
THE SHAPE OF the anterior ocular surface is a primary consideration in scleral lens design and fitting. The cornea, bulbar conjunctiva, and sclera are the anatomical tissues that determine the surface shape of the eye. This article will review current understandings of corneoscleral shape (CSS) and how it impacts scleral lens fitting.

CORNEA
The cornea is a transparent, avascular tissue that is composed of five layers and provides approximately two-thirds of the eye’s optical power. Computerized videokeratography, anterior segment optical coherence tomography (AS-OCT), and Scheimpflug tomography have revolutionized the ability to measure and assess the cornea. The cornea is prolate in geometry and has an oval shape with the horizontal diameter typically larger than the vertical diameter.1 Corneal toricity is defined as unequal curvature of the perpendicular meridians that is influenced by genetics, eyelid pressure, and the extraocular muscles.2,3
Ectasias of the cornea, such as in keratoconus, increases keratometry dioptric values and irregular astigmatism.4 The geometry of the cornea changes from prolate to oblate after myopic refractive surgery and in some cases of penetrating keratoplasty. Corneal scarring and trauma can result in significant irregularity of the corneal surface.
Corneal diameter is an important consideration for scleral lens fitting. Horizontal diameters greater than 12.4mm can result in insufficient limbal vault. Compression of the corneal limbus will result in limbal keratitis and vascularization. Depending on the scleral lens design, increasing the lens diameter may be necessary to achieve proper corneal clearance for eyes that have relatively large corneal diameters.
A difference of greater than 0.5mm between the horizontal and vertical diameters can be clinically relevant for a scleral lens fit,5 as it can result in excessive superior and inferior limbal vault that leads to midday fogging and conjunctival prolapse.6,7 In this case, an oval optic zone that matches the diameter difference should be considered to achieve an even circumferential clearance. Although most scleral designs utilize prolate corneal zone geometries, oblate designs will achieve a more even fluid reservoir for postsurgical corneas with oblate profiles.
CORNEOSCLERAL JUNCTION
The 1.5mm to 2mm transition zone between the cornea and sclera is termed the corneoscleral junction (CSJ).8 Although it had been popularly thought that the CSJ was curved, van der Worp and colleagues demonstrated that the CSJ is, in fact, tangential.9
These findings have been validated by numerous studies examining the CSJ profile.8,10,11 In a study of 204 subjects, Hall and co-workers using AS-OCT measurements found that 77% of CSJ angles were within 5° of 180° and 20% were within 1°.10 The mean CSJ angle was 173° horizontally and 178.3° vertically. Using corneoscleral topography measurements of the right eyes of 105 healthy subjects, Consejo and colleagues found a group mean CSJ angle of 177.5° with rotational asymmetry where the nasal region was steeper as compared to the rest of the sectors.8
The tangential profile of the CSJ is an important consideration for scleral lens design. Van der Worp and colleagues had originally suggested that scleral lens designs should use tangential rather than curved profiles.9,12 Scleral lenses that have a curved limbal zone can result in excessive limbal clearance, which can cause midday fogging.
Another study reported that there was a greater proportion of eyes that had excessive limbal clearance that experienced midday fogging (57%) compared to eyes without midday fogging (11%).7 Therefore, a scleral lens that has a tangent limbal zone design will have a lower clearance of the paralimbus, possibly decreasing clinical signs and symptoms of midday fogging.
SCLERA/BULBAR CONJUNCTIVA
The sclera covers more than 80% of the eye surface and is composed of collagen fibrils that have an irregular arrangement.13 Recent advancements in instrument and software technology have improved our understanding of scleral shape.
