
KERATOCONUS IS TYPICALLY referred to as a bilateral corneal ectatic, thinning, and steepening disease.1,2 Corneal scarring is a common consequence of the pathophysiological events of this pathology and should be added to that list.

Keratoconus is not a rare anomaly and until recently prevalence was believed to be 1 in 2,000.3 However, recently a much higher incidence has been reported, suggesting that keratoconus has an incidence of 1 in 375 in a general population.4 Due to the suggested greater incidence, it may be argued that this disease, together with other ectatic disease entities, such as pellucid marginal degeneration and post-refractive ectasia, deserve more of our attention.
Cross-linking of the progressively keratoconic cornea in accordance with the U.S. Food and Drug Administration (FDA)-approved Dresden protocol is a well-established and effective procedure.5 However, there are a few remaining issues that require further studies.
Can the cornea of the young safely be exposed to an adult dose, 5.4 J/cm2, of UVA of 365nm? Is the immature cornea more likely to develop scar formation? Will one UVA exposure stop progression? Should the cornea of the young keratoconus patient be treated immediately on diagnosis or will progression have to be established first? This review attempts to assess where we are in addressing these issues.
DRESDEN PROTOCOL
The FDA has limited the age range for the Dresden protocol to 14–65 years, which was the age range of the cohort studied in the clinical trial that led to the approval (Table 1). Incidentally, the FDA-approved protocol does not exactly follow the original Dresden protocol, but the small differences are not likely to affect clinical outcomes.5
| Patient age range | 14-65 years |
| Corneal thickness | ≥ 400μm |
| Wavelength | 370nm |
| Irradiation (energy x time = dose) | 3 mW/cm2 x 30 minutes = 5.4 Joules |
| Epitheliμm | debrided (epi-off) |
| Two similar formulations with a difference in osmolarity Riboflavin (Vitamin B2) |
Isotonic Photrexa Viscous - 301-339 mOsm/kg riboflavin 5’-phosphate in 20% dextran ophthalmic solution 0.146%; both solutions can be applied every two minutes for 30 minutes. Photrexa – 157-177 mOsm/kg riboflavin 5’-phosphate dextran ophthalmic solution 0.146% Both solutions applied every two minutes for 30 minutes. |
Any deviation from the FDA protocol makes the procedure an off-label one—in other words, an experimental one lacking an evidence basis. This is not necessarily a bad thing and often practiced in medicine. Therapeutic medications are frequently dispensed off-label to good effect, but we need to fully understand what we are getting into when we do off-label cross-linking.
For example, in “accelerated” cross-linking, the purpose is to reduce the exposure time from the 30 minutes mandated by the Dresden protocol to a shorter and more manageable period. To deliver the required dose in a shorter time period, the beam energy must be elevated; if the exposure time is shortened to five minutes, the beam energy must be elevated six times.6 Is there any evidence showing that this higher beam energy is safe and effective?
The Dresden protocol dictates the removal of the epithelium (epi-off), typically by mechanical means or using an alcohol-soaked pad. Leaving the epithelium on (epi-on) and untouched throughout the irradiation is a common deviation from the FDA protocol.
PEDIATRIC CORNEA
One of the criteria that must be met to qualify for cross-linking irradiation is that the cornea must be at least 400µm thick. This limitation is there because the endothelium and the crystalline lens are harmed by 370nm wavelength and, if the cornea is thinner than 400µm, more of the radiation will reach these tissues. For this reason, we need to be aware of when a human cornea has reached adult size.
All corneal layers are formed and differentiated at birth and, interestingly, the corneal thickness of the newborn is between 545µm and 573µm, which is a little thicker than the size of the average adult corneal size, which is 535µm.7-12 Newborns’ corneas already have the negative meniscus lens profile seen in adults, where the peripheral cornea is approximately 80µm or 20% thicker than the central cornea.7,10
The larger horizontal corneal diameter in a newborn is 10.0mm, which is only 1.7mm less than the adult size.13 More recently the corneal diameter of 100 full-term newborns measured 9.5mm, but the orientation measurement was not disclosed.11 Nevertheless, we can conclude that the corneal diameter in the newborn is a little smaller than that of in adult.
