ASTIGMATISM AND GP lenses are a match made in heaven. They go together like peanut butter and jelly, bacon and eggs. Given the surge in interest in fitting GP lenses, driven largely by myopia control and orthokeratology, it’s a great time to revisit some of the basics that make fitting GPs to your astigmatic patients simple and successful.
A key reason that GPs are such a great option for patients who have moderate to high astigmatism is the clarity and stability of vision. Most of the time, particularly in cases of with-the-rule (WTR) astigmatism, a non-flexing spherical lens will correct virtually the entire astigmatic refractive error without worry about lens rotation—that’s the beauty of spherical fits.
Now think about a soft toric. Although we have many exceptional designs available today, they are subject to instability with active head and eye movements. Several studies have documented mislocation/rotation of as much as 25º to 30º with changes in head and gaze position.1-3 And that can lead to visual instability, often in situations like sports where your patients are counting on clear vision.
Keep in mind that every 10º of toric lens axis mislocation induces astigmatism equal to approximately one-third of the toric lens power; and for every additional 10º of rotation, there is a doubling of the amount of induced cylinder4 (Table 1).
| SOFT LENS CYLINDER POWER | ||||
| 0.75DC | 1.25DC | 1.75DC | 2.25DC | |
| 5º off axis | 0.12 | 0.20 | 0.29 | 0.38 |
| 10º off axis | 0.25 | 0.41 | 0.58 | 0.75 |
| 15º off axis | 0.37 | 0.61 | 0.87 | 1.13 |
| 20º off axis | 0.50 | 0.82 | 1.16 | 1.50 |
Beyond the optical benefits, GPs are super easy to fit. Trial lenses are nice, but not needed—just a good spectacle refraction (Rx) and keratometry readings (Ks). But first, let’s talk about a few other tips for GP fitting success.
PATIENT COMMUNICATION
These days, patients may have never met anyone wearing GP lenses. But in the “old days,” some people had a very negative impression of how a GP lens would feel on the eye—based primarily on misinformation. That said, there is a sensation associated with first-time wear of a GP lens, but use of topical anesthetic at fitting and dispensing visits has been shown to markedly improve the adaptation experience.5
In an 80-subject clinical trial comparing the use of anesthetic versus a placebo drop, the anesthetic group rated comfort significantly higher at both dispensing and two-week visits. The subjects also perceived adaptation, sensitivity, and time to adapt to be significantly better at the end of the one-month study, and the dropout rate was 2 out of 40 (5.0%) compared to 8 of 40 (20.0%) in the placebo group.
The second tip is to be positive in communication to the patient and share the reasons for selecting a GP lens. A presentation to the patient should include the benefits of crisp and stable vision, excellent oxygen transmission, durability, and ease of care. They should also be assured that the lens awareness or “tickling” sensation that they experience when lenses are first applied is a result of the lids blinking across the lens edge; reassure them that this will go away as their eyes adapt to the lenses, usually within the first few days or, occasionally, weeks of wear.
And do it with a positive tone and affect. A study compared three types of presentation of features and benefits of GP lenses: Fear-arousing words and a non-enthused tone, neutral content/non-enthused, and neutral content delivered with an enthused affect.6 There was a significant difference in the number of dropouts over the month-long study: 6/19 (31.6%) who received the fear-arousing message delivered without enthusiasm, 2/17 (11.8%) who received neutral content in a non-enthusiastic presentation, and 0/13 (0.0%) when the neutral content was delivered with enthusiasm.
And finally, there is no physiological basis for the need to “build up” lens tolerance starting at a few hours of wear. It’s very disruptive for people to remove lenses in the middle of the day. It’s better to have them wear lenses as long as is comfortable from the beginning; but be sure to let them know they should remove the lenses if they feel their lids becoming sore or if the sensations are worsening. If there is a potential concern about being able to wear them all day, have patients start on a weekend or day when they don’t have activities scheduled that might be interrupted by removing the lenses.
