, and enhancing depth of focus, thus enhancing the quality of vision (Gurnani and Kaur, 2023).
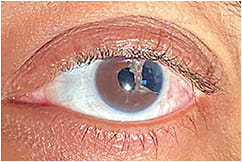
If the iris is damaged, tissue may end up missing, causing polycoria, or the iris muscles may cease to work, resulting in an enlarged, irregular, or poorly reactive pupil. Iris defects typically cause visual impairment due to increased photophobia, glare, and decreased contrast sensitivity, as well as cosmetic disfigurement (Mayer et al, 2017).
These defects can arise due to congenital reasons or are acquired through trauma or surgery. Prosthetic colored soft contact lenses can be a viable option, especially when surgical intervention is undesired or too risky (Migneco, 2005). There are three main types of prosthetic colored contact lenses: translucent tinted, computer generated, and hand painted.
Translucent tinted lenses are usually indicated for patients who want to augment their natural eye color or enhance their color perception (especially athletes or patients who have color deficiencies) (Yeung and Wong, 2020). They can also be used to decrease light transmission for patients who are photophobic (Schornack et al, 2007). These lenses have a uniform hue and can be customized to have clear, translucent tinted or black pupils.
These lenses can mask mild disfigurements and partial iris defects in those who have dark irises, but the pigment is generally not dense enough to block peripheral light transmission and reconstruct a significant amount of abnormal iris (unless using a total black annular ring). The color, iris diameter, shade of tint, and pupillary diameter can be customized, but iris and corneal details cannot.
Computer-generated or hand-painted lenses usually are the best option for patients who need prosthetic lenses to mask large iris defects because they allow the use of an opaque underprint to significantly block peripheral light and form a specific pupillary diameter.
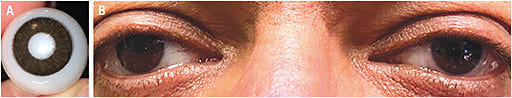
Computer-generated lenses allow for an array of colors and patterns generated by dot-matrix printing. To provide a realistic look, many designs allow for layering of different colors and/or including iris details such as limbal rings and pupillary frills. Various colors of opaque underprints are available to provide full iris occlusion; however, the underprint color can impact the perceived color and iris detail of the front surface. These underprints are reproducible with good consistency and don’t fade.
Hand-painted lenses offer a customizable appearance and are the most expensive, requiring more time for fitting and manufacturing. Intricate ocular details (iris flecks, coronas, limbal rings, and vasculature) can be added. This option allows for decentration to improve symmetry with the other eye. They are impossible to 100% reproduce and can fade over time, especially if the manufacturer’s cleaning recommendations aren’t followed.
This option is useful for patients who have iris defects and want the most natural look and best color match, especially those who have lighter colored irises and who need an opaque underprint for full iris reformation. CLS
References
- Gurnani B, Kaur K. Traumatic Iris Reconstruction. StatPearls [Internet]. StatPearls Publishing, 2023 May 4.
- Mayer C, Tandogan T, Hoffman AE, Khoramnia R. Artificial iris implantation in various iris defects and lens conditions. J Cataract Refract Surg. 2017 Jun;43:724-731.
- Migneco MK. Contact lens management of aniseikonia and photophobia induced by trauma. Eye Contact Lens. 2005 Nov;31:252-253.
- Yeung KK, Wong R. Colored Contact Lenses: More than a Pretty Eye. Rev Cornea Contact Lens. 2020 Feb 15. Available at reviewofcontactlenses.com/article/colored-contacts-more-than-a-pretty-eye . Accessed June 13, 2023.
- Schornack MM, Brown WL, Siemsen DW. The use of tinted contact lenses in the management of achromatopsia. Optometry. 2007 Jan;78:17-22.




