SCLERAL LENSES HAVE a number of specialty applications that can both change people’s lives and create issues that need to be addressed. This article reviews three examples of various scleral lens uses and their success. This includes: 1) oblate scleral lenses for prolate corneas, 2) piggyback scleral lenses, and 3) factors contributing to scleral lens spontaneous on-eye breakage.
OBLATE SCLERAL LENSES FOR PROLATE CORNEAS
Scleral lenses (SLs) may have a prolate or an oblate design. The prolate design is characterized by a steeper back optic zone radius (BOZR), and the lens peripheral curves tend to flatten toward the periphery. In oblate SLs, also called reverse geometry lenses, the BOZR is flatter than the adjacent peripheral curve. Oblate designs are generally indicated in cases in which the cornea is flatter centrally compared to the periphery, such as corneas that have undergone refractive surgery for myopia, radial keratotomy, or certain keratoplasty procedures.
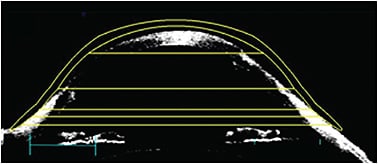
By fitting a prolate lens on an oblate cornea, the lens may have an optimal clearance centrally but touches the mid-peripheral cornea. To clear the peripheral cornea from touch, lens vault needs to be increased, resulting in excessive central clearance (Figures 1 and 2).
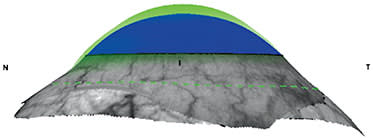
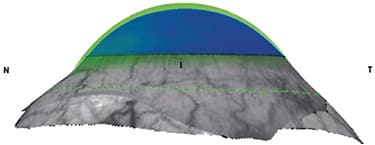
Excessive central clearance will affect oxygen supply to the cornea, lens centration, midday fogging, and quality of vision due to the prismatic effect from the post-tear layer, especially in cases with decentered ectasias. Oblate designs will allow for proper vault in the mid-peripheral cornea while maintaining the appropriate central clearance (Figure 3). However, oblate SLs may also be beneficial for prolate corneas.
Here are some indications for using an oblate lens design:
Peripheral Ectasia In the case of peripheral ectasia, the lens will touch the apex while exhibiting excessive clearance in the opposite quadrant (Figure 4). If using a prolate lens, the corneal vault needs to be increased to avoid the lens touching the corneal apex. Several significant issues will result from the augmented lens sagittal height:
The excessive vault in the opposite area will increase further, causing fitting issues, such as lens decentration, midday fogging, excessive limbal clearance, and discomfort.1
- The oxygen transmissibility to the cornea will significantly decrease. This is an important concern, especially in compromised corneas.2,3
- The BOZR will become steeper and the post-lens layer will become increasingly convex, adding more plus power to the lens system. To compensate for this plus power, the lens requires a higher minus power. With high-minus power, the optic zone diameter is reduced. If the lens is decentered and the pupil diameter is large, the transition between the optic zone and the peripheral curve will fall in the pupil area, increasing higher-order aberrations (HOAs). A low-minus-powered SL will reduce image minification, impacting the quality of vision.4
- Additionally, SLs show some decentration inferiorly and temporally. Due to the lens decentration, prismatic effect and HOAs, especially spherical aberration and coma, will significantly increase with lens power increase.
Reverse geometry lenses, in which the peripheral cornea area is steeper than the central, will allow adequate vaulting over the decentered ectasia while maintaining the central lens area close to the cornea. As a result, the oxygen delivery to the cornea is greater, the lens minus power is reduced, the optic zone diameter is larger, and the lens is more stable on the eye.
Limbal Clearance Small SLs are generally designed for eyes that have a smaller horizontal visible iris diameter (HVID). However, the choice of lens diameter depends on various factors, and sometimes a smaller lens is necessary despite the larger HVID. This can be due to factors such as a small palpebral aperture, difficulties in applying larger lenses, the need to avoid conjunctival irregularities, or a low corneal sagittal height.
