
SPECIALTY LENS OPTIONS provide opportunities to improve visual outcomes for various corneal and ocular surface conditions. That having been said, our specialty lens patients and their conditions do not exist on an island but are influenced by various factors. Thus, it is incumbent on practitioners to assess these individuals’ unique needs and assure them that we are doing all we can to optimize clinical outcomes.

This will often involve not only the lenses that we prescribe for our patients but also the use of other therapeutics to maximize their outcomes. Here, we present several factors that can negatively impact optimal contact lens wear plus information on how to overcome these challenges by recruiting targeted pharmaceutical intervention when appropriate.
LID POSITION
Good lid position is necessary to optimize vision. Ptosis can alter the level of light entering the pupil and, in doing so, can have consequences for a patient’s vision.1 Until recently, the only treatment option for ptosis was surgery.1 This raises the lid position, allowing more light into the eye unhindered by the upper lid.
Recently, a pharmaceutical agent has been approved to treat age-related blepharoptosis. The active ingredient is 0.1% oxymetazoline, and it is approved to be used once a day for acquired ptosis.2 Oxymetazoline is an alpha-adrenergic agonist. It has a fivefold greater efficacy for alpha-2 receptors over alpha-1 receptors.3 Thus, it selectively activates alpha-adrenergic receptors in Mueller’s muscle.4
Mueller’s muscle is partially responsible for holding the lid at an appropriate position, so that the lid margin and lashes are not hindering the superior pupil.1 Clinical trials demonstrated both an elevated upper eyelid position and improvement in superior visual field when patients using 0.1% oxymetazoline were compared with patients utilizing a placebo.5,6
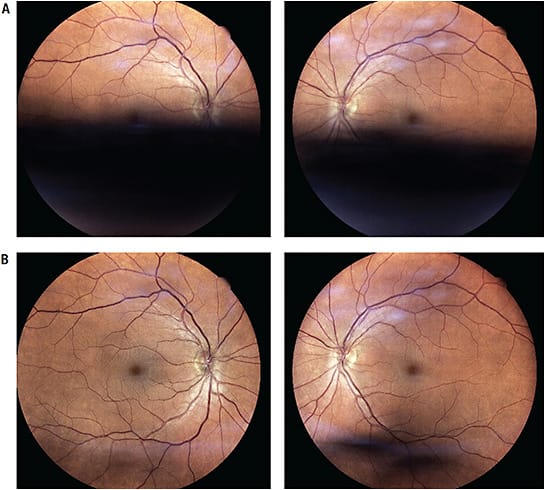
A recent poster at SECO 2023 examined individuals’ confocal scanning laser images of the retina with ptosis before instillation of 0.1% oxymetazoline and after instillation of the drop.7 The inferior retinal image with confocal scanning laser imaging is acquired from the superior pupil. Thus, any obstruction of the inferior retina is likely due to a ptotic lid blocking the image acquisition (Figure 1). This demonstrates clinically the effect on the vision and visual field that ptosis can have.
Lid position is important to consider with our specialty lens wearers. Often, these are patients who have severely compromised corneas through irregular ocular surfaces or severe dryness; thus, it is critical to optimize light entrance into the eye. Fortunately, a scleral lens, which is often the treatment of choice for these patients, can also help increase the position of the upper eyelid (Figure 2).

Soft multifocal contact lenses provide a unique opportunity to provide patients with both distance and near vision correction through simultaneous vision. As the optical zone of the lens is divided into both distance and near optics, it reduces the quality of the optical signal compared with a single vision lens at each distance.8 Unfortunately, if patients have ptosis that is severe enough to impede some of the pupil, this may further reduce the quality of the optical image. Therefore, it is critical to take eyelid position into consideration when fitting these patients with contact lenses.
• Case Example A 60-year-old female came in for a comprehensive eye examination. She was a hyperopic presbyope wearing soft multifocal daily disposable contact lenses. She had noticed that her vision through her contact lenses started getting weaker and felt that she might need a stronger prescription in her contact lenses, especially for reading. Her medical history was unremarkable. Her examination revealed moderate ptosis OD and OS (Figure 3).