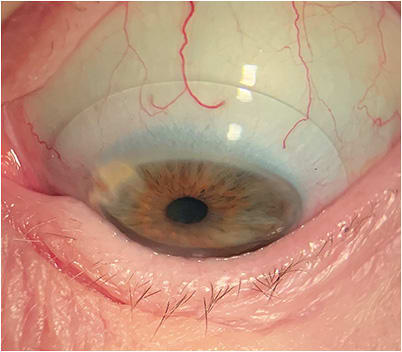
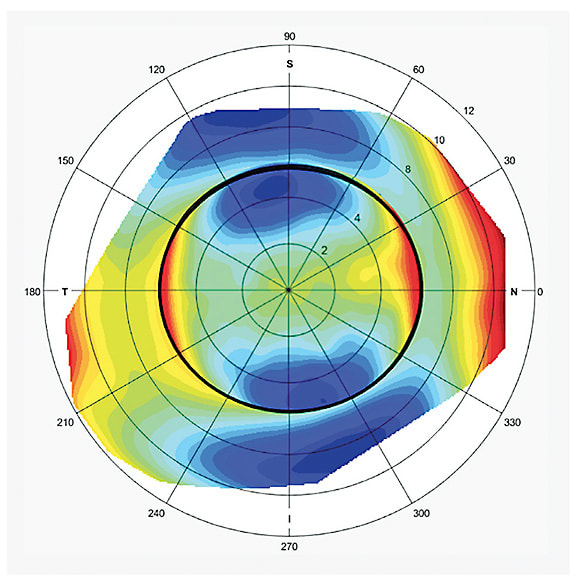
Typically, the anterior scleral surface is tangential and nonspherical in shape.9 The temporal scleral surface is significantly steeper than nasally with limited variation between the nasal, superior, and inferior quadrants14,15 (Figure 1).

This anatomical anomaly has been theorized to be a consequence of the spiral of Tillaux, which describes the location of attachment differences of the extraocular muscles.5,11 Measured from the limbus, the measurements of muscle insertion are 7.0mm (lateral rectus), 7.5mm (superior rectus), 6.5mm (inferior rectus), and 5.0mm (medial rectus).9
Differences in scleral sagittal heights of two perpendicular meridians results in scleral toricity, which averages 100 to 200 microns at a 15mm chord and increases in magnitude with increasing chord values.15 Scleral shapes that are either spherical or toric are rotationally symmetric while asymmetric scleral shapes are non-rotationally symmetric.5
The bulbar conjunctiva is a transparent tissue covering the sclera that is loosely attached to Tenon’s capsule. The stroma of the conjunctiva contains blood vessels, nerves, and mucin-producing goblet cells.16,17 The conjunctiva functions to provide ocular surface lubrication, mechanical protection, and immune defense.15 The average thickness of the conjunctiva is 240 microns and decreases with age.18 The nasal conjunctiva (270 microns) is, on average, thicker than the temporal conjunctiva (249 microns).19
The spongy conjunctival tissue acts as a cushion for the scleral lens landing zone, which helps to accommodate a mild mismatch between the landing zone of a scleral lens and the ocular surface. The landing zone of a scleral lens settles into the conjunctiva during lens wear, which results in a temporary flattening of its shape, which can be unequal after lens removal.20-22
Two studies reported that conjunctival indentation from short-term scleral lens removal did not return to baseline three hours post lens removal.20,21 These studies show a 70% to 77% return to baseline during this period.
Although it isn’t known how long it takes for complete conjunctival rebound after scleral lens use, it is recommended that current scleral lens wearers stay out of their lenses for two to three days prior to a scheduled scleral lens fitting to avoid inaccurate shape assessment during the design process. It is possible that there can be permanent architectural changes to the conjunctiva after long-term wear of an overly compressed scleral lens.
A pinguecula, which is a common yellow raised growth on the interpalpebral nasal or temporal conjunctiva, contributes to surface asymmetry when elevated more than 100 to 200 microns.23 Conjunctival blebs secondary to trabeculectomy or shunt surgeries for glaucoma result in significant localized elevation changes and asymmetric changes to the ocular surface.
The Scleral Shape Study Group (SSSG) devised a classification system to categorize scleral shape patterns.24 The study evaluated 140 eyes of prospective scleral lens patients who had undergone corneoscleral topography. Four scleral shape patterns were determined utilizing a circumferential shape plot at a 16mm chord.
The results were as follows: Group 1 were spherical scleras (5.7% of eyes), defined as having a plot with low amplitude deviations of ≤ 300 microns. Group 2 were regular toric scleras (28.6% of eyes), defined as having a sagittal height plot with a sin2 pattern, periodicity of 180°, and greater than a 300-micron difference between highest and lowest depressions. The largest category was group 3, asymmetric scleras (40.7% of eyes), which had plot asymmetries of > 300 microns. Group 4 (25% of eyes) had a sagittal height plot with a repeating sin2 pattern, but a periodicity different from 180°.