Some lens designs offer the ability to adjust only the limbal clearance, ensuring that the lens does not touch the limbus. Alternatively, an oblate design, featuring a steeper curve over the limbus, can effectively address any contact in that area.
Lens Power in Advanced Keratoconus, Highly Irregular Corneas, or High Myopia When fitting SLs for patients who have advanced keratoconus, highly irregular corneas, or high myopia, a steep BOZR is necessary, resulting in a high-minus-powered lens. As mentioned earlier, a steep curve and high-minus lenses present several issues. With an oblate design, the BOZR will be flatter, reducing lens power (Figure 5). The following is an example of how a flatter BOZR may significantly reduce the lens power.
- Prolate lens parameters:
- BOZR = 7.20mm
- Back Vertex Power (BVP) = –9.00D
- Oblate lens parameters:
- BOZR = 8.90mm
- BVP = –0.50D
The quality of vision provided by a lens that has a power of –0.50D is greater than that of one that has a –9.00D power, considering image minification, lens decentration, prismatic effect, HOAs, and optic zone diameter. Additionally, the quality of vision for presbyopic patients, distance and near, is greater with an add of +2.00D on a –0.50D refractive error as opposed to a –9.00D refractive error.
Oblate designs, originally designed for oblate corneas, have several benefits in prolate corneas in terms of ameliorating the quality of vision, providing lens stability on the eye, and more corneal physiological outcomes. Oblate SLs have particular advantages in cases with decentered ectasias, advanced keratoconus, highly irregular corneas, high myopia, and larger corneas needing to be fitted with small-diameter SLs.
PIGGYBACK: AN ALTERNATIVE FOR SCLERAL LENSES
SLs are beneficial for several indications, and sometimes they represent the only option for conditions that cannot be fitted with other modalities. Fitting failure in these conditions may be dramatic and result in eye surgery, depression, psychological problems, or emotional instability. Clinicians need to be creative and think outside the box to avoid dropout and its psychological impact.
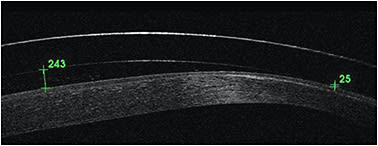
Piggybacking a SL onto a soft contact lens (SCL) may be necessary to ameliorate the fit or function. A concern of applying two contact lenses may be corneal edema. A recent study compared corneal edema in individuals wearing standard SLs and reverse piggyback SLs in 10 healthy participants with normal corneas.5 In the study, optical coherence tomography measured corneal and fluid reservoir thickness before and after wearing the lenses and found similar levels of central corneal edema between the two groups.
The following are some conditions that can benefit from this technology. To start, let’s look at a conventional piggyback system in which a SL is placed over a soft lens.
Insufficient Vault In some highly irregular corneas, SLs may not properly vault over a corneal elevation or apex while at the same time showing excessive clearance in the other corneal areas, generally the opposite area. An oblate design may be beneficial in the case of a decentered corneal apex.
If the corneal elevation is located centrally, it is necessary to increase lens sagittal height. However, this will further increase the peripheral clearance, which is already excessive, causing several issues such as lens decentration, midday fogging, excessive limbal clearance, discomfort, prolapse, and hypoxia.1,3
Applying an SCL under the SL will avoid corneal touch and mechanical stress over the epithelium.6 Additionally, when applying a SL in progressive keratoconus, the vault may appear optimal during the fitting process, but insufficient at the follow-up visits as the disease progresses. In these cases, a piggyback SL over an SCL may avoid SL remakes and additional costs to the patient. This may be an option until the annual scheduled lens replacement.
Photophobia Some patients who have severe ocular surface disease may have increased indoor light sensitivity, compromising their vision. While sunglasses are usually worn outside, their wear may be undesirable indoors. An SL may be piggybacked onto a tinted SCL to alleviate light hypersensitivity during daytime wear (Figure 6).