When her eyelids were lifted, she immediately experienced better vision at both distance and near. Although her visual acuity was the same, her impression of her vision was much better. We removed her lenses and placed a drop of 0.1% oxymetazoline in each eye. Fifteen minutes later, the lenses were placed back on her eyes with a substantial improvement in her subjective vision.
DRY EYE
Over the last decade, there has been a substantial evolution of both dry eye diagnostics and therapeutics. Practitioners now have the ability to understand the underlying cause of dry eye and also be much more targeted with our treatments based on the etiology of the condition.
That having been said, eyecare providers need to be highly cognizant of the health of the ocular surface of patients for whom they care, including specialty lens wearers. One of the strategies to optimize the experience of a patient wearing GP lenses is to apply a polyethylene glycol (PEG) polymer mixture to the lens surface. This renders the surface more hydrophilic and thus improves its wettability. A randomized crossover clinical trial demonstrated improvements in lens comfort, dry eye symptoms, lid wiper epitheliopathy, tear breakup time (TBUT), and comfortable lens wear time in scleral lens wearers with the PEG polymer applied to their lenses compared with untreated lenses.9
It is critical to understand the dynamics of the ocular surface in order to optimize the patient’s wearing experience. Someone who has dry eye will have difficulty wearing contact lenses comfortably, in part because of the lack of a stable tear film.10 Understanding this and optimizing the function of the ocular surface will improve the patient’s lens wear.
• Case Example A 67-year-old female came into the office for a complete eye examination as a new patient. She wanted to update her glasses. She had had radial keratotomy (RK) about 30 years ago. She felt that her vision had become worse at both distance and near through glasses and that her vision sometimes fluctuated throughout the day. Her best-corrected visual acuity was 20/40 OD and 20/50 OS with a moderate hyperopic and astigmatic correction. She also reported using artificial tears three or four times a day.
Anterior segment examination was remarkable for moderate meibomian gland dysfunction (MGD) OD and OS and a low TBUT of three seconds OD, two seconds OS. Both corneas had prominent RK scars and +2 corneal staining inferiorly. Mild cataracts were observed in each eye. Topographies demonstrated irregular corneas OD and OS. Anterior segment optical coherence tomography (AS-OCT) demonstrated irregular corneal epithelial thickness (Figure 4). Retinal health was unremarkable. Cytokine testing was positive OD and OS and Standard Patient Evaluation of Eye Dryness (SPEED) questionnaire was scored at 20.

Options for vision correction were discussed, and we proceeded to fit her with scleral lenses coated in a PEG coating to optimize comfort with the lenses. As we were waiting for her lenses to arrive, the patient started on 0.5% loteprednol q.i.d. OD and OS and cyclosporine 0.09% b.i.d. OD and OS, in addition to warm compresses b.i.d. for 10 minutes. I had her use this regimen until she was evaluated at lens dispensing.
At an office visit two weeks later, she picked up the lenses that had been ordered. At that visit, her TBUT had improved to six seconds OD and OS, there was trace corneal staining inferiorly OD and OS, and the cytokine findings were negative OD and OS. Her SPEED score was 10.
The lenses that were ordered fit well and they were dispensed. We tapered the loteprednol drop to b.i.d. for five days and then q.d. for five days prior to discontinuing the drops. She continued with 0.09% cyclosporine b.i.d. and the warm compress b.i.d., both in each eye.
She was evaluated again two weeks later for a scleral lens and dry eye follow-up. She was compliant with 0.09% cyclosporine b.i.d. and warm compresses. She was doing exceptionally well with applying and removing her scleral lenses along with cleaning and disinfecting them. She is continuing with her current treatment regimen, and she returned three months later for an advanced meibomian gland warming and evacuation procedure. She has been successfully wearing her scleral lenses ever since.
