
MUCH OF THE INFORMATION in this article—as with previous annual reports—is obtained from a combination of recent research and polling of both the Contact Lens Spectrum (CLS) readers and experts in the contact lens industry. Recent developments in myopia management, corneal GPs, scleral lenses, and custom soft lenses will be highlighted. In addition, advancements in keratoconus and multifocal contact lenses will be presented.
The GP Lens Institute (GPLI) Advisory Board, consisting of prominent experts in specialty contact lenses, were asked what they believed to be the most important developments in GP and custom soft lenses in the past year. Their top five responses (ranked 1 to 5) are listed here:
- Higher-order aberration (HOA)-correcting optics, wavefront aberrometry, and related quality of vision advancements with scleral lenses.
- High-/hyper-Dk lens materials.
- Customization of scleral lenses to include quadrant-specific, bi-elevation, scan-based free-form designs, and increased profilometry use and applications.
- Increased application of myopia management options, including orthokeratology, soft multifocals, and low-dose atropine.
- Increased custom soft lens options, including soft multifocal lenses with offset optics, and ordering lenses having nonstandard sagittal depth and powers outside of standard ranges.
It is not a surprise that many of these developments pertain to myopia management and scleral lenses, and they will be emphasized in this report.
MYOPIA MANAGEMENT
Interest in integrating one or more methods of myopia management into practice today continues to grow as it is rapidly becoming the standard of care. Additionally, overnight orthokeratology, peripheral-plus-power soft multifocals, and low-dose atropine all effectively slow down myopia progression in young people, either alone or in combination.
When surveyed, the CLS readership indicated that only 27% have not integrated myopia management into their practices. The preferred modality continues to be soft multifocals (60.6%) with overnight orthokeratology next (48.5%), followed by low-dose atropine (43.9%) (Figure 1). Several exceptional comprehensive articles on myopia management have been published and are well worth reading for anyone considering implementing this important—and quality-of-life-improving—modality into clinical practice.1,2

Soft Multifocal Lenses Although this modality—as compared to overnight orthokeratology—requires lens wear during the day, its ease of implementation and initial comfort benefits have resulted in its increased popularity. In addition, recent studies comparing both modalities have found a similar rate of slowing myopia progression3 and no significant difference in axial length growth.3,4 In the latter study, it was concluded that there was little, if any, difference in efficacy between the two modalities. Most recently, the Bifocal Lenses In Nearsighted Kids (BLINK) Study group found that short-term wear of soft multifocal lenses does not negatively affect children’s quality of life.5
Overnight Orthokeratology According to our readership, 61% of eyecare professionals (ECPs) who are actively fitting overnight orthokeratology indicated that they increased their use of this modality in the past year (Figure 2). As with myopia management in general, the understanding of overnight orthokeratology has advanced greatly with recent contributions to the literature. In particular, the British Contact Lens Association (BCLA) Contact Lens Evidence-based Academic Report (CLEAR) white paper—authored by several of the foremost experts in the field—represents a very comprehensive overview.6

One large-scale report, including a total of 655 eyes, concluded that orthokeratology can effectively slow myopia progression versus the various control groups used in the studies, although the efficacy of myopia control did tend to decrease over time.7 A very important finding of this study was that no difference in adverse events was found between orthokeratology and the control groups.
Another report reviewed 37 studies pertaining to the same overnight orthokeratology lens design, finding not only consistently good efficacy in slowing myopia progression, but that when separating out the 10 prospective studies, an average of 91% of the orthokeratology wearers completed the study.8 Consistent with previous research, it has recently been found that reducing the treatment zone—in this case from 6.2mm to 5.0mm—had a significant effect on the efficacy of myopia control.9 It has also been found that overnight orthokeratology does not appear to impact the ocular surface over time.10
The benefits of overnight orthokeratology are not limited to children. It has been found to be effective and—most notably—improve the quality of life when worn by adults.11 When comparing children and adult wearers who were established spectacle, soft contact lens, or orthokeratology wearers, it was concluded that activity-driven adults and children perceived significant benefits of orthokeratology as compared to wearing spectacles.12
GP LENSES
The use of GP lenses continues to be stable in the marketplace. In the recent CLS feature, “International Contact Lens Prescribing in 2022,” it was reported that there were 12% GP lens fits in addition to 1% orthokeratology fits in the U.S.13 As in past years, it was encouraging that a very high percentage (98.4%) of the readership surveyed do fit GP lenses.