Initial Handling Issues and Discomfort with SLs SL handling may be challenging, and in some cases it may lead to abandoning SLs.7-9 In particular, SL handling difficulties have been reported in a pediatric patient of 6 years old.10 SLs were prescribed to this patient to restore vision after a traumatic injury to her left eye and to avoid amblyopia.
The patient reported significant discomfort and pain after five minutes of lens application, leading to its immediate removal. An SCL was prescribed for training and to increase her confidence in lens application and removal. The SL was refit when the patient became comfortable with SCL handling. She continued to report significant discomfort with the SL and had to remove it after a few minutes of wear. An SCL was prescribed under the SL to alleviate the pain during lens wear.
After two weeks of piggyback wear, the patient could wear the SL without the soft lens for eight to 10 hours daily.10 In this case, the piggyback system helped reduce initial discomfort and pain and increase SL tolerance in the eye.
Midday Fogging This is a common, frustrating issue when wearing SLs, which results in unsatisfactory vision and potential dropout.9 This problem is multifactorial. Piggybacking lenses may be an option to reduce midday fogging when it persists despite several management strategies. This approach reduces the volume of post-lens fluid, effectively minimizing fogging. Furthermore, the SCL may act as a barrier, preventing the ingress of particles and further decreasing the occurrence of this phenomenon.
Allergy to Rigid Contact Lenses While it is uncommon, patients may exhibit an allergic reaction to the material of rigid contact lenses. Allergies can also occur in response to the tint, UV blocker, or surface treatments applied to the lenses. Placing a soft lens beneath the SL can help minimize the contact between the rigid lens and the conjunctiva, thereby reducing the eye’s exposure to allergens.
Another option is to use a reverse piggyback system in which a soft lens is placed over the SL.
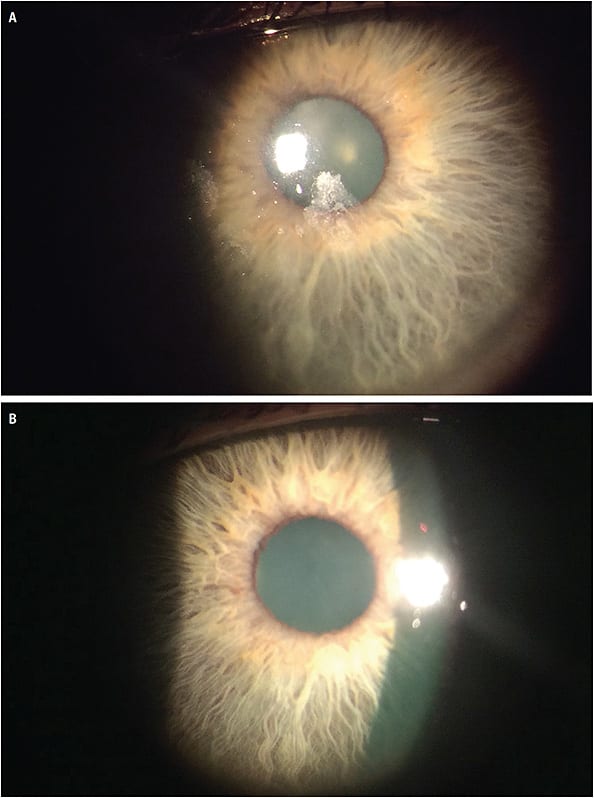
Occlusion Therapy A reverse piggyback SL was used on an 8-month-old pediatric patient.11 The patient was affected by familial dysautonomia, which is characterized by alacrimia and corneal hypoesthesia. As a result of her low corneal sensitivity, a scratch on her right cornea went unnoticed and developed into a severe corneal erosion, which progressed into a neurotrophic ulcer and a significant scar covering her iris.
SLs were prescribed for this baby to protect her corneas from future trauma and dryness. After two months of lens wear, the scar density reduced. Atropine was prescribed for the right eye to enlarge pupil diameter to exceed the diameter of the corneal scar and allow visual development.