PUPIL SIZE
Pupil size can significantly alter the quality of a patient’s vision. In general, practitioners know that reducing the size of the pupil decreases the size of blur circles and extends a patient’s depth of focus. Additionally, large pupils can alter a patient’s visual system. Conversely, increasing the pupil size will reduce the depth of focus11,12 and may also exacerbate higher-order aberrations.
There is a simple test to perform in the examination room to determine whether a patient’s pupil size may be the reason that their visual quality is reduced. Simply cover one eye in a dark examination room and, while the patient is looking at a line on the eye chart, shine a bright light in the patient’s non-viewing eye. This will consensually constrict the pupil of the viewing eye. If the patient reports improved vision, they may benefit from controlling the pupil size. Pupil dilation can create a discrepancy in visual quality between well-lit and dimly lit environments.
Fortunately, we have pharmaceutical means of reducing pupil size. Brimonidine is an alpha-2 adrenergic agonist that acts on the alpha-2 receptor on the presynaptic nerve ending of the dilator muscle. Thus, it reduces norepinephrine in synaptic cleft and reduces the activity of the dilator muscle, preventing pupil dilation in low light levels.13,14 This is an important strategy and should be considered for patients who have reduced vision under low-light-level conditions.
• Case Example A 50-year-old male who has keratoconus and who was successfully wearing corneal GP lenses for keratoconus presented for his yearly comprehensive eye examination. He reported that the vision and comfort were great with the lenses. The only complaint he had was that his vision could be better in the evening.
His vision with his GP lenses was 20/20 OD and OS. When all lights were off in the examination room, he commented on the reduced visual quality. When one eye was covered, and a transilluminator was shone in the covered eye, the vision with the viewing eye immediately improved. The patient’s pupil was dilating beyond the edge of the optical zone of the lens, causing the visual issues under low light levels.
We discussed the challenge with the patient and discussed options of increasing the size of the lens, considering a scleral lens, or providing pupillary modulation with a pharmaceutical agent, as needed. The patient wanted to try to initially increase the size of the lens, which we did. He did note an improvement in vision but was still noticing a reduction in visual quality in the evening.
We then prescribed brimonidine 0.1% to use 1 gtt 15 minutes prior to critical viewing tasks in low light levels. We followed up with the patient a week later, and he noted significantly improved vision in low light levels after using the drops.
• Case Example A 35-year-old female successfully wears orthokeratology lenses to correct her myopia. She came in for her yearly comprehensive examination and noted that driving at night was difficult. The reason was pupil dilation, which allowed light passing through the peripheral treatment zone optics to enter the pupil under low light conditions.
We initially increased the size of the treatment zone, which improved the patient’s vision, but she was still hoping to see better. Once we were at the maximum, we could increase the size of the treatment zone; we also discussed pharmaceuticals, specifically brimonidine. The patient elected to proceed with pharmaceutical treatment.
The patient was a light-eyed individual. We recommended trying brimonidine 0.025% to use 15 minutes prior to night driving. Brimonidine at this concentration is available over the counter and is easily accessible. We followed up with the patient one week later, and she reported a significant improvement in vision under low light levels.
THE ALLERGIC INFLUENCE
Allergic eye disease can be detrimental to the contact lens wearer. This applies not only to the specialty lens wearer but also for those who wear lenses for vision correction as an alternative to glasses.
Several forms of allergic eye disease can affect the eye. Seasonal and perennial conjunctivitis are cases of type 1 hypersensitivity that are histamine-driven.15 Other chronic forms of allergic disease include vernal keratoconjunctivitis, atopic keratoconjunctivitis, and giant papillary conjunctivitis.16,17 Sensitivities can also develop to preservatives present in therapeutics, disinfectants, eye drops, and contact lens solutions.
Fortunately, many treatments exist. Several antihistamines are available to treat type 1 hypersensitivity responses, including olopatadine, ketotifen, azelastine, cetirizine, bepotastine, and alcaftadine.18-27 Topical corticosteroids are available for more chronic and/or aggressive forms of hypersensitivity responses.28
Ultimately, daily disposable lenses provide a viable option for patients who have hypersensitivities, as the lenses are new every day.29 Unfortunately, some patients are not candidates for daily disposable lenses, in particular those requiring specialty lenses. Thus, it is critical to understand the solutions that patients are using for their lenses.