This classification system is a reference for practitioners to use when considering scleral lens design. Fewer than 10% of eyes would be best fit utilizing a spherical landing zone, whereas the majority of patients would be best fit with a landing zone that is more customized than a spherical landing zone.
Clinically, 100-micron differences have been reported to be significant when matching the landing zone design with scleral shape.5 Therefore, an eye could be categorized as toric but exhibit 100 to 200 microns of localized asymmetry, which affects a scleral lens fit. For example, a scleral lens that has a toric landing zone that matches scleral toricity could have a localized vault to avoid impingement of a peripherally located nasal pinguecula.
As mentioned, the anterior scleral surface is tangent in profile. A tangent design landing zone that continues from the limbal zone of the lens design will reduce bearing and potential conjunctival compression (Figure 2). Visser and colleagues reported on a tangential designed scleral lens that gently positioned on the scleral surface, increasing fitting tolerance.12 The bitangential design used for 213 eyes achieved successful fits that resulted in high comfort scores.
CORNEAL AND SCLERAL TORICITY
When considering a possible relation between corneal and scleral shapes, some studies have suggested that there is a relationship between corneal and scleral toricity when astigmatism is > 2.00D.11,25 Another study measured a cohort of healthy eyes using corneoscleral topography and found that corneal toricity seems to “follow” scleral toricity in eyes with astigmatism.26 The authors therefore suggest that astigmatism is not restricted to the cornea but should be considered to affect the entire ocular surface.
Furthermore, they hypothesize that the sclera influences corneal astigmatism as a result of the sclera’s relative increased rigidity. Corneal astigmatic changes have been reported after ocular surgeries, including cataract surgery, trabeculectomy, and scleral buckle for retinal detachment.26
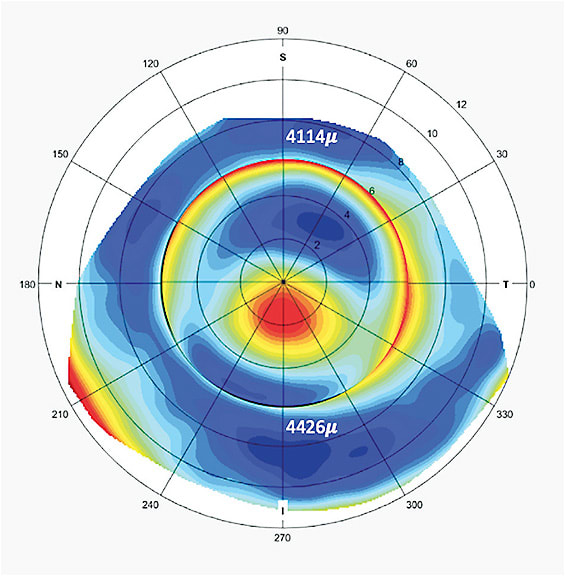
Clinically, scleral toricity and the need to utilize a toric landing zone could be predicted for eyes that have astigmatism and corneal toricity. Figure 3 represents the corneoscleral topography of a patient’s left eye that has high amounts of corneal toricity. The surrounding elevation map of the sclera demonstrates a continuation of the toricity from the cornea. For these cases, the toricity of the landing zone that extends into the limbal region can improve even circumferential limbal vault.
SCLERAL SHAPE AND KERATOCONUS
Recent research has shown a definitive relation between corneal and scleral shape in the keratoconic eye. Pinero and co-workers reported on a corneoscleral analysis of a keratoconus population and found that their scleral profiles had higher levels of asymmetry compared to healthy eyes, especially eyes with moderate-to-advanced keratoconus.27
A retrospective study by SSSG found increases in scleral toricity and asymmetry for eyes with ectasia compared with normal eyes.28 The 227 eyes that had ectasia were subdivided into central ectasia and peripheral ectasia using measurements from corneoscleral topography. The mean scleral toricity measurements were as follows: normal cornea 172 microns, central ectasia 210 microns, and peripheral ectasia 220 microns. Additionally, sagittal height measurements were taken at a 16mm chord of the sclera at the same axis of corneal ectasia and at a position 180° away.
Differences in sagittal heights between these locations were considered a quadrant-specific effect with the following values: normal corneas 17 microns, central ectasia 66 microns, and peripheral ectasias 289 microns (Figure 4). Specifically, the sclera was steepest in the same semi-meridian as the corneal apex.