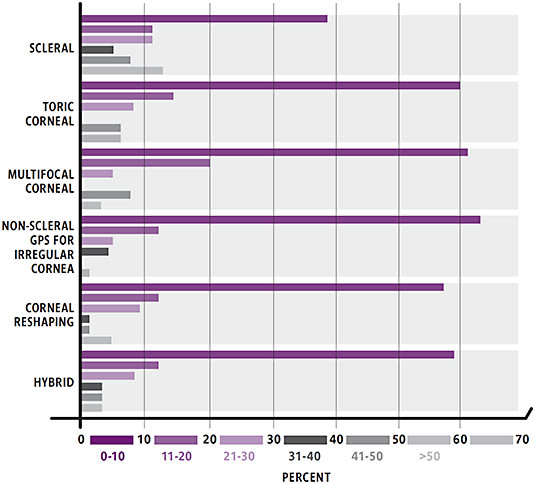
Figure 3 shows the GP fitting trends for six different categories as revealed by the readership survey. When viewing the categories in black (31% to 40% lenses prescribed), dark gray (41% to 50% lenses prescribed), and light gray (> 50% lenses prescribed), scleral lenses are the most common fit modality, followed by toric corneal and multifocal corneal GP lenses.
As in previous years, the CLS readership was asked whether they fit GP lens designs empirically or via the use of diagnostic lenses (Table 1). As would be expected, as a result of today’s manufacturing technology—as well as continuing advances in instrumentation to evaluate the cornea—toric GP lenses, corneal reshaping/orthokeratology, multifocals, and spherical lenses are fit predominantly via empirical means.
| DESIGN | EMPIRICAL | DIAGNOSTIC |
| Toric GP | 77% | 23% |
| Corneal Reshaping | 72% | 28% |
| Multifocal | 68% | 32% |
| Spherical | 56% | 44% |
| Hybrid | 52% | 48% |
| Non-Scleral IC | 37% | 63% |
| Scleral | 19% | 81% |
With empirical-based calculators, hybrids can typically be fit empirically as well. Patients exhibiting irregular corneas, however, often benefit from diagnostic fitting. With advances in profilometry-driven designs, empirical fitting of scleral lenses should increase in the years ahead.
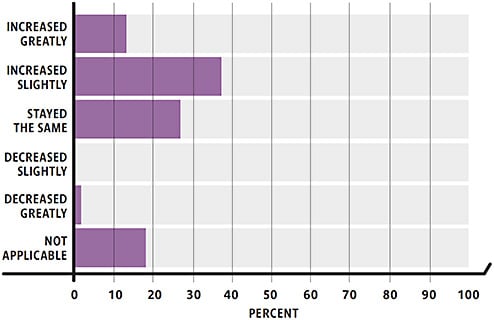
Scleral Lenses According to a recent survey, 21% of rigid lenses used in the U.S. are scleral lenses.14 The readership poll also noted that scleral lens use is increasing. About 20% of the respondents do not fit scleral lenses; only 1.5% reported that scleral use has decreased in their practice over the past year; and approximately 51.5% indicated that it was increasing; and about one in seven respondents reported that it has increased greatly (Figure 4).
In this same survey, the readership was asked about the frequency with which they order their scleral lenses with spherical peripheral curves, toric haptics, and quadrant-specific haptics. Toric haptics were commonly used, with 90% of respondents indicating they were minimally being ordered in 20% of their lenses, and almost half of the respondents minimally ordering toric haptics in 50% of their lenses.