In addition to multipurpose disinfecting solutions, make sure to consider peroxide-based disinfecting systems for specialty lens wearers, including GP lenses. It is critical to understand the impact that allergic eye disease can have on your patients. Additionally, practitioners should learn how to ultimately leverage the appropriate strategies to optimize outcomes for patients through appropriate use of pharmaceuticals.
• Case Example A 32-year-old male was successfully fit with scleral lenses for keratoconus. Three months later, he came in for a follow-up visit. At that time, he let me know that his vision was great with the contact lenses, but he felt that recently the vision seemed to be clouding up during the day. He had tried using contact lens rewetting drops, but they didn’t seem to help with the clouding.
On examination, visible clouding of the post-lens tear reservoir was evident. The landing zone of the lenses was well aligned, there was adequate limbal clearance, and central clearance was 250µm OD and OS. The patient was currently using a one-step multipurpose disinfecting solution. The patient also reported having allergies and was taking an oral antihistamine.
Anterior segment assessment revealed +1 diffuse hyperemia OD and OS with a mild papillary response on the palpebral conjunctiva. The patient did report some symptoms of itching as well. Upon closer inspection, the patient also had floppy eyelid syndrome. When asked about sleep apnea, he admitted that he did have sleep apnea and used a continuous airway pressure (C-PAP) unit at night.
The patient was started on olopatadine 0.7% eye drops q.a.m. OD and OS 15 minutes prior to placing scleral lenses on eye. We also had him start using a peroxide-based disinfecting solution to store and disinfect the lenses. Additionally, we prescribed loteprednol etabonate 0.5% ointment that we had the patient apply to his eyes in the evening for seven days.
The patient was seen one week later for a follow-up visit with complete resolution of fogging. He continues to use the peroxide disinfecting solution along with olopatadine 0.7% eye drops in the morning prior to lens application.
PRESBYOPIC ADVANCEMENTS
Traditional means of correcting presbyopia are being supplemented with pharmaceutical agents to enhance near vision by reducing the pupil size and increasing the depth of focus for patients. Currently one therapeutic is available, pilocarpine 1.25%, in a vehicle that quickly neutralizes the pH of the drop when it contacts the eye.30 Pilocarpine is a muscarinic agonist that reduces the size of the pupil, creating an extended depth of focus and improvement in near vision for presbyopes.31
Several other companies are studying other molecules for pupil constriction in order to improve near vision. Some include low-dose pilocarpine, aceclidine, and carbachol. Supplementary molecules that act on the dilator muscle include brimonidine and phentolamine, which are used in combination with cholingeric agonists to cause pupil constriction.32-35 These pharmaceuticals can be leveraged to provide our specialty lens wearers with improved near vision and may be a consideration if multifocal lenses are not an option.
• Case Example A 48-year-old who had a history of penetrating keratoplasty OD and OS called into the office for an emergency triage; he was concerned that his corneal grafts may be failing. He had been wearing scleral lenses successfully for several years.
When he came into the office, AS-OCT measurements indicated appropriate fitting characteristics with respect to the central clearance, limbal clearance, and landing zone characteristics. The patient’s distance visual acuity with the scleral lenses was 20/20 OD and OS. His near visual acuity was 20/60 OU. When asked about vision, he stated that the distance vision seemed to be good, but the near vision seemed to have become significantly weaker.
A distance over-refraction over the scleral lenses resulted in plano OD and OS. The near add was measured at +1.50D, achieving a near vision of 20/20 OU. We explained that presbyopia was the reason for his symptoms, and that it is a normal process. We discussed the options with him, including multifocal lenses, monovision, glasses over his contact lenses as needed, and pilocarpine 1.25% drops placed in the eyes 15 minutes prior to lens application.