So, at birth, the cornea is remarkably close to adult size and about 20µm thicker than the average adult cornea. However, according to Duke-Elder and Wybar, adult corneal dimensions are achieved within two years of life.13 Given that keratoconus is rarely diagnosed before the age of 10, there is no reason to delay cross-linking for fear that the cornea is still growing.14
INDICATION FOR CROSS-LINKING
Cross-linking of the corneal stroma is designed to arrest the progression of keratoconus. Unfortunately, the literature does not contain a validated protocol for determining progression of keratoconus. It is beyond the scope of this article to discuss all factors that play into diagnosing progression. Suffice it to say that many practitioners look for increased steepening of the corneal anterior and, particularly, posterior curvatures. However, we cannot ignore the fact that keratoconus is a corneal thinning disease and, therefore, the final formula for disease progression determination involves multiple factors.
In adolescents (age ≤ 18 years) disease progression is less associated with eye rubbing, ethnicity, and gender than with the severity of the disease.15 This suggests that the aggressiveness of keratoconus pathophysiology is a more important factor than the age at which keratoconus begins.
According to another study on a similar population, it was reported that patients with paracentral cones and/or corneal thickness less than 450µm had an increased likelihood of progression.16 The importance of the eccentricity of the cone apex is further indicated in a study involving 54 eyes of 36 pediatric patients, which concluded that the more peripheral the cone location is, the more likely there is progression.17 Studies clearly suggest that age is not the dominant factor in predicting progression.
POST-CROSS-LINKING PROGRESSION OF KERATOCONUS
Are children and adolescents at greater risk of post-cross-linking disease progression? There are now a healthy number of studies reporting on cross-linking in young people, and they are almost all from outside the U.S. Unfortunately, but not surprisingly, they report a diversity in outcomes. For reasons discussed above, we will limit our coverage to studies following the Dresden protocol.
The purpose of corneal cross-linking is to arrest disease progression, but UVA exposure is not always successful in achieving this result. Seiler and Seiler recently summarized the worldwide Dresden protocol cross-linking experience from “hundreds of thousands of keratoconus and post-LASIK ectasia eyes” as successful in arresting disease progression in more than 90% of exposures, with a less than 3% complication rate.18
Independent studies on adults utilizing the Dresden protocol report varying outcomes, some of which may be explained by the follow-up time, others by the protocol followed. One study of 241 keratoconic eyes of patients older than 18, which included a follow-up period of a maximum of six years, determined that only two eyes, or <1% of the eyes, progressed to need a retreatment.19
A more recent study assessing one eye of each of 131 keratoconic patients older than 18 showed that the steepest corneal meridian (Kmax) had increased by more than two diopters in five years in 15% of the eyes, but by 10 years this number increased to 33%.20 In this study, the spectacle best-corrected visual acuity in logMAR improved by one line and corneal thickness pre- and post-exposure were not statistically different. Only four eyes required a repeat procedure and were subsequently stabilized.
This tells us that cross-linking in adult eyes is successful in the majority of cases. A complete arrest of the progression of keratoconus is not guaranteed; the treated patient should be counseled on this reality prior to irradiation and followed for a long time.
Off-label trans-epithelial cross-linking, i.e., without performing epithelial debridement, can elevate the need for a second treatment to one-third of the irradiated patients.17 According to Seiler and Seiler, the reduced efficacy of the accelerated cross-linking (shorter exposure time with a higher energy beam) leads to a shallower corneal exposure with a resultant reduced tissue stiffening;18 Polido, dos Xavier Santos Araújo, Alexander, and colleagues, summarizing current data on the pediatric group, stated that we need long-term prospective clinical studies to determine the ideal protocol, progression assessment, and retreatment approach.21
Relatively early on, it was reported that in a group of 15 patients aged 10-15 and followed for 12 months, cross-linking appeared to be as effective on children as on adults.22 A later five-year study of patients who were under 18 years of age at the time of the cross-linking reported progression in 22% of the study cohort. This compares favorably to the aforementioned adult data.17 Extending the follow-up to 10 years did not alter the progression rate of pediatric patients measurably; Mazzotta and colleagues showed that 24% demonstrated progression after this period.23
CROSS-LINKING COMPLICATIONS
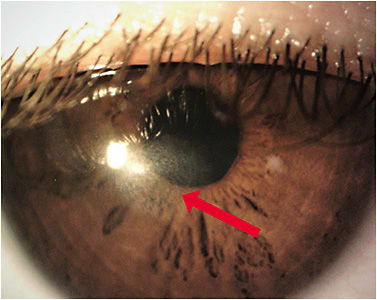
Corneal cross-linking utilizing the FDA-approved Dresden protocol, and off-label modifications thereof, does not come without risks (Table 2). Most commonly reported ocular complications following cross-linking are pain, stromal haze (Figure 1), and sterile infiltrates.24
| Most commonly reported complications24 |
|
| Rarer complications24 |
|
| Correlation25 | younger age = significantly correlated to experiencing greater pain |
In a prospective study of 178 eyes of 135 patients evaluating post-cross-linking, pain was most intense and usage of analgesics was highest within the first three days, decreasing significantly thereafter. Patient age and pain were significantly correlated, with younger patients experiencing greater pain.25 When considering cross-linking in pediatric patients, it is important to educate parents on the potential for pain and the use of analgesics for their child. Rarer but more detrimental adverse events include infection, corneal melting, stromal scarring, corneal perforation, and ulceration.