Quadrant-specific haptics are gaining popularity as well. More than 60% of respondents are ordering this very custom scleral design for at least 20% of their patients, which bodes well for achieving an optimum fit and patient success (Table 2). In addition, one in six respondents indicated they are using profilometry in scleral lens fitting, another indicator that an optimum fitting relationship often can be achieved empirically (Table 2).
| 1. What percentage of scleral lenses are ordered with: | 2. Do you use profilometry in scleral lens fitting? | |||
| TYPE | ≥ 20% | ≥ 50% | Yes | 17% |
| Toric Haptics | 91% | 48% | ||
| Quadrant-Specific Haptics | 61% | 33% | No | 83% |
| Spherical Peripheral Curves | 73% | 40% | ||
Studies have shown that the number of experienced scleral lens practitioners is increasing,15 the complication rate is quite low,16 and scleral lenses are the first option for the management of irregular corneas, ahead of corneal GP lenses.17 This result is consistent with the readership poll, which showed that scleral lenses were the “go-to” lens; almost half of the respondents indicated they fitted at least half of their irregular cornea patients into scleral lenses. This was followed by small-diameter corneal GP (16.9%) and larger corneal intralimbal GP lenses (12.1%) or a combined 27% for corneal GPs (Table 3).
| LENS TYPE | ≥ 20% OF PATIENTS | ≥ 50% OF PATIENTS |
| Scleral Lenses | 73% | 48% |
| Small OAD GP | 42% | 17% |
| Intralimbal GP | 36% | 12% |
| Hybrids | 30% | 8% |
| Custom Soft | 27% | 8% |
| Piggyback | 14% | 3% |
Sclerals have proven to be quite successful for pediatric patients who have irregular corneas, including keratoconus, trauma, and post-keratoplasty.18,19 It has been reported recently that reverse piggyback lenses (soft/scleral) are a viable option in addressing poor front-surface wettability issues with scleral lenses, and 12% of active scleral lens fitters have tried this modality.20 This combination has not been found to induce significant edema after short-term wear.21
Keratoconus The development of wavefront-guided designs has been an exciting modality for the GP correction of keratoconus and, as noted earlier, is seen by the GPLI Advisory Board as the biggest advancement in GP lenses in the past year. HOA-correcting optics, placed on the front surface of scleral lenses, resulted in correction of a significant number of HOAs while resulting in improvements in both visual acuity and contrast sensitivity.22
Likewise, GP lenses were found to improve visual performance, especially low-contrast visual acuity in patients after penetrating keratoplasty.23 Hybrid lenses have been found to improve vision in moderate and advanced keratoconus as much as corneal GPs, and both are especially beneficial to individuals exhibiting central cones.24
Multifocals GP multifocals have always represented the best option for offering visual clarity, due to the rigid lens optics, the center-distance design for aspheric lenses, and the ability to have distance optics in front of the eyes for distance tasks and near optics in front of the eyes for near tasks via segmented, translating designs.
In our readership survey, aspheric multifocal lenses were the go-to for 31.2% of respondents (17.2% do not fit this design), as compared to concentric GP multifocals at 13.8% (41.7%), scleral multifocals at 12.3% (42.1%), segmented translating multifocals at 10.2% (39.0%), and hybrid multifocals at 5.2% (60.0%) (Table 4).
| TYPE | ≥ 20% | ≥ 50% | N/A |
| Aspheric Corneal GP | 56% | 31% | 17% |
| Concentric GP | 38% | 14% | 42% |
| Scleral | 35% | 12% | 42% |
| Segmented, Translating GP | 24% | 10% | 39% |
| Hybrid | 21% | 5% | 60% |
CUSTOM SOFT LENSES
There exists a contact lens for anyone who desires or benefits from contact lens wear. Nowhere is this more evident than with custom soft lenses. They are beneficial in three primary groups of individuals: 1) Those having a unique ocular size or shape (steep or flat corneas; large or small corneal diameters); 2) those who have high/out-of-customary range of refractive errors (high-minus or -plus prescriptions; high astigmatism); and 3) those exhibiting irregular astigmatism.25 In addition, they are invaluable and often life-changing for individuals in need of custom-tinted/prosthetic soft lenses.
It has recently been found that patients are willing to pay for a toric correction (versus spherical) to achieve the vision benefits.26 Therefore, cost should not be a factor precluding one from the use of a custom soft toric or other form of custom soft lens. Soft toric lenses are available in lens parameters well beyond the standard –2.25D cylinder maximum and 10˚ axes, often available in as much as 10D of cylinder correction in 1˚ axis steps.