The patient is extremely happy with his distance vision and would prefer not to alter the lenses. He was open to wearing glasses over his lenses as needed but was interested in trying the eye drop. He wanted to know what to do when the drops wore off, and I let him know that he would simply revert back to his glasses at that time.
I prescribed 1.25% pilocarpine for the patient to use 1 gtt q.a.m. 15 minutes prior to applying lenses to his eyes and followed up with him two weeks later. At that time, he was happy with the performance of the drops. He did note that some days he seemed to get more sustained benefit than on other days.
CONCLUSION
Specialty lenses have progressed tremendously over the last decade, providing us with new ways to help our patients. Pharmaceuticals have also advanced tremendously. Understanding the benefits of both and how to utilize them synergistically will ultimately provide patients with the best clinical outcomes. CLS
References
- Finsterer J. Ptosis: causes, presentation, and management. Aesthetic Plast Surg. 2003 May-Jun;27:193-204.
- Wirta DL, Korenfeld MS, Foster S, et al. Safety of Once-Daily Oxymetazoline HCl Ophthalmic Solution, 0.1% in Patients with Acquired Blepharoptosis: Results from Four Randomized, Double-Masked Clinical Trials. Clin Ophthalmol. 2021 Oct 8;15:4035-4048.
- Hosten LO, Snyder C. Over-the-Counter Ocular Decongestants in the United States — Mechanisms of Action and Clinical Utility for Management of Ocular Redness. Clin Optom (Auckl). 2020 Jul;12:95-105.
- RVL Pharmaceuticals Inc. Upneeq (oxymetazoline hydrochloride ophthalmic solution), 0.1%, Prescribing Information. 2020. Available at ecp.upneeq.com/wp-content/uploads/2022/10/Upneeq-PI-IFU.pdf . Accessed July 20, 2023.
- Shoji MK, Markatia Z, Ameli K, et al. The effects of topical oxymetazoline on eyelid position, eye redness, and patient-reported eye appearance: A randomized controlled trial. J Plast Reconstr Aesthet Surg. 2023 May;80:66-74.
- Slonim CB, Foster S, Jaros M, et al. Association of Oxymetazoline Hydrochloride, 0.1%, Solution Administration With Visual Field in Acquired Ptosis: A Pooled Analysis of 2 Randomized Clinical Trials. JAMA Ophthalmol. 2020 Nov;138:1168-1175.
- Remon L, Perez-Merino P, Macedo-de-Araujo RJ, Amorim-de-Sousa AI, González-Méijome JM. Bifocal and Multifocal Contact Lenses for Presbyopia and Myopia Control. J Ophthalmol. 2020 Mar 27;2020:8067657.
- Brujic M. Use of confocal scanning retinal imaging to identify visual field limitations and evaluate effects of oxymetazoline hydrochloride ophthalmic solution, 0.1% treatment in adult patients with acquired ptosis. Presented at SECO, Atlanta. February 2023. Available at seco2023posters.s3.amazonaws.com/brujic_confocal/index.html . Accessed July 20, 2023.
- Mickles CV, Harthan JS, Barnett M. Assessment of a Novel Lens Surface Treatment for Scleral Lens Wearers With Dry Eye. Eye Contact Lens. 2021 May 1;47:308-313.
- Koh S. Contact Lens Wear and Dry Eye: Beyond the Known. Asia Pac J Ophthalmol (Phila). 2020 Dec;9:498-504.
- Wolffsohn JS, Davies LN. Presbyopia: Effectiveness of correction strategies. Prog Retin Eye Res. 2019 Jan;68:124-143.
- Schwiegerling J, Gu X, Hong X, Lemp-Hull J, Merchea M. Optical Principles of Extended Depth of Focus IOLs. 2020 Aug. Available at us.alconscience.com/sites/g/files/rbvwei1736/files/pdf/Optical-Principles-of-EDOF-US-CAT-2000006.pdf . Accessed July 20, 2023.
- Marx-Gross S, Krummenauer F, Dick HB, Pfeiffer N. Brimonidine versus dapiprazole: Influence on pupil size at various illumination levels. J Cataract Refract Surg. 2005 Jul;31:1372-1376.