After another two months, the haze regressed, and the iris was visible through the scar. It has been observed that she also has visual functionality in her right eye while her left eye is covered. Intermittent esotropia has begun to develop.
Occlusion therapy was prescribed to enhance vision in her right eye. Patching occlusion was unsuccessful as the baby did not cooperate. The only option was occlusion through use of a contact lens. As the good eye had to be occluded, SCLs on the baby’s cornea were strongly contraindicated because of the increased traumatic and ocular infection risks. It was decided to apply a reverse piggyback on her left eye with a soft lens placed over the SL.
The SCL was well centered and appeared not to dry quickly. A wearing time regimen of four hours was initiated, to be increased to seven hours per day, with the use of non-preserved artificial tears every two hours to maintain soft lens hydration.
After a few weeks, atropine use was discontinued, but left eye occlusion continued. At the final visit, corneal haze was reduced, there were no changes in vision, and the esotropia disappeared.11
Wettability Issues with lens surface wettability frequently occur, and this problem is triggered by storing the lenses dry. It becomes a challenge when performing the over-refraction, as vision is affected by the poor wetting areas of the lens surface.
To ameliorate wettability during over-refraction, it may be recommended to wipe the anterior surface of the SL while it is applied on the eye with a moistened cotton swab or an SL plunger. It also has been suggested to apply a low-powered daily contact lens over the SL. It’s possible that placement of an SCL over the SL may ameliorate wettability (Figure 7).
When fitting SLs, creativity is often needed to resolve fitting challenges and provide a good contact lens solution to patients, preventing dropout. Piggyback SLs may be considered an optimal option when all other solutions fail. However, it is essential to consider some challenges.
Two types of care solutions are needed, one for the SCLs and another for the SLs. Patients may be confused by the different solutions prescribed and compliance may reduce, triggering issues and complications to the eye.
The use of a hydrogen peroxide system may be beneficial, as this care system may be used for both lens modalities, soft and rigid lenses. A daily disposable SCL may be used, avoiding the need for two different solutions. Patients will use their usual solution for SLs, as a disposable lens does not need to be cleaned and disinfected. Additionally, a daily disposable soft lens will minimize allergen buildup and deposits.5
Another important concern when fitting a piggyback is hypoxia. The use of high Dk for SL and silicone hydrogel is indicated.
FACTORS CONTRIBUTING TO SCLERAL LENS SPONTANEOUS ON-EYE BREAKAGE
SL handling has been reported to be a challenge for patients and sometimes may lead to dropout.7,8 When handling the lens, patients may damage or break it. While a relatively high incidence of lens breakage during its handling was reported in the keratoconus12 and pediatric13 populations, only two single cases of on-eye breakage were described in the literature.14,15
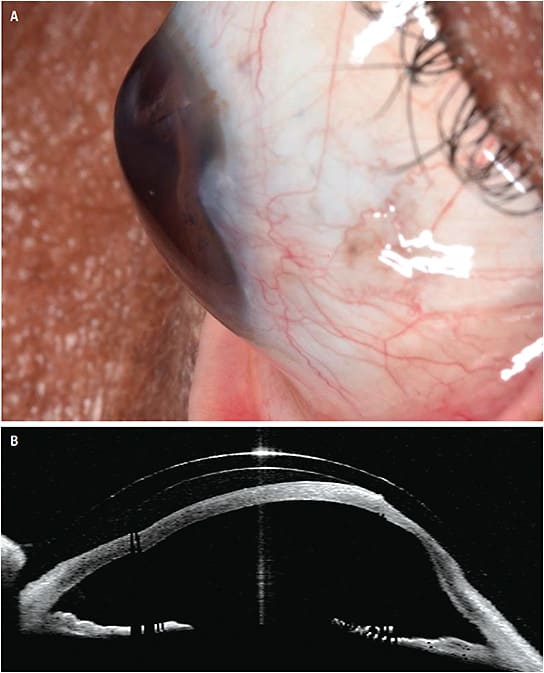
Walker and colleagues reported an on-eye breakage of an SL following a significant impact. A staple sprang from an electric stapler and hit the patient’s left eye, creating a hole in the center of the lens14 (Figure 8). The patient reported moderate pain and conjunctival redness. The authors concluded that the rigidity of the SL and the deep post-lens fluid reservoir provided a strong protective barrier to the cornea and anterior segment, preventing significant damage.