According to the CLS readership survey, standard soft toric contact lenses are easily the lens modality of choice for the high (≥ 2D) refractive astigmat; in the 2024 survey, this value will increase, and it will be interesting to see whether custom soft torics will fare better (Table 5). An increasing number of toric multifocal lens designs are also becoming available, many in a silicone hydrogel lens material. These are often replaced quarterly, and some laboratories will provide a trial lens in the predicted parameters for assessment of fit and vision.
| TYPE | ≥ 20% | ≥ 50% |
| Standard Soft Toric | 87% | 56% |
| Custom Soft Toric | 59% | 23% |
| Spherical GP | 48% | 17% |
| Toric GP | 46% | 9% |
Once again, when asked which modality the readership prefers for the astigmatic presbyope, the standard soft contact lens (i.e., multifocal) again prevailed, but toric multifocals showed a large increase compared to the 2022 survey (Table 6).
| TYPE | ≥ 20% | ≥ 50% |
| Spherical Soft Multifocal | 56% | 30% |
| Custom Soft Multifocal | 37% | 19% |
| Aspheric GP | 49% | 15% |
| Hybrid Multifocal | 26% | 9% |
| Translating, Segmented GP | 21% | 7% |
There has also been an increased interest in the soft lens management of keratoconus and other irregular cornea patients. There are an increasing number of lathe-cut custom soft lenses for irregular cornea patients.27 Many of these designs are available in a silicone-hydrogel lens material—an important consideration due to the greater center thicknesses used in these designs—and most are available in toric parameters.
What does the future hold for custom soft lenses? Certainly, new latheable soft lens materials are on the horizon. In addition, much new information has emphasized how important sagittal depth is when fitting soft lenses.28,29 Studies have found that 23.3% of corneal diameters fall outside of the normal values (i.e., ≥ 0.5mm smaller than or greater than the average diameter of 11.8mm).28 The sagittal depth tends to vary between lenses as well, sometimes quite significantly.29 Thus, custom soft lenses, even in spherical prescriptions, have definite applications. With today’s technology, the use of corneal scleral topography helps determine sagittal height, which can then be beneficial in designing a custom soft lens.30
THE FUTURE OF CONTACT LENSES
The future of contact lenses is very exciting. Representative findings from surveys sent to both the GPLI Advisory Board and cornea and contact lens residents from 1999 to 2023 are provided in Table 7. Obviously, HOA correction will become more commonplace, notably with—but not limited to—scleral lens designs. Free-form designs with wavefront optics should be readily adopted.
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Three-dimensional (3D) printing and artificial intelligence (AI) are especially exciting, and it will be fascinating to see new applications for them in the near future. While 3D printing still has some limitations, it will potentially allow patients to receive their specialty lenses much more quickly and eliminate the need for practitioners to maintain multiple units in stock and long-term storage.31
It will be interesting to see what new developments will occur in myopia management. New soft lenses continue to be developed and show promise.32 Orthokeratology lens designs—a growing segment of GP contact lens manufacture—are now being embraced by some of the major soft lens companies, which will probably result in a growing GP market. Likewise, atropine-eluting contact lenses show promise in slowing down myopia progression.33 And speaking of drug-eluting contact lenses, not only should these be available to assist our allergy sufferers, but lenses to help with the management of dry eye, glaucoma, and the monitoring of blood sugar should be available in the not-too-distant future.
Other advancements to come should include improved GP and soft contact lens materials, improved instrumentation to measure scleral profile, and better anterior segment optical coherence tomography (AS-OCT) to optimize scleral contact lens success. Along these lines, it has been found that corneal GP lens software for keratoconus that is built into AS-OCT may be useful in determining an accurate contact lens prescription.34
Contact lenses continue to represent an exciting and ever-changing area of eyecare practice. With the innovations in technology, lens designs, and materials, the applications for GP and custom soft lenses will continue to change the lives of our patients. CLS
Acknowledgments: Roxanne Achong-Coan, OD; Melissa Barnett, OD; Edward Boshnick, OD; Mile Brujic, OD; Karen Carrasquillo, OD; Carmen Castellano, OD; Gloria Chiu, OD; Brian Chou, OD; Greg DeNaeyer, OD; Barry Eiden, OD; Robert Ensley, OD; Daddi Fadel, DOptom; Jennifer Fogt, OD; John Gelles, OD; Alan Glazier, OD; Katie Greiner, OD; Robert Grohe, OD; Susan Gromacki, OD, MS; Elise Kramer, OD; Langis Michaud, OD, MSc; Marcus Noyes, OD; Thomas Quinn, OD, MS; Pam Satjawatcharaphong, OD; Louise Sclafani, OD; David Seibel, OD; Joseph Shovlin, OD; and Jeff Walline, OD, PhD.