PATIENT SELECTION
Patients who have WTR refractive astigmatism between 1D and 2D whose refractive cylinder referenced to the corneal plane and difference between keratometry readings (ΔK) are similar (within ~0.75D) are great candidates for a spherical GP fit. These patients have sufficient astigmatism to be bothersome visually but are likely to have levels of corneal astigmatism that make fitting a GP simple.
The WTR cornea provides a nice geometry that allows the spherical lens to gently tilt back and stay under the upper lid without creating excessive edge lift inferiorly. Further, the tear film behind the GP lens neutralizes the astigmatism. Remember that because the natural intraocular lens usually has about 0.50DC to 0.75DC against-the-rule (ATR) power, expect the cornea to have slightly more physical astigmatism than in the cylindrical component of the refraction.
When corneal astigmatism exceeds about 2.50D WTR, it is time to start thinking of a bitoric option—that’s when that inferior clearance can become excessive, and flexure may interfere with the ability to mask the corneal astigmatism. Usually, this will be a spherical power effect bitoric that has the optics of a sphere (more about this later). ATR astigmatism can be tricky, but not impossible with GP lenses. Because low ATR refractive astigmatism often comes from the lens and not the cornea, you do lose the benefit of the GP lens on the surface to mask astigmatism, however. With higher amounts of ATR cylinder, the steeper horizontal meridian of the cornea can make it difficult to center a GP lens. Those ATR patients are often better suited to soft toric options.
LENS DESIGN PROCESS
It isn’t essential to have a trial or diagnostic set when fitting a GP lens. The warranted or guaranteed fit policies of many GP laboratories make empirical fitting almost risk-free. And when you have a lens custom designed for the patient, they will have crisp vision and can begin their GP journey fully equipped for success. As mentioned earlier, Ks and a refraction are really all it takes to design the lens. Laboratories will likely have basic designs optimized in terms of material, peripheral curves, thickness, etc., so you just need to decide on a base curve (BC), power, and diameter.
Let’s start with a spherical example. For most eyes, a diameter in the 9.0mm to 9.5mm range will provide for a fit that can tuck under the upper lid and be centered by the dynamics of the lens-cornea interaction. This is effectively an “interpalpebral” or corneal fit, even though the upper lid will generally interact with the lens. A true “lid-attached” fit relies on the lid to hold and move the lens, but may lead to unintended corneal molding due to the need to fit the lens flatter than the steeper corneal meridian.
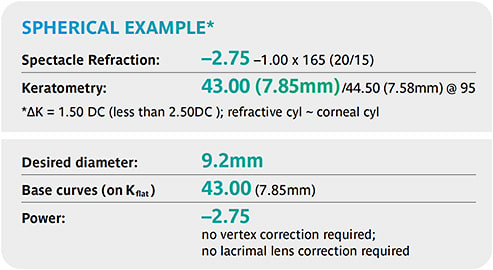
The “on flat K” fit makes calculating power easy (no lacrimal lens created) and will usually provide a lens-to-cornea fitting relationship that results in good vision, comfort, and physiology. Just find the flattest corneal meridian (lowest dioptric power, longest radius) and that becomes the initial base curve (in diopters). Note that while a base curve is a radius and, therefore, expressed in millimeters, using diopters is well understood and makes calculations easier. The spherical power will be the vertex distance-corrected spherical component of the spectacle refraction: a lower number for minus values greater than –4.00D, and a higher number for plus values greater than +4.00D.
Conversion charts are available from your laboratories, in lens parameter guides, and online; again, it’s easy to just ask your online assistant to pull up a vertex distance chart. You generally only need to vertex distance correct the spherical component of your spectacle Rx when fitting a spherical lens; the GP lens will take care of the rest.
An exception is when the sphere power and cylinder power added together exceed –4.00D. We’ll talk more about this in the toric design section below. See the example in Figure 1 for a simple WTR astigmatic patient who has low myopia. Practitioners need only concern themselves with the numbers in blue.