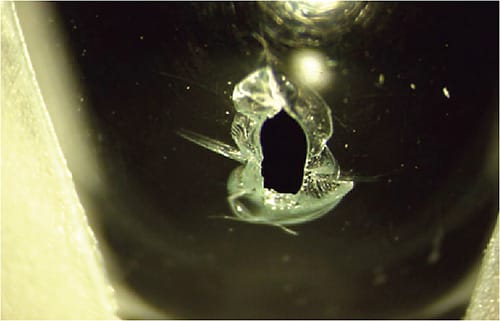
Recently, Macedo and coworkers reported a similar episode of lens rupture in the eye from an object moving at high velocity, without triggering any severe corneal damage.15 The authors had the same conclusions as those of the previous report: the rigid lens combined with the large fluid reservoir protected the eye, allowing it to absorb and distribute the kinetic energy of the object impacting the lens.
Clinically, sporadic episodes of a lens breaking in the eye have been reported. It is not common for contact lenses to spontaneously break while on the eye. Damage to or fracture of the lens is generally triggered by touch or blinking, causing the final break. In personal experience, patients and practitioners reported episodes of SL on-eye rupture following a significant trauma. Also in these cases, the SL absorbed the trauma and saved the cornea from more damage. Several factors might cause SL spontaneous on-eye breakage, including the following.
SL Handling Like all rigid lenses, SLs are subject to physical damage and chipping. SLs are more exposed to these issues because of their larger diameter and deeper sagittal height, which result in difficulties when handling during the cleaning process, lens application or removal, or lens placement in the lens case. In some patients, handling difficulties is greater.
- Patients Who Have Difficulties Handling becomes a greater challenge in patients who have dexterity issues, tremors, arthritic joints, or missing digits. Patient education is crucial in these cases. It’s also essential to choose the appropriate method for lens handling and tools for lens application and removal, increasing success and avoiding any damage to the lens.
- Patients Who Have Poor Vision The risk of having the lens damaged or chipped is also greater in patients who have poor vision with high ametropia, presbyopia, highly irregular cornea, or advanced keratoconus, as they have more difficulty seeing the lens when handling. Additionally, because of their poor vision, those patients cannot appropriately check the lens integrity before applying it to the eye. All SL wearers must check the lenses carefully before application; this becomes more important in patients who have poor vision.
Storage Case Issues SLs may be especially subject to damage because of their larger diameter; many cases were originally designed for the smaller corneal and soft lenses. The risk of lens damage from the storage case is higher for patients who have handling issues and poor vision, because these wearers may have difficulty in correctly placing the lenses inside the compartments. If the lens edge is positioned slightly outside the compartment, it will chip during case closure.
The SLs should be placed in the concave side of the case and not on the convex one. Maintaining the lenses horizontal and level, the vertical part of the case should be brought toward the lens and gently closed (Figure 9).
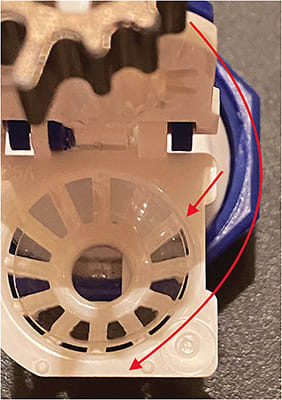
Along with these considerations, patients who have poor vision require more dedication and time during education sessions. They must wear their glasses to carefully inspect both lenses before their application every morning and verify the correct lens placement in the case compartments before closing the case. It is appropriate to provide larger cases dedicated to SLs, which are designed to accommodate the lenses’ larger diameter and greater sagittal height (Figure 10). The lens will fit more securely in larger cases, avoiding any chipping during closure.