A prospective cohort study of 670 eyes reported a 1.6% post-cross-linking infection rate.24 Although this rate is low, there is a possibility that patients will develop reduced visual acuity; according to the data submitted to the FDA, 1% to 2% of patients had corneal opacity or scarring at the 12-month follow-up.26
TIMING OF CROSS-LINKING IN THE YOUNG
Because young patients’ corneas reach adult dimensions early in life, cross-linking should not be delayed due to young age. But should we advise the young keratoconus individual to have cross-linking performed on diagnosis, and not wait to establish progression? This is a notion already expressed in the literature, but is there a scientific basis for abandoning the steps mandated in the Dresden protocol?
Chatzis and Hafezi recommended that with children and adolescents, cross-linking should be performed as soon as the diagnosis of keratoconus is established and should not be delayed until progression is proven.27 In contrast, Or and colleagues argued that there is no urgency for immediate cross-linking without first establishing progression.28 This obvious contradiction requires future prospective, controlled studies with long follow-up periods to resolve this important issue.
We feel that the early age at which the cornea achieves adult dimensions explains why the young eye response is similar to an adult one. Studies have indicated that the location of the cone apex is a more important factor than age in predicting progression. In our university eye clinic, we favor looking for evidence of advancement of the disease before performing cross-linking. However, future research may convince us to do the opposite. This is, indeed, the essence of the need for continued study of literature.
WHAT HAVE WE LEARNED?
Based on existing literature, we have learned that by the time an eye has developed any clinically notable signs of keratoconus, it has already achieved adult dimensions.13 Therefore, cross-linking should not be delayed because of young age. The literature also provides evidence suggesting that the age of the patient is less of a factor in predicting progression than the eccentricity of the cone apex and the corneal thickness.
The weaker association of age with progression is further emphasized by a report on progressive keratoconus in patients over 48 years of age.29 We would argue that it would be prudent to establish progression rather than irradiate the young cornea immediately upon diagnosis.
A number of studies cited in the above text clearly indicate that best clinical outcomes are achieved by the Dresden protocol, which includes corneal epithelial debridement (epi-off).18,19 Trans-epithelial exposures are less effective and more frequently require retreatment.
Knowing that the ocular surface epithelium is extremely vulnerable to ultraviolet radiation, the standard cross-linking dose of 5.4 Joules/cm2 of 370nm wavelength is sufficient to induce severe metabolical stress and ultimately kill the epithelial cells forming the ocular surface.30-32 As a consequence, epithelial cells exposed to riboflavin will suffer terminal harm and be lost if irradiated with this dosage. Thus, trans-epithelial cross-linking is not likely to spare the epithelium or to prove that these cells can survive, say, in the presence of higher oxygen concentration, as has been tried. Healthy epithelial cells need to be illustrated in high resolution six to 12 hours after exposure or the time it takes for mortally traumatized epithelial cells to fall off the ocular surface.
There is a good argument for not utilizing the accelerated cross-linking protocols, in which radiation energy levels are elevated to reach the desired dosage in a shorter period of time. The safety of the vulnerable corneal cells, epithelium, keratocytes, and endothelium to this increased UV irradiation needs to be proven at a cellular level.