Simple, right? You may choose to fit a little steeper than K, just go back to the SAMFAP rule (steeper add minus, flatter add plus) to adjust your final lens power. For example, to go 0.50D steeper, such as when fitting for overnight wear, order a lens with an additional –0.50D power to compensate for the lacrimal lens. And yes, overnight wear is possible with GPs, even when you aren’t doing orthokeratology. One lens material is cleared for up to 30 days of overnight wear, and had a statistically significant lower rate of adverse events compared to a soft lens worn overnight on a six-night-per-week basis.7 Overnight lens adherence is significantly more frequent and persistent for flat-fitting lenses as compared to steep.
Now, back to fitting astigmatic patients. When corneal astigmatism exceeds about 2.50D, a toric back surface is recommended to more evenly distribute lens bearing to avoid unwanted corneal changes and to improve lens wearing comfort. And more often than not, these high levels of astigmatism are due primarily to corneal astigmatism. Therefore, optically there is a need for a spherical GP correction even though physically a toric is needed. Luckily, there is a solution that is as easy to design as a spherical lens and provides the same optical benefit—that is, freedom from any optical effect of lens rotation. So, let’s get started. The principles are the same—the desire to fit a cornea that has about 0.75D to 1.00D of WTR astigmatism—as with a lens that is spherical in nature.
This design is referred to as a spherical power effect (SPE) bitoric. A certain amount of cylinder is added to the front surface to offset the effect of creating the toric back surface, and laboratories will determine that. Determine the back surface curves and the spherical power you’d like based on the same principles used for the spherical lens. We’ll assume that we want an on-K fit again, so our flat curve will be the same as our flattest corneal meridian. We’ll create sufficient toricity on the lens to leave the ideal amount of uncorrected corneal astigmatism or “rocking room” between the lens back surface and the cornea.
The only slightly tricky thing to remember with higher amounts of cylinder is to correctly vertex the total power of each meridian in order to determine the cylinder at the corneal place when looking at how close corneal and refractive cylinders are (Figure 2). With minus sphere powers and high cylinder powers, the refractive cylinder is less at the corneal plane.
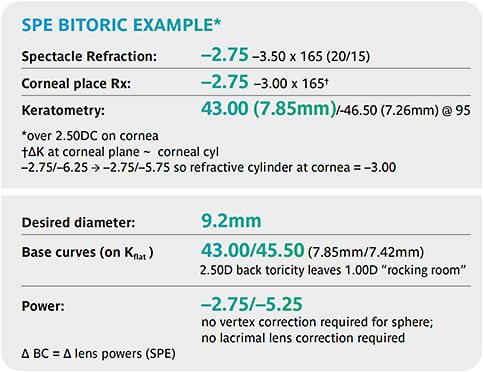
What is easy about an SPE design is that once you’ve determined the difference between your two back curves (allowing for your “rocking room”), you’ve also determined the difference between the powers of your two meridians. If the back surface has 2.50D difference as in the example in Figure 2, your second power will be 2.50D more minus than your first one (determined the same way you did with spheres). With an on-K fit, it can almost be done in your head.
Without a diagnostic fitting set, which is rare in a typical practice, the recommendation is to order an SPE lens, even if you do see a mismatch between refractive and corneal cylinder. If they don’t routinely do it, have the lab dot the flat meridian of your SPE bitoric. In the unusual case that vision isn’t as good as you expect, note the position of the axis of the lens on the eye and add or remove cylinder at that axis.
With high amounts of corneal cylinder, the axis of the corneal cylinder will usually be similar to the refractive axis. If additional cylinder is needed, the lens now becomes a cylindrical power effect (CPE) bitoric; however, by starting with a SPE, there are fewer issues with cross cylinder calculations when troubleshooting the next lens.
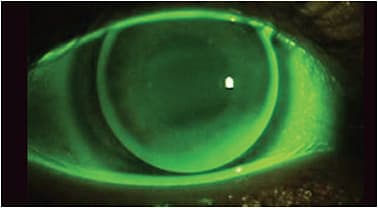
FLUORESCEIN PATTERNS
The last factor to mention is fluorescein patterns. Learn to read them. With corneal astigmatism, the fluorescein pattern will show what to do when making changes. One mistake to avoid is flooding the eye with fluorescein. All that will be seen is the front surface tear film. Apply the minimum amount of fluid by wetting the strip and then shaking it until no drops remain, and then gently touch (don’t “paint”) a peripheral area of the conjunctiva. Have the patient blink a few times and then view the pattern. Sometimes looking outside of the slit lamp at the unmagnified view makes it easier to see the overall pattern.