Thin Lenses The large diameter of an SL makes it more susceptible to damage and breakage. The thinner the SL, the higher the risk of rupture. The lens thickness also depends on lens power. The higher the negative power, the thinner the lens.
It’s crucial to select the appropriate material for large and high negative SLs. A material with higher modulus, superior resistance to flexure, and greater hardness is more stable and resistant to breakage. Also, it is possible to change the thickness of negative power lenses. Without impacting lens power, the lens may be made thicker. This might be beneficial to increase lens resistance to fractures, especially for wearers who have handling issues and poor vision.
Oblate designs are indicated in high negative lens powers. By flattening the lens base curve, the negative lens power will reduce and the lens will be thicker. Additionally, oblate designs increase the quality of vision in high myopes and patients who have advanced keratoconus.
SUMMARY
SL design and manufacture continues to improve and expand to meet the ever-increasing and potentially life-changing benefits of this modality. The examples given in this article will hopefully both expand and optimize your scleral lens practice. CLS
References
- Fadel D. Scleral Lens Issues and Complications Related to a Non-optimal Fitting Relationship Between the Lens and Ocular Surface. Eye Contact Lens. 2019 May;45:152-163.
- Fadel D. Modern scleral lenses: Mini versus large. Cont Lens Anterior Eye. 2017 Aug;40:200-207.
- Barnett M, Courey C, Fadel D, et al. CLEAR - Scleral lenses. Cont Lens Anterior Eye. 2021 Apr;44:270-288.
- Vincent SJ, Fadel D. Optical considerations for scleral contact lenses: A review. Cont Lens Anterior Eye. 2019 Dec;42:598-613.
- Bliss VH, Branjerdporn N, Ooi PJ, et al. Corneal oedema during reverse piggyback scleral lens wear. Ophthalmic Physiol Opt. 2023 May 11. [Online ahead of print]
- DeNaeyer G. Piggybacking Scleral Lenses. Contact Lens Spectrum. 2012 Feb;27:18.
- Barnett M, Lien V, Li JY, et al. Use of Scleral Lenses and Miniscleral Lenses After Penetrating Keratoplasty. Eye Contact Lens. 2016 May;42:185-189.
- Asena L, Altinors D. Clinical outcomes of scleral Misa lenses for visual rehabilitation in patients with pellucid marginal degeneration. Contact Lens Anterior Eye. 2016 Dec;39:420-424.
- Pecego M, Barnett M, Mannis MJ, Durbin-Johnson B. Jupiter scleral lenses: the UC Davis Eye Center Experience. Eye Contact Lens. 2012 May;38:179-182.
- Murphy DA, Samples JS, Zepeda EM, Riaz KM. Progression From Soft Lens to Piggyback Soft-Scleral Contact Lens System to Facilitate Scleral Lens Use in a Pediatric Patient. Eye Contact Lens. 2021 Jul 1;47:426-428.
- Michaud L, Carrasquillo K. Piggyback cosmetic contact lens as an occlusion therapy in a patient with familial dysautonomia. Eye Contact Lens. 2010 Nov;36:367-370.
- Fuller DG, Wang Y. Safety and Efficacy of Scleral Lenses for Keratoconus. Optom Vis Sci. 2020 Sep;97:741-748.
- Rathi VM, Mandathara PS, Vaddavalli PK, Srikanth D, Sangwan VS. Fluid filled scleral contact lens in pediatric patients: challenges and outcome. Cont Lens Anterior Eye. 2012 Aug;35:189-192.
- Walker MK, Caroline P, Kinoshita B, Lampa M, Zheng F, André M, Kojima R. The Protective Advantage of Scleral Contact Lenses. Poster presented at the Global Symposium of Lens Specialty, Las Vegas, January 2015.
- Macedo-de-Araújo RJ, van der Worp E, González-Méijome JM. On-eye breakage and recovery of mini-scleral contact lens without compromise for the ocular surface. Cont Lens Anterior Eye. 2018 Jun;41:311-314.