These findings were validated in a study by Dhaese and colleagues in which investigators evaluated 20 eyes of 17 subjects who had keratoconus. Using corneoscleral topography, the study found that the steepest regions of the central cornea, peripheral cornea, and sclera tended to share a common angle.29
Clinically these findings are important when designing a landing zone for the keratoconus eye. On average, the landing zone will need approximately 200 microns of toricity for the typical patient who has ectasia. However, a quadrant-specific steepening of the landing zone in the same semi-meridian as the corneal apex will often be necessary to optimize the lens fit. Failure to utilize a quadrant-specific design, when necessary, can result in lens decentration; the majority of the time it will decenter inferiorly.28
The relationship between the position of the corneal apex and scleral asymmetry demonstrates a possible interconnectedness of these two tissues, as has been reported with toricity.26 Pinero and colleagues have suggested that for keratoconus, the mechanical weakening of the cornea due to collagen disruption causes the corneoscleral profile to rise in areas opposite the ectasia and decrease in areas that are proximal.27
Scleral shape can change after crosslinking or corneal hydrops. There is, at minimum, one published study of a patient who had a change in scleral shape three months after corneal crosslinking that was significant enough to require a refitting of his scleral lens for the affected eye.30 DeNaeyer and colleagues reported on a case series of keratoconus patients who had corneoscleral topography measurements before and after hydrops in which one patient had an increase in both corneal and scleral irregularity.31
CONCLUSION
Numerous advances in instrumentation and software have expanded our knowledge of corneoscleral shape, which has significantly improved scleral lens design and fitting success. An adequate and even fluid reservoir of a fit scleral lens is achieved by matching the geometry of the cornea, either prolate or oblate, with the corneal zone design of a scleral lens.
Tangent profile limbal and landing zones will contour to the natural slope of the scleral surface, minimizing excessive limbal clearance and conjunctival compression. The majority of scleral shapes are best fit using toric, quadrant-specific, or free-form landing zones.
Scleral toricity can be predicted for eyes with astigmatism that have limbal-to-limbal toricity, as toricity in these cases extends beyond the cornea to the scleral surface. Keratoconic eyes can have predicted scleral steepness in the same semi-meridian in the case of peripheral ectasia, and consequently will be best fit with a quadrant-specific or free-form lens design. CLS
References
- Khng C, Osher RH. Evaluation of the relationship between corneal diameter and lens diameter. J Cataract Refract Surg. 2008 Mar;34:475-479.
- Read SA, Collins MJ, Carney LG. A review of astigmatism and its possible genesis. Clin Exp Optom. 2007 Jan;90:5-19.
- Denisova K, Barmettler A. Oculoplastic considerations for refractive procedures. Curr Opin Ophthalmol. 2020 Jul;31:241-246.
- Ferdi AC, Nguyen V, Gore DM, Allan BD, Rozema JJ, Watson SL. Keratoconus Natural Progression: A Systematic Review and Meta-analysis of 11 529 Eyes. Ophthalmology. 2019 Jul;126:935-945.
- Fadel D. The influence of limbal and scleral shape on scleral lens design. Cont Lens Anterior Eye. 2018 Aug;41:321-328.
- Fadel D. Scleral Lens Issues and Complications Related to a Non-optimal Fitting Relationship Between the Lens and Ocular Surface. Eye Contact Lens. 2019 May;45:152-163.
- Walker MK, Bailey LS, Basso KB, Redfern RR. Nonpolar Lipids Contribute to Midday Fogging During Scleral Lens Wear. Invest Ophthalmol Vis Sci. 2023 Jan;64:7.
- Consejo A, Rojas-Viñuela J, Sebastian-Carmona J, Ezpeleta J, Piñero DP. Corneoscleral junction angle in healthy eyes assessed objectively. Cont Lens Anterior Eye. 2023 Jan;46:101815.
- Van der Worp E, Graf T, Caroline PJ. Exploring Beyond the Corneal Borders. Contact Lens Spectrum. 2010 Jun;25:26-32.
- Hall LA, Hunt C, Young G, Wolffsohn J. Factors affecting corneoscleral topography. Invest Ophthalmol Vis Sci. 2013 May 1;54:3691-3701.
- Ritzmann M, Caroline PJ, Börret R, Korszen E. An analysis of anterior scleral shape and its role in the design and fitting of scleral contact lenses. Cont Lens Anterior Eye. 2018 Apr;41:205-213.