References
- Sankaridurg P, Berntsen DA, Bullimore MA, et al. IMI 2023 Digest. Invest Ophthalmol Vis Sci. 2023 May;64:7.
- Lanca C, Repka MX, Grzybowski A. Topical review: Studies on management of myopia progression from 2019-2021. Optom Vis Sci. 2023 Jan 1;100:23-30.
- Fang JMM, Huang Z, Long Y, et al. Retardation of myopia by multifocal soft contact lens and orthokeratology: A 1-year randomized clinical trial. Eye Contact Lens. 2022 Aug 1;48:328-334.
- Skidmore KV, Tomiyama ES, Rickert ME, Richdale K, Kollbaum P. Retrospective review of the effectiveness of orthokeratology versus soft peripheral defocus contact lenses for myopia management in an academic setting. Ophthalmic Physiol Opt. 2023 May;43:534-543.
- Ticak A, Walline JJ, Berntsen DA, et al; BLINK Study Group. Quality of life after wearing multifocal contact lenses for myopia control for 2 weeks in the BLINK Study. Ophthalmic Physiol Opt. 2023 Aug 23. [Online ahead of print]
- Vincent SJ, Cho P, Chan KY, et al. BCLA CLEAR – Orthokeratology. 2021 Apr;44:240-269.
- Tang K, Si J, Wang X, Lu X, Bi H. Orthokeratology for Slowing Myopia Progression in Children: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Eye Contact Lens. 2023 Sep 1;49:404-410.
- Bullimore MA, Liu M. Efficacy of the Euclid orthokeratology lens in slowing axial elongation. Cont Lens Anterior Eye. 2023 Jun 24:101875. [Online ahead of print]
- Li N, Lin W, Zhang K, et al. The effect of back optic zone diameter on relative corneal refractive power distribution and corneal higher-order aberrations in orthokeratology. Cont Lens Anterior Eye. 2023 Feb:46:101755.
- Ruan J, Zhang Y, Chen Y. Influence of overnight orthokeratology on tear film and meibomian glands in myopic children: a prospective study. BMC Ophthalmol. 2023 Apr 3;23:136.
- Ren Q, Yang B, Liu L, Cho P. Orthokeratology in adults and effect on quality of life. Cont Lens Anterior Eye. 2023 June;46:101824.
- Lattery LJ, Chao C, Walline JJ, et al. Parent and patient perceptions of myopia modalities. Cont Lens Anterior Eye. 2023 April;46:101772.
- Morgan PB, Woods CA, Tranoudis IG, et al. International Contact Lens Prescribing in 2022. Contact Lens Spectrum. 2023 Jan;38:28-35. Available at clspectrum.com/issues/2023/january-2023/international-contact-lens-prescribing-in-2022 . Accessed Aug. 29, 2023.
- Nichols JJ, Fisher D. Contact Lenses 2022. Contact Lens Spectrum. 2023 Jan;38:20-26. Available at clspectrum.com/issues/2023/january-2023/contact-lenses-2022 . Accessed Aug. 29, 2023.
- Nau CB, Harthan JS, Shorter ES, et al. Trends in Scleral Lens Fitting Practices: 2020 Scleral Lenses in Current Ophthalmic Practice Evaluation Survey. Eye Contact Lens. 2023 Feb 1;49:51-55.
- Schornack MM, Nau C, Harthan J, Shorter E, Nau A, Fogt J. Survey-based Estimation of Corneal Complications Associated with Scleral Lens Wear. Eye Contact Lens. 2023 Mar 1;49:89-91.
