History
A 37-year-old African American male was referred for a second opinion on his scleral lenses. He was diagnosed with keratoconus in 2011 and used corneal GP lenses for four years. He switched to scleral lenses after breaking too many GP lenses and has been wearing sclerals for about three years with an average daily wear time of 16 hours.
Exam Findings
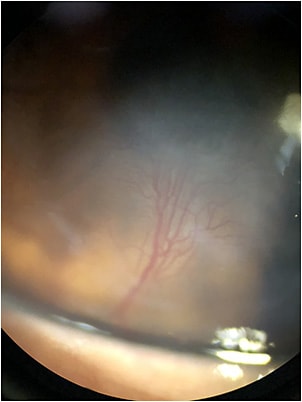
Visual acuities with scleral lenses were reduced at distance to 20/70 OD and 20/200 OS. The scleral lenses showed a nonoptimal fit with 429μm of central clearance on the right eye and central touch on the left. Moderate peripheral corneal vascularization of the right and severe central vascularization of the left eye was observed. The left cornea can be seen in Figure 1 and Video 1.
The patient’s scleral lenses were refit and the material was changed to a hyper-Dk material. The sagittal depth in the right eye was reduced while it was increased for the left eye. After two months, the patient’s vision increased to 20/60 in the right eye

Discussion
Oxygen permeability and transmissibility are important parameters of contact lenses that are often ignored. A higher Dk value is desirable and allows more oxygen to the cornea reducing hypoxic conditions. Due to the advances in contact lens materials, corneal vascularization is not as frequent as before.1
However, patients who are reliant on contact lenses for optimal vision may wear their contacts for much longer than the average person. Coupling a low-Dk material with an improper fit and extended wear time can cause vascularization of the cornea and reduced vision. An improved fit and material will result in halting new blood vessel growth and ghost vessel sequalae.2
Conclusion
This patient had reduced vision due to his combined keratoconus, corneal scarring, and neovascularization. While we cannot completely clear the cornea with higher-Dk lenses due to the ghost vessels, this may improve vision and reduce the likelihood of future progressive vision loss.
References
1. Sweeney DF. Have silicone hydrogel lenses eliminated hypoxia? Eye Contact Lens. 2013 Jan;39:53-60.
2. Chan WK, Weissman BA. Corneal pannus associated with contact lens wear. Am J Ophthalmol. 1996 May;121:540-546.