Using the cobalt blue filter, open the illumination up as wide as possible and hold a yellow barrier filter in front of the instrument optics (not in front of the illumination). An alignment pattern on a low-to-moderate WTR cornea will appear uniformly dark across the horizontal midline, with a bright green area of fluorescence across the bottom of the lens (if it is tucked under the upper lid) as shown in Figure 3. With an SPE lens leaving 0.75D to 1.00D of “rocking” room, the pattern will look similar.
With a spherical lens on a highly astigmatic cornea, bubbles can often be seen at the inferior edge, particularly on the blink, suggesting that you need to “wrap” (steepen) that vertical meridian a little closer to the cornea. If you’ve gone too steep in the horizontal meridian, you will see a classic “double D” pattern, as shown in Figure 4.
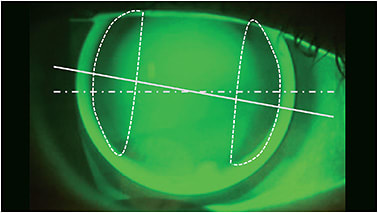
The fluorescein pattern will also show you the axis of the corneal astigmatism. With too much toricity in a bitoric lens, a black ring of midperipheral bearing will be observed all the way around the lens, indicating the need to flatten the steeper meridian to allow better tilt and tear exchange. One paper noted a quick and consistent way to record key aspects of a GP fit, which may be helpful.8
IN CONCLUSION
Fitting GP lenses really is simple and can even be performed empirically with high success. In a clinical study comparing lenses ordered empirically versus via trial fitting, 86% of subjects were successfully fit from the nomogram (empirical) versus 92% with trial fitting, effectively not different.9
So, the next time you have a patient in the chair who has moderate or high astigmatism, talk to them about the benefits of GP lenses, and work with your local GP laboratory to get a custom-designed and -manufactured GP sphere or SPE bitoric for them to try. You may be surprised at your success. CLS
References
- Zikos GA, Kang SS, Ciuffreda KJ, et al. Rotational stability of toric soft contact lenses during natural viewing conditions. Optom Vis Sci. 2007 Nov;84:1039-1045.
- Chamberlain P, Morgan PB, Moody KJ, Maldonado-Codina C. Fluctuation in visual acuity during soft toric contact lens wear. Optom Vis Sci. 2011 Apr;88:E534-E538.
- McIlraith R, Young G, Hunt C. Toric lens orientation and visual acuity in non-standard conditions. Cont Lens Anterior Eye. 2010 Feb;33:23-26.
- Lindsay RG. A New Angle on Soft Toric Lenses. Contact Lens Spectrum. 2017 Aug;32:20-25.
- Bennett ES, Smythe J, Henry VA, et al. Effect of topical anesthetic use on initial patient satisfaction and overall success with rigid gas permeable contact lenses. Optom Vis Sci. 1998 Nov;75:800-805.
- Bennett ES, Stulc S, Bassi CJ, et al. Effect of patient personality profile and verbal presentation on successful rigid contact lens adaptation, satisfaction and compliance. Optom Vis Sci. 1998 Jul;75:500-505.
- Gleason W, Tanaka H, Albright RA, Cavanagh HD. A 1-Year Prospective Clinical Trial of Menicon Z (tisilfocon A) Rigid Gas-Permeable Contact Lenses Worn on a 30-day Continuous Wear Schedule. Eye Contact Lens. 2003 Jan;29:2.
- Wolffsohn JS, van der Worp E, de Brabander J. Consensus on recording of gas permeable contact lens fit. Cont Lens Anterior Eye. 2013 Dec;36:299-303.
- Postma JT, Postma AM, Schnider CM. A comparison between nomogram vs. trial fitting of rigid gas permeable contact lenses. J Am Optom Assoc. 1993 Apr;64:258-263.