- Shorter E, Fogt J, Nau C, Harthan J, Nau A, Schornack M. Prescription Habits of Scleral Lenses for the Management of Corneal Irregularity and Ocular Surface Disease Among Scleral Lens Practitioners. Eye Contact Lens. 2023 Feb 1;49:46-50.
- Walker MK, Bergmanson JPG, Schornack M, Fadel D. IFSLR 2023 Recap. Contact Lens Spectrum. 2023 Sept;38:37-41. Available at clspectrum.com/issues/2023/september-2023/ifslr-2023-recap . Accessed Sept. 1, 2023.
- Severinsky B, Lenhart P. Scleral contact lenses in the pediatric population—Indications and outcomes. Cont Lens Ant Eye. 2022 Jun;45:101452.
- Contact Lenses Today. 2023 June 25. Available at clspectrum.com/newsletters/contact-lenses-today/june-25,-2023 . Accessed Aug. 29, 2023.
- Bliss VH, Branjerdporn N, Ooi PJ, et al. Corneal oedema during reverse piggyback scleral lens wear. Ophthalmic Physiol Opt. 2023 Sep;43:1065-1069.
- Badrinarayanan A, Balakrishnan AC, Dutta R, Kumar RM, Iqbal A. Impact of Scleral Lens Front Surface Eccentricity on Visual Acuity, Contrast Sensitivity, and Higher-Order Aberrations in Eyes with Keratoconus. Eye Contact Lens. 2023 Sep 1;49:374-378.
- Zhang J, Lin X, Wang X, et al. Investigation of contrast visual acuity with rigid gas permeable contact lenses after penetrating keratoplasty. BMC Ophthalmol. 2023 Jan 9;23:12.
- Taşcı YY, Saraç O, Çağıl N, Yeşilırmak N. Comparison of Hybrid Contact Lenses and Rigid Gas-Permeable Contact Lenses in Moderate and Advanced Keratoconus. Turk J Ophthalmol. 2023 Jun;53:142-148.
- Andrzejewski T, Harthan J. Custom Soft Lenses 2023. Contact Lens Spectrum. In Press.
- Morgan OA, Mirza AA, Parmar KR, et al. Clinical performance and willingness to pay for soft toric contact lenses in low and moderate astigmats. Cont Lens Anterior Eye. 2023 Jul 15;101887.
- Tyler’s Quarterly Soft Contact Lens Parameter Guide. 2023 Mar;40:19.
- van der Worp E, Lampa M, Kinoshita B, Fujimoto MJ, Coldrick BJ, Caroline P. Variation in sag values in daily disposable, reusable and toric soft contact lenses. Cont Lens Anterior Eye. 2021 Dec;44:101386.
- van der Worp. Pacific University SCL Sagittal Depth Story. 2021. Available at commons.pacificu.edu/work/ns/380b99ad-5f0b-4e77-a286-a8d1f74bdfe9 . Accessed Aug. 29, 2023.
- Viñuela JR, Piñero DP, Martínez MB. Comparing sagittal heights calculated using corneal parameters and those measured with profilometry. Cont Lens Anterior Eye. 2022 Aug 22;101747.
- Phan CM. 3D Printing of Specialty Contact Lenses. Contact Lens Spectrum. 2023 Aug;38:43. Available at clspectrum.com/issues/2023/august-2023/fast-forward-to-the-future . Accessed Aug. 29, 2023.
- Cheng X, Xu J, Brennan NA. Randomized trial of soft contact lenses with novel ring focus for controlling myopia progression. Ophthalmol Sci. 2023 Oct 18;3:1-10.
- Fu Y, Luo Y, Chen X, Tong Y, Zhu Y, Yang L. Atropine-eluting silicone contact lenses for myopia control. J Biomater Appl. 2023 May;37:1724-1735.
- Itoi M, Itoi M, Harigaya A, Ishigaki K, Satou R, Ueda E. Cornea RGP contact lens fitting software for keratoconus built-in anterior segment optical coherence topography. Eye Contact Lens. 2022 Dec 1;48:503-508.