The cross-linking procedure represents a great advancement in the care of patients diagnosed with keratoconus (Figure 2). It is important to keep in mind that the goal for our young keratoconus patients is to avoid the need for a transplant. When a penetrating transplant is necessary, the risk of rejection may be higher in the younger individual. However, the literature and individual transplant surgeons are divided on the issue of whether age is a significant risk factor: some believe age is a factor33-36 while others argue37,38 that this is not the case. CLS
References
- Gomes JA, Tan D, Rapuano CJ, et al. Global consensus on keratoconus and ectatic diseases. Cornea. 2015;34:359-369.
- Santodomingo-Rubido J, Carracedo G, Suzaki A, et al. Keratoconus: An updated review. Cont Lens Anterior Eye. 2022;45:101559.
- Rabinowitz YS. Keratoconus. Surv Ophthalmol. 1998;42:297-319.
- Godefrooij DA, de Wit GA, Uiterwaal CS, Imhof SM, Wisse RPL. Age-specific Incidence and Prevalence of Keratoconus: A Nationwide Registration Study. Am J Ophthalmol. 2017;175:169-172.
- Wollensak G, Spoerl E, Seiler T. Riboflavin/ultraviolet-a-induced collagen crosslinking for the treatment of keratoconus. Am J Ophthalmol. 2003 May;135:620-627.
- Walsh J, Bergmanson JPG. Ocular Visible Light and Ultraviolet Radiation Transmittance. In: Bergmanson JPG, ed. Clinical Ocular Anatomy and Physiology, 30th ed. Houston: Texas Eye Research and Technology Center. 2023:71-75.
- Bergmanson JPG. Cornea. In: Bergmanson JPG, ed. Clinical Ocular Anatomy and Physiology, 30th ed. Houston: Texas Eye Research and Technology Center. 2023:78-115.
- Ehlers N, Sorensen T, Bramsen T, Poulsen EH. Central corneal thickness in newborns and children. Acta Ophthalmol (Copenh). 1976 Jul;54:285-290.
- Autzen T, Bjornstrom L. Central corneal thickness in full-term newborns. Acta Ophthalmol (Copenh). 1989 Dec;67:719-720.
- Portellinha W, Belfort R Jr. Central and peripheral corneal thickness in newborns. Acta Ophthalmol (Copenh). 1991 Apr;69:247-250.
- Sehrawat P, Beri S, Garg R, Datta V, Shandil A. Central corneal thickness and corneal diameter in preterm and term newborns and preterm neonates at term. Indian J Ophthalmol. 2019 Oct;67:1575-1578.
- Doughty MJ, Zaman ML. Human corneal thickness and its impact on intraocular pressure measures: a review and meta-analysis approach. Surv Ophthalmol. 2000 Mar-Apr;44:367-408.
- Duke-Elder S, Wybar KC. The cornea. In: Duke-Elder S, ed. System of ophthalmology. Volume II. The anatomy of the visual system, 2nd ed: Kimpton. 1961:92-131.
- Arffa RC. Dystrophies of the Epithelium, Bowman’s Layer and Stroma. In: Arffa RC, Grayson M, eds. Grayson’s diseases of the cornea, 4th ed. St. Louis: Mosby. 1997:413-464.
- Meyer JJ, Gokul A, Vellara HR, McGhee CNJ. Progression of keratoconus in children and adolescents. Br J Ophthalmol. 2023;107:176-180.
- Sarac O, Caglayan M, Cakmak HB, Cagil N. Factors Influencing Progression of Keratoconus 2 Years After Corneal Collagen Cross-Linking in Pediatric Patients. Cornea. 2016;35:1503-1507.
- Godefrooij DA, Soeters N, Imhof SM, Wisse RP. Corneal Cross-Linking for Pediatric Keratoconus: Long-Term Results. Cornea. 2016 Jul;35:954-958.
- Seiler TG, Seiler T. Corneal cross-linking: History, Physiology and Techniques. In: Izquierdo L, Henriquez MA, Mannis MJ, eds. Keratoconus Diagnosis and Management. Philadelphia: Elsevier. 2023;395-401.