- Kato COS, Shimizu K, Kamiya K, Ishikawa H, Igarashi A. Effects of brimonidine tartrate 0.1% ophthalmic solution on the pupil, refraction, and light reflex. Sci Rep. 2018 Jun 13;8:9003.
- Bonini S. Allergy and the eye. Chem Immunol Allergy. 2014;100:105-108.
- Kenny SE, Tye CB, Johnson DA, Kheirkhah A. Giant papillary conjunctivitis: A review. Ocul Surf. 2020 Jul;18:396-402.
- Singhal D, Sahay P, Maharana PK, Raj N, Sharma N, Titiyal JS. Vernal Keratoconjunctivitis. Surv Ophthalmol. 2019 May-Jun;64:289-311.
- Alcon Inc. Pataday. 2022 Available at pataday.myalcon.com . Accessed July 20, 2023.
- Leonardi A, Quintieri L. Olopatadine: a drug for allergic conjunctivitis targeting the mast cell. Expert Opin Pharmacother. 2010 Apr;11:969-981.
- Namdar R, Valdez C. Alcaftadine: a topical antihistamine for use in allergic conjunctivitis. Drugs Today (Barc). 2011 Dec;47:883-890.
- AbbVie. Lastacaft. 2022. Available at lastacaft.com . Accessed July 20, 2023.
- Alcon Inc. Systane Zaditor Antihistamine Eye Drops. 2020 Available at systane.myalcon.com/products/systane-zaditor-antihistamine . Accessed July 20, 2023.
- Bausch & Lomb Inc. Alaway Preservative Free antihistamine eye drops. 2023. Available at alaway.com . Accessed July 20, 2023.
- Meloto CB, Ingelmo P, Perez EV, et al. Mast cell stabilizer ketotifen fumarate reverses inflammatory but not neuropathic-induced mechanical pain in mice. Pain Rep. 2021 Jun 3;6:e902.
- Abelson MB, Chapin MJ, Kapik BM, Shams NB. Efficacy of ketotifen fumarate 0.025% ophthalmic solution compared with placebo in the conjunctival allergen challenge model. Arch Ophthalmol. 2003 May;121:626-630.
- Eyevance Pharmaceuticals LLC. Zerviate (cetirizine ophthalmic solution) 0.24%. 2023. Available at myzerviate.com . Accessed July 20, 2023.
- Malhotra RP, Meier E, Torkildsen G, Gomes PJ, Jasek MC. Safety of cetirizine ophthalmic solution 0.24% for the treatment of allergic conjunctivitis in adult and pediatric subjects. Clin Ophthalmol. 2019 Feb 19;13:403-413.
- Bielory BP, Perez VL, Bielory L. Treatment of seasonal allergic conjunctivitis with ophthalmic corticosteroids: in search of the perfect ocular corticosteroids in the treatment of allergic conjunctivitis. Curr Opin Allergy Clin Immunol. 2010 Oct;10(5):469-477.
- Hayes VY, Schnider CM, Veys J. An evaluation of 1-day disposable contact lens wear in a population of allergy sufferers. Cont Lens Anterior Eye. 2003 Jun;26:85-93.
- Meghpara BB, Lee JK, Rapuano CJ, Mian SI, Ho AC. Pilocarpine 1.25% and the changing landscape of presbyopia treatment. Curr Opin Ophthalmol. 2022 Jul 1;33:269-274.
- Grzybowski A, Ruamviboonsuk V. Pharmacological Treatment in Presbyopia. J Clin Med. 2022 Mar 3;11:1385.
- Orasis Pharmaceuticals, Inc. CSF-1 Overview. Available at orasis-pharma.com/our-solution/csf-1-overview . Accessed July 20, 2023.
- Visus Therapeutics. Available at visustx.com . Accessed July 20, 2023.
- LENZ Therapeutics. Available at lenz-tx.com . Accessed July 20, 2023.
- Ocuphire Pharma. Available at ocuphire.com . Accessed July 20, 2023.