- Visser ES, Van der Linden BJ, Otten HM, Van der Lelij A, Visser R. Medical applications and outcomes of bitangential scleral lenses. Optom Vis Sci. 2013 Oct;90:1078-1085.
- Bataille L, Piñero DP. Characterization of the geometric properties of the sclero-conjunctival structure: a review. Int J Ophthalmol. 2020 Sep;13:1484-1492.
- Consejo A, Llorens-Quintana C, Bartuzel MM, Iskander DR, Rozema JJ. Rotation asymmetry of the human sclera. Acta Ophthalmol. 2019 Mar;97:266-270.
- Walker MK, Schornack MM, Vincent SJ. Anatomical and physiological considerations in scleral lens wear: Conjunctiva and sclera. Cont Lens Anterior Eye. 2020 Dec;43:517-528.
- Shumway CL, Motlagh M, Wade M. Anatomy, Head and Neck, Eye Conjunctiva. In StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. 2023 Jan.
- DeNaeyer GW. Scleral lenses and the conjunctiva. Contact Lens Spectrum. 2014 Jan;29:48.
- Zhang X, Li X, Xiang M, et al. Bulbar conjunctival thickness measurements with optical coherence tomography in healthy Chinese subjects. Invest Ophthalmol Vis Sci. 2013 Jul 12;54:4705-4709.
- Read SA, Alonso-Caneiro D, Vincent SJ, et al. Anterior eye tissue morphology: Scleral and conjunctival thickness in children and young adults. Sci Rep. 2016 Sep 20;6:33796.
- Alonso-Caneiro D, Vincent SJ, Collins MJ. Morphological changes in the conjunctiva, episclera and sclera following short-term miniscleral contact lens wear in rigid lens neophytes. Cont Lens Anterior Eye. 2016 Feb;39:53-61.
- Consejo A, Behaegel J, Van Hoey M, Wolffsohn JS, Rozema JJ, Iskander DR. Anterior eye surface changes following miniscleral contact lens wear. Cont Lens Anterior Eye. 2019 Feb;42:70-74.
- Macedo-de-Araújo RJ, van der Worp E, González-Méijome JM. In vivo assessment of the anterior scleral contour assisted by automatic profilometry and changes in conjunctival shape after miniscleral contact lens fitting. J Optom. 2019 Apr-Jun;12:131-140.
- DeNaeyer GW. Pingueculitis and Scleral Lens Wear. Contact Lens Spectrum. 2022 Sep;37:52.
- DeNaeyer G, Sanders D, van der Worp E, Jedlicka J, Michaud L, Morrison S. Qualitative Assessment of Scleral Shape Patterns Using a New Wide Field Ocular Surface Elevation Topographer: The SSSG Study. JCLRS. 2017 Nov;1:12-22.
- Macedo-de-Araújo RJ, Amorim-de-Sousa A, Queirós A, van der Worp E, González-Méijome JM. Relationship of placido corneal topography data with scleral lens fitting parameters. Cont Lens Anterior Eye. 2019 Feb;42:20-27.
- Consejo A, Rozema JJ. Scleral Shape and Its Correlations With Corneal Astigmatism. Cornea. 2018 Aug;37:1047-1052.
- Piñero DP, Martínez-Abad A, Soto-Negro R, et al. Differences in corneo-scleral topographic profile between healthy and keratoconus corneas. Cont Lens Anterior Eye. 2019 Feb;42:75-84.
- DeNaeyer G, Sanders DR, Michaud L, et al. Correlation of Corneal and Scleral Topography in Cases with Ectasias and Normal Corneas: The SSSG Study. JCLRS. 2019 May;3:10-20.
- Dhaese SE, Kreps EO, Consejo A. Scleral shape and its correlation with corneal parameters in keratoconus. Cont Lens Anterior Eye. 2021 Aug;44:101366.
- DeNaeyer G, Sanders D. Collagen Crosslinking for Keratoconus Can Change Scleral Shape: A Case Report. JCLRS. 2018 Mar;2:15-21.
- DeNaeyer GW, Sanders DR, Farajian TS. Corneal and scleral elevation topography changes after corneal hydrops in keratoconus cases. Poster presented at the Global Specialty Lens Symposium, Las Vegas. January 2019.