- Raiskup-Wolf F, Hoyer A, Spoerl E, Pillunat LE. Collagen crosslinking with riboflavin and ultraviolet-A light in keratoconus: long-term results. J Cataract Refract Surg. 2008 May;34:796-801.
- Seifert FK, Theuersbacher J, Schwabe D, Lamm O, Hillenkamp J, Kampik D. Long-Term Outcome of Corneal Collagen Crosslinking with Riboflavin and UV-A Irradiation for Keratoconus. Curr Eye Res. 2022 Nov;47:1472-1478.
- Polido J, Dos Xavier Santos Araujo ME, Alexander JG, Cabral T, Ambrósio R Jr., Freitas D. Pediatric Crosslinking: Current Protocols and Approach. Ophthalmol Ther. 2022 Jun;11:983-999.
- Arora R, Gupta D, Goyal JL, Jain P. Results of corneal collagen cross-linking in pediatric patients. J Refract Surg. 2012 Nov;28:759-762.
- Mazzotta C, Traversi C, Baiocchi S, et al. Corneal Collagen Cross-Linking With Riboflavin and Ultraviolet A Light for Pediatric Keratoconus: Ten-Year Results. Cornea. 2018 May;37:560-566.
- Saad S, Saad R, Jouve L, et al. Corneal crosslinking in keratoconus management. J Fr Ophtalmol. 2020 Dec;43:1078-1095.
- Ghanem VC, Ghanem RC, de Oliveira R. Postoperative pain after corneal collagen cross-linking. Cornea. 2013 Jan;32:20-24.
- Glaukos. Photrexa Prescribing Information. Available at accessdata.fda.gov/drugsatfda_docs/label/2016/203324s000lbl.pdf . Accessed May 4, 2023.
- Chatzis N, Hafezi F. Progression of keratoconus and efficacy of pediatric [corrected] corneal collagen cross-linking in children and adolescents. J Refract Surg. 2012 Nov;28:753-758.
- Or L, Rozenberg A, Abulafia A, Avni I, Zadok D. Corneal Cross-Linking in Pediatric Patients: Evaluating Treated and Untreated Eyes-5-Year Follow-Up Results. Cornea. 2018 Aug;37:1013-1017.
- Kollros L, Torres-Netto EA, Rodriguez-Villalobos C, et al. Progressive keratoconus in patients older than 48 years. Cont Lens Anterior Eye. 2023 Apr;46:101792.
- Lattimore MR Jr. Effect of ultraviolet radiation on the energy metabolism of the corneal epithelium of the rabbit. Photochem Photobiol. 1989 Feb;49:175-180.
- Pitts DG, Bergmanson JP, Chu LW. Ultrastructural analysis of corneal exposure to UV radiation. Acta Ophthalmol (Copenh). 1987 Jun;65:263-273.
- Bergmanson JP. Corneal damage in photokeratitis--why is it so painful? Optom Vis Sci. 1990 Jun;67:407-413.
- Maguire MG, Stark WJ, Gottsch JD, et al. Risk factors for corneal graft failure and rejection in the collaborative corneal transplantation studies. Collaborative Corneal Transplantation Studies Research Group. Ophthalmology. 1994 Sep;101:1536-1547.
- Foulks GN. Diagnosis and management of corneal allograft rejection. In: Krachmer JH, Mannis MJ, Holland EJ, eds. Cornea, 3rd ed. Philadelphia: Elsevier/Mosby; 2011:1409-14016.
- Trief D, Marquezan MC, Rapuano CJ, Prescott CR. Pediatric corneal transplants. Curr Opin Ophthalmol. 2017 Sep;28:477-484.
- Perez-Straziota C, Gaster RN, Rabinowitz YS. Corneal Cross-Linking for Pediatric Keratcoconus Review. Cornea. 2018 Jun;37:802-809.
- Wajnsztajn D, Hopkinson CL, Larkin DFP, et al. Keratoplasty for Keratoconus in Young Patients: Demographics, Clinical Features, and Post-transplant Outcomes. Am J Ophthalmol. 2021 Jun;226:68-75.
- Price LD, Larkin DFP. Diagnosis and management of keratoconus in the paediatric age group: a review of current evidence. Eye (Lond). 2023 Jun 6. [Online ahead of print]



